Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
![]() Access video lecture content for this chapter online at Elsevier eBooks+
Access video lecture content for this chapter online at Elsevier eBooks+
The eyelids are one of the first areas on the face to show signs of aging. They undergo a predictable pattern of anatomical changes, typically producing a tired appearance, and may also develop functional issues such as eyelid malposition. Optimal periocular rejuvenation with blepharoplasty necessitates not only addressing aesthetic and functional concerns of the eyelids, but also those of the eyebrow and midface. In 2020 there were 325,112 blepharoplasties performed in the US, making blepharoplasty one of the most commonly performed aesthetic procedures in the United States. Eighty five percent (85%) of these procedures were performed in women and were mostly performed in patients 40 years and older (91%).
Given the commonality of this procedure and the global tendency for younger and younger patients to be undergoing plastic surgery, secondary blepharoplasties are being performed with increasing frequency and present a unique challenge for the plastic surgeon with the most common indication for secondary blepharoplasty being lid malposition of the upper eyelid. Most lid malpositioning resolves within 4–6 weeks; when malposition does not affect the cornea, correction should not occur until this window of time has passed as spontaneous resolution is common. During the interim period before operative repair or spontaneous resolution it is critical to instruct patients on corneal protection. This should include lubricating eyedrops, protective eyeglasses, and eyelid taping at night. Lid malposition that does compromise the cornea, however, should be treated as soon as possible. Overall, better results with secondary blepharoplasty are achieved when surgery is performed at 6 months to 1 year following the initial surgery. This fact alone can create consternation for the unhappy patient and the eager-to-please plastic surgeon. In most cases the senior author underscores the value in the adage “never put off to tomorrow what may be done day after tomorrow just as well”. This chapter discusses considerations specific to secondary blepharoplasty.
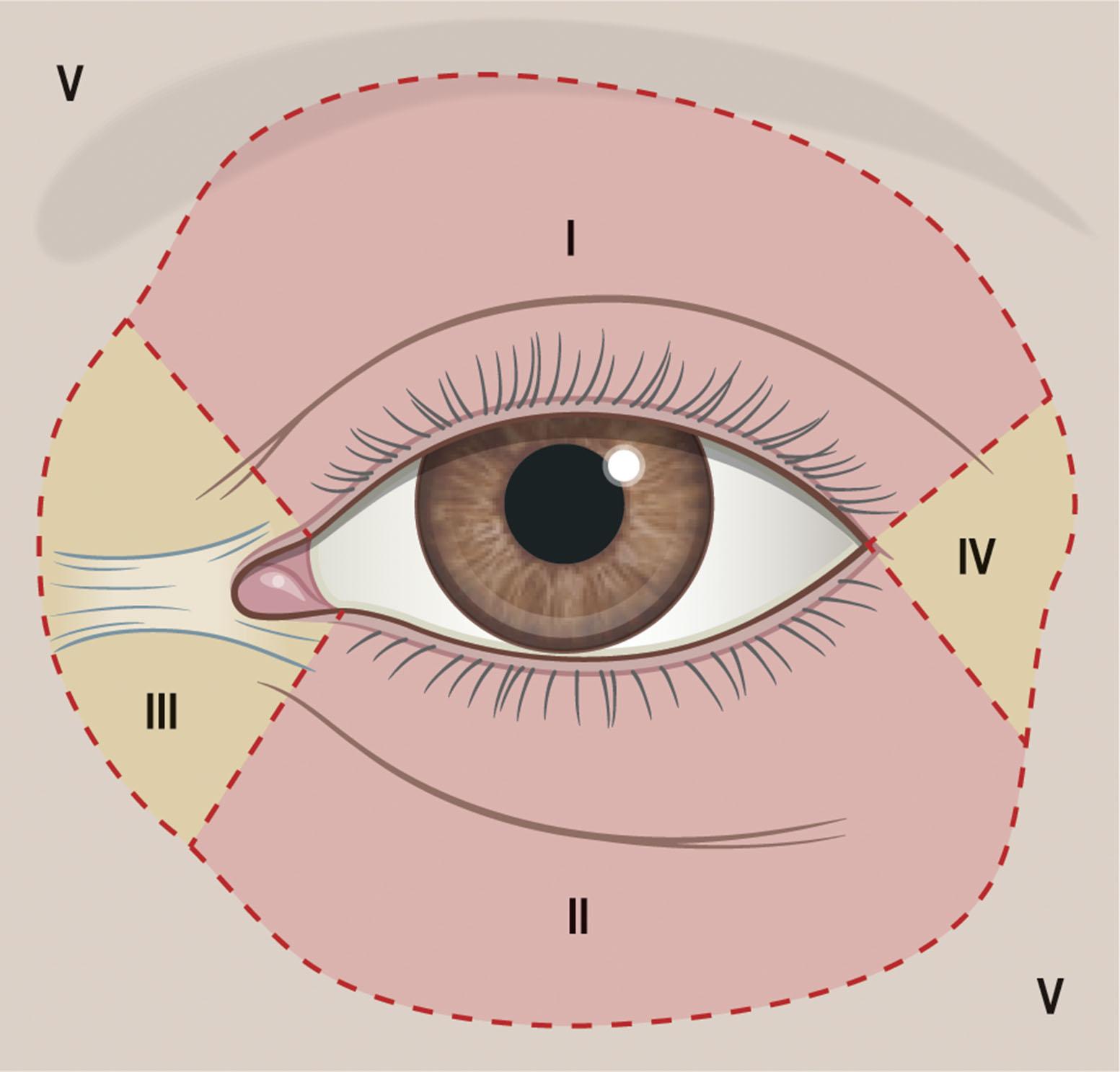
The skin of the eyelid is the thinnest in the body and has minimal subcutaneous fat. Tissue outside the eyelids but in and outside the periocular region (zones III, IV, V) is histologically, structurally, and mechanically thicker and less pliable and must be considered as contributory to eyelid functional and aesthetic disorders ( Fig. 14.1 ) . As patients age, the periorbital skin has decreased type I collagen synthesis and increased dermal collagenase activity. With time, these metabolic shifts lead to thinning, folding, and wrinkling of the eyelid skin.
The orbicularis oculi is the sphincter of the eyelid ( Fig. 14.2 ). This muscle is adherent to the overlying skin and comprises three parts: orbital, palpebral, and lacrimal. The outer orbital portion attaches medially to the medial canthal tendon, the nasal part of the frontal bone, and along the inferomedial orbital margin. Laterally, the orbital portion continues around the orbit and attaches to the lateral canthus. The palpebral portion of the orbicularis oculi, the middle segment, has pretarsal and preseptal segments. Medially, the preseptal segment of the palpebral portion of the orbicularis oculi has the anterior head, which becomes the anterior crus of the medial canthal tendon and inserts into the frontal process of the maxilla, and the posterior head, which inserts into the posterior lacrimal crest (Horner’s muscle). Laterally, the preseptal fibers of the palpebral portion of the orbicularis oculi coalesce with the lateral palpebral ligament to form the lateral palpebral raphe. The small, inner portion of the orbicularis oculi, the lacrimal segment, interdigitates with the medial palpebral ligament. This portion of the orbicularis oculi arises from the orbital surface of the lacrimal bone, passes behind the lacrimal sac, and divides into upper and lower slips. These slips insert into the superior and inferior tarsi, medial to the puncta lacrimalia.
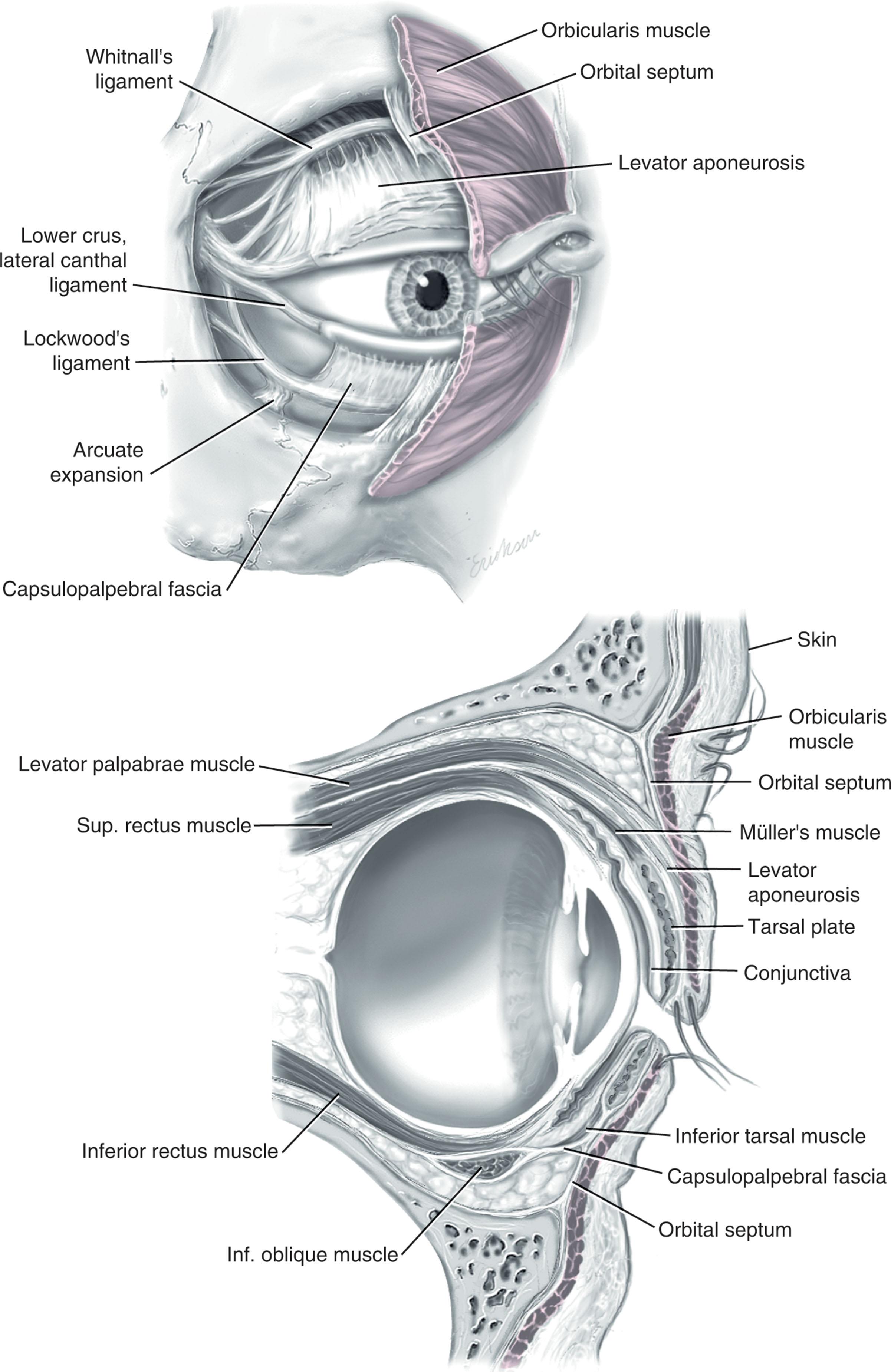
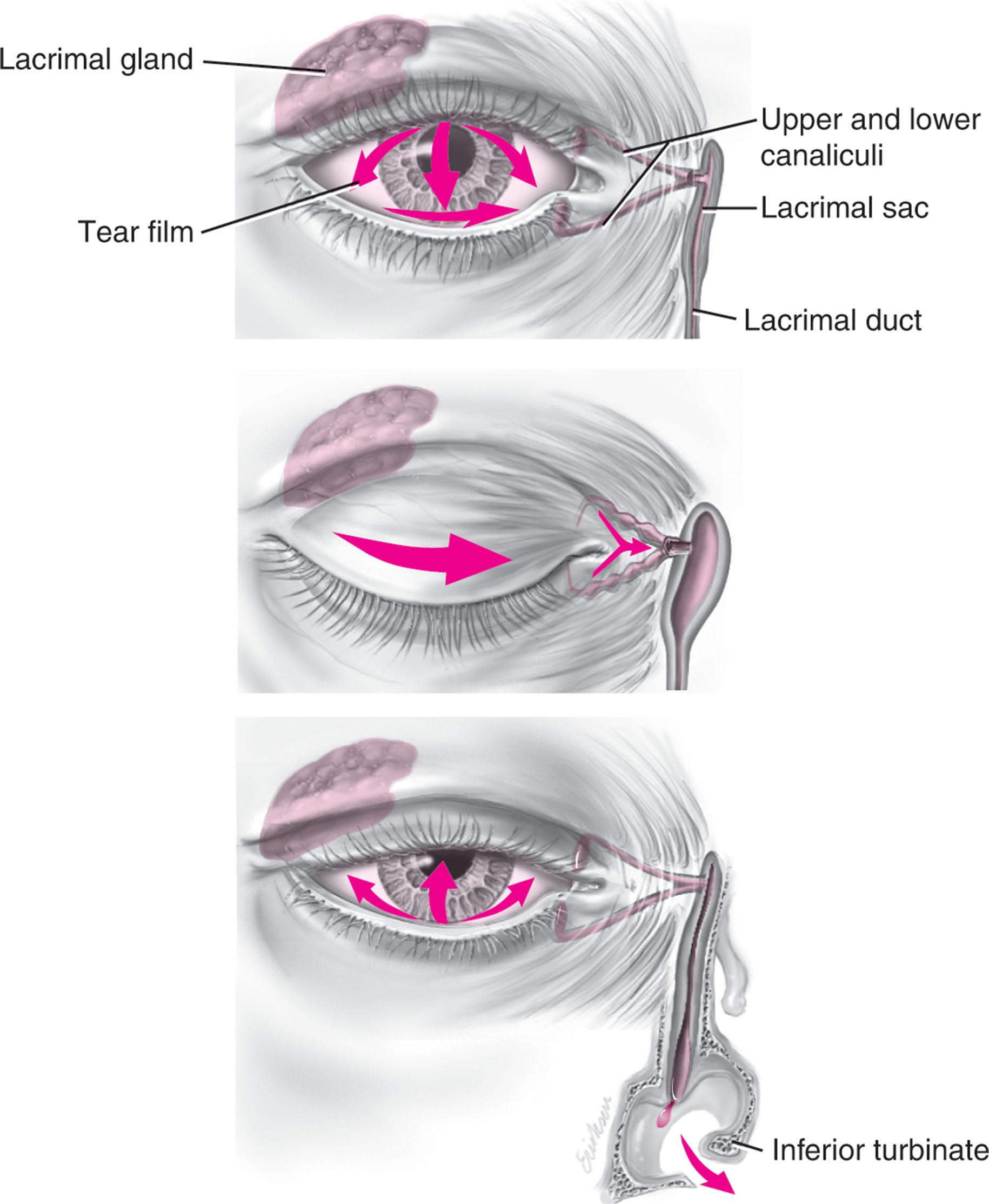
The three segments of the orbicularis oculi have distinct functions. The orbital portion of the orbicularis oculi tightly closes the eye. Contraction of the pretarsal and preseptal portions of the palpebral orbicularis oculi primarily closes the eyelid. The lacrimal portion transposes the lacrimal canals medially to receive tears and compresses the lacrimal sac ( Fig. 14.3 ) .
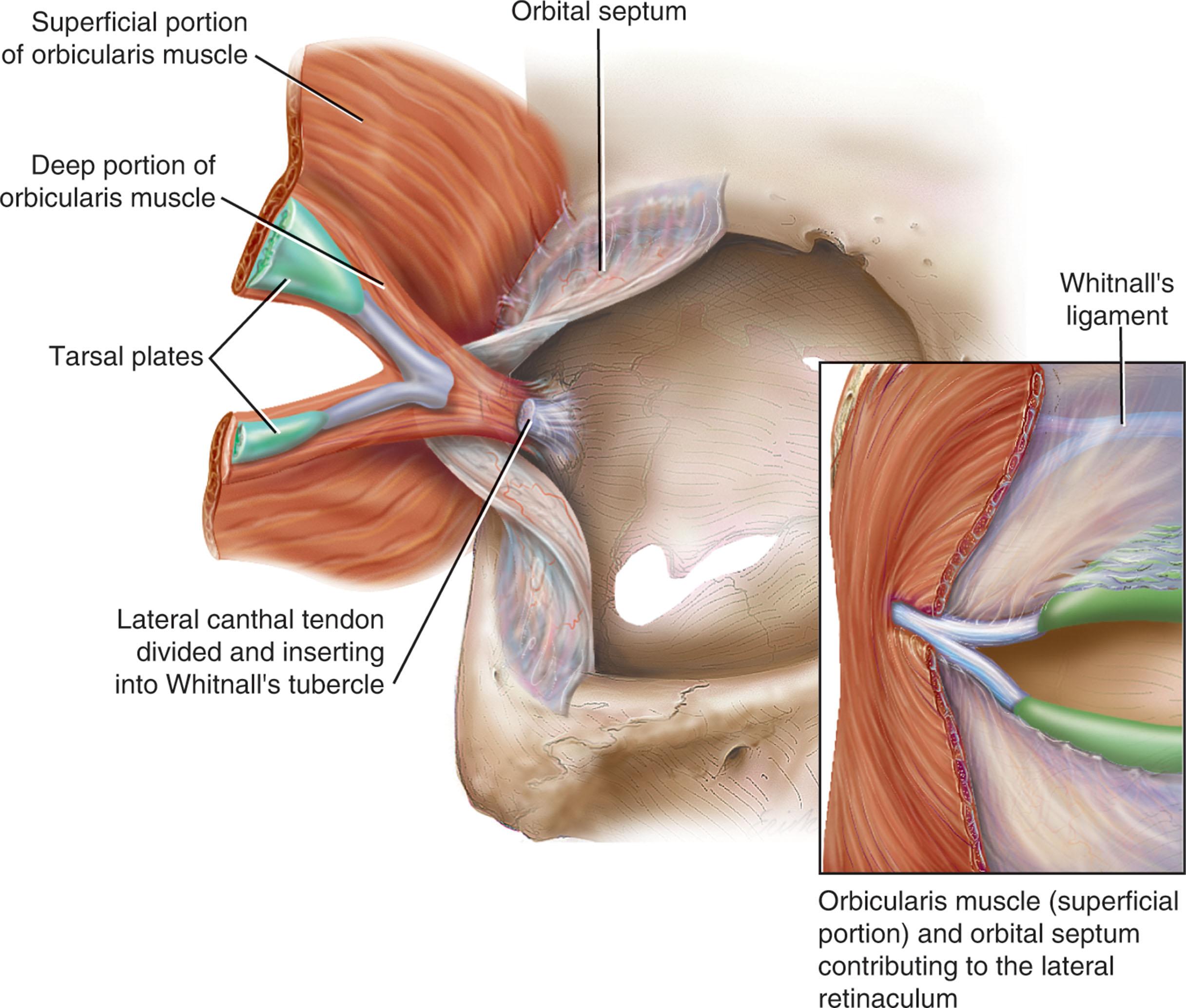
The orbicularis oculi is anchored by well-defined ligamentous attachments. Medially, the orbicularis occuli attaches directly to the inferior orbital rim. Laterally, the orbital retaining ligament bridges the fascia of the orbicularis oculi to the periosteum of the orbital rim. At the lateral canthus, the orbital retaining ligament merges with the lateral orbital thickening, a triangular condensation of the superficial and deep orbicularis oculi that extends across the frontal process of the zygoma onto the deep temporalis fascia. Release of the orbital retaining ligament and lateral orbital thickening allows untethered re-draping of the eyelid ( Fig. 14.4 ).
With age, the orbicularis oculi muscles relax, and the ligamentous attachments attenuate. This transformation results in progressive upper and lower eyelid ptosis. Malar ptosis compounds this eyelid ptosis, forming a malar crescent or festoon over the malar eminence with an aged appearance. In addition, the pigment of the orbicularis oculi becomes more apparent over the thinning skin. In effect, progressive senescent attenuation combined with Newtonian gravitational forces contributes to intercanthal narrowing, lateral canthal declination, lateral fat pad herniation due to septal laxity, eyelid malposition, and other pathology ( Fig. 14.5 ).
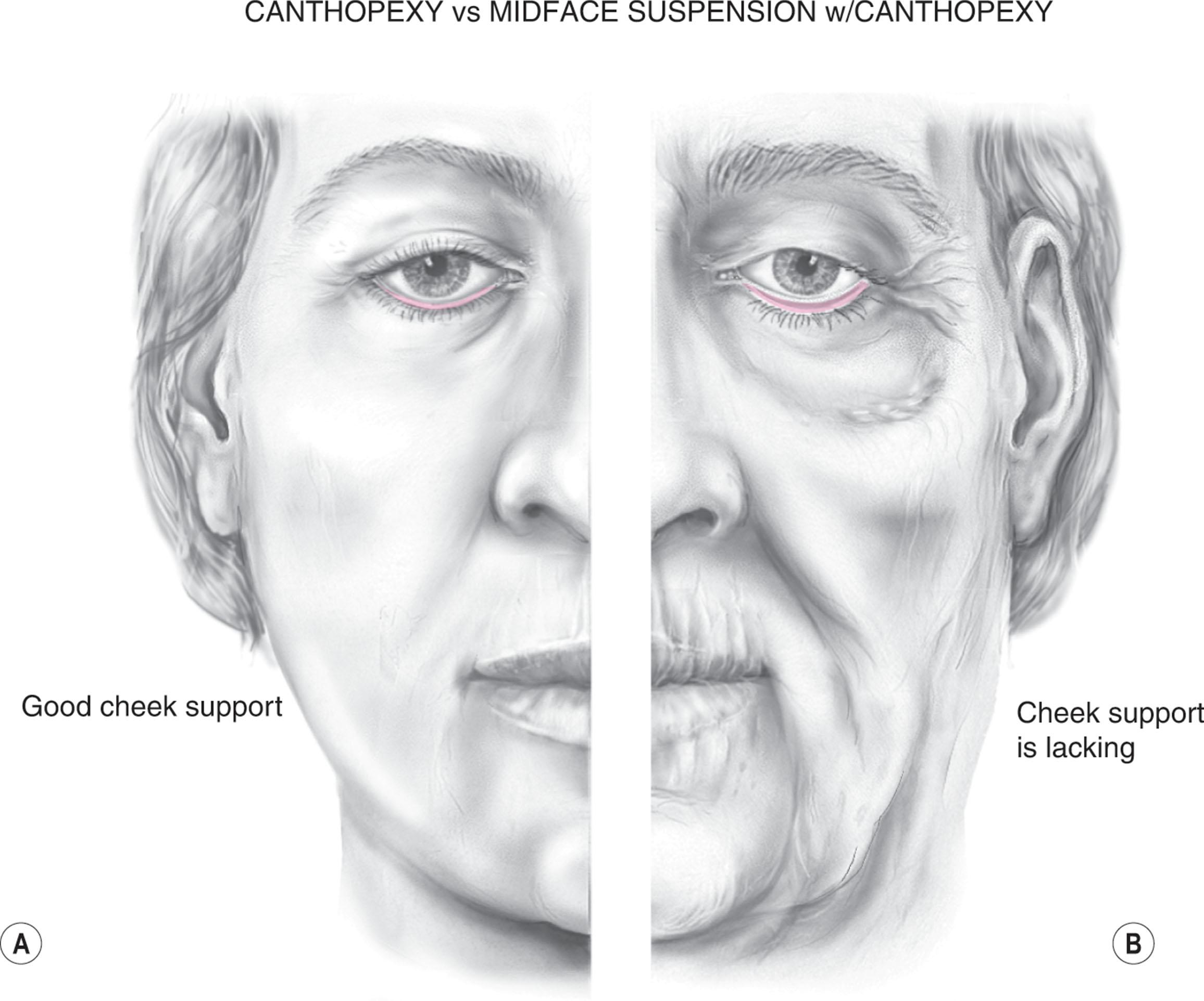
The critical point to evaluate in the patient preoperative period is the pressure or absence of lid face ptosis. In corrective secondary procedures, zone II (lower eyelid) should not be used to support zone V (cheek) in order to achieve an optimal functional and cosmetic result ( Fig. 14.6 ).
The tarsal plates, composed of dense fibrous tissue, are located directly above the lid margins and contribute to the integrity and support of each eyelid. Each tarsus measures approximately 29 mm long and 1 mm thick. The semilunar, superior tarsus measures 10 mm centrally and narrows medially and laterally. Conversely, the rectangular, inferior tarsus measures 3.5–5 mm centrally. The medial and lateral ends of the tarsus are attached to the orbital rims by the medial and lateral palpebral ligaments. Each tarsus contains approximately two sebaceous meibomian glands. These glands secrete meibum which is an oily substance that prevents evaporation of the tear film.
The orbital septum has dense fibroelastic tissue and forms the anterior boundary of the orbital contents. On the upper eyelid, the orbital septum inserts 10–15 mm above the superior tarsal border and joins the levator aponeurosis. On the lower eyelid, the orbital septum joins the capsulopalpebral fascia 5 mm below the tarsal border. In addition, inferiorly, the orbital septum fixates to the rim of the orbital periosteum and forms the arcus marginalis.
The upper eyelid has two distinct intraorbital fat compartments, medial and central, divided by the superior oblique. The medial fat pad is lighter and firmer than the central fat pad. In addition, the medial fat pad encompasses the infratrochlear nerve and the terminal branch of the ophthalmic artery. Of note, the lacrimal gland occupies the lateral compartment.
The lower eyelid has three distinct fat compartments: the medial, central, and lateral fat pads. The inferior oblique separates the medial and central fat pads. The central and lateral fat pads are separated by the arcuate expansion, a fascial band extending from the capsulopalpebral fascia to the inferolateral orbital rim.
The interconnecting septae of the intraorbital fat link the extraconal (outside the muscle cone) and intraconal (within the muscle cone) spaces. Traction on fat just posterior to the orbital septum can produce forces in any of these spaces and accounts for the small but definite risk of orbital hemorrhage or even blindness when addressing anterior orbital fat during a surgical procedure. The blepharoplasty surgeon should be well versed in the acute treatment of orbital hemorrhage.
The preseptal, or extraorbital, fat represents retro-orbicularis oculi fat (ROOF), which may accumulate outside the orbital rim on the inferior lateral brow and upper malar areas.
The levator palpebrae muscle is the upper eyelid retractor and originates from the lesser wing of the sphenoid, extending anteriorly along the superior orbit. The levator condenses approximately 14–20 mm above the superior border of the tarsus into Whitnall’s ligament. Anterior to Whitnall’s ligament, the levator forms a bilamellar aponeurosis that joins with the septum to insert into the tarsus. A lateral horn divides the lacrimal gland into the palpebral and orbital lobes and contributes to the lateral retinaculum. A medial horn inserts into the lacrimal crest. The posterior lamella of the levator aponeurosis contains Müller’s muscle.
The capsulopalpebral fascia forms the lower eyelid retractors. This fibroelastic tissue originates from the inferior rectus and oblique muscles, fuses into Lockwood’s ligament, and inserts approximately 5 mm below the inferior tarsus.
The lateral canthus partitions into an anterior and posterior leaflet. The anterior leaflet inserts onto the orbital rim periosteum, and the posterior leaflet inserts onto the lateral orbital tubercle (Whitnall’s), approximately 3 mm behind the orbital rim. The lateral canthus lies approximately 6 mm below the lacrimal gland fossa and is the culmination of the lateral canthal retinaculum, which consists of the lateral horn of the levator palpebrae superioris, preseptal and pretarsal orbicularis oculi, Lockwood’s ligament, and the check ligament of the lateral rectus muscle.
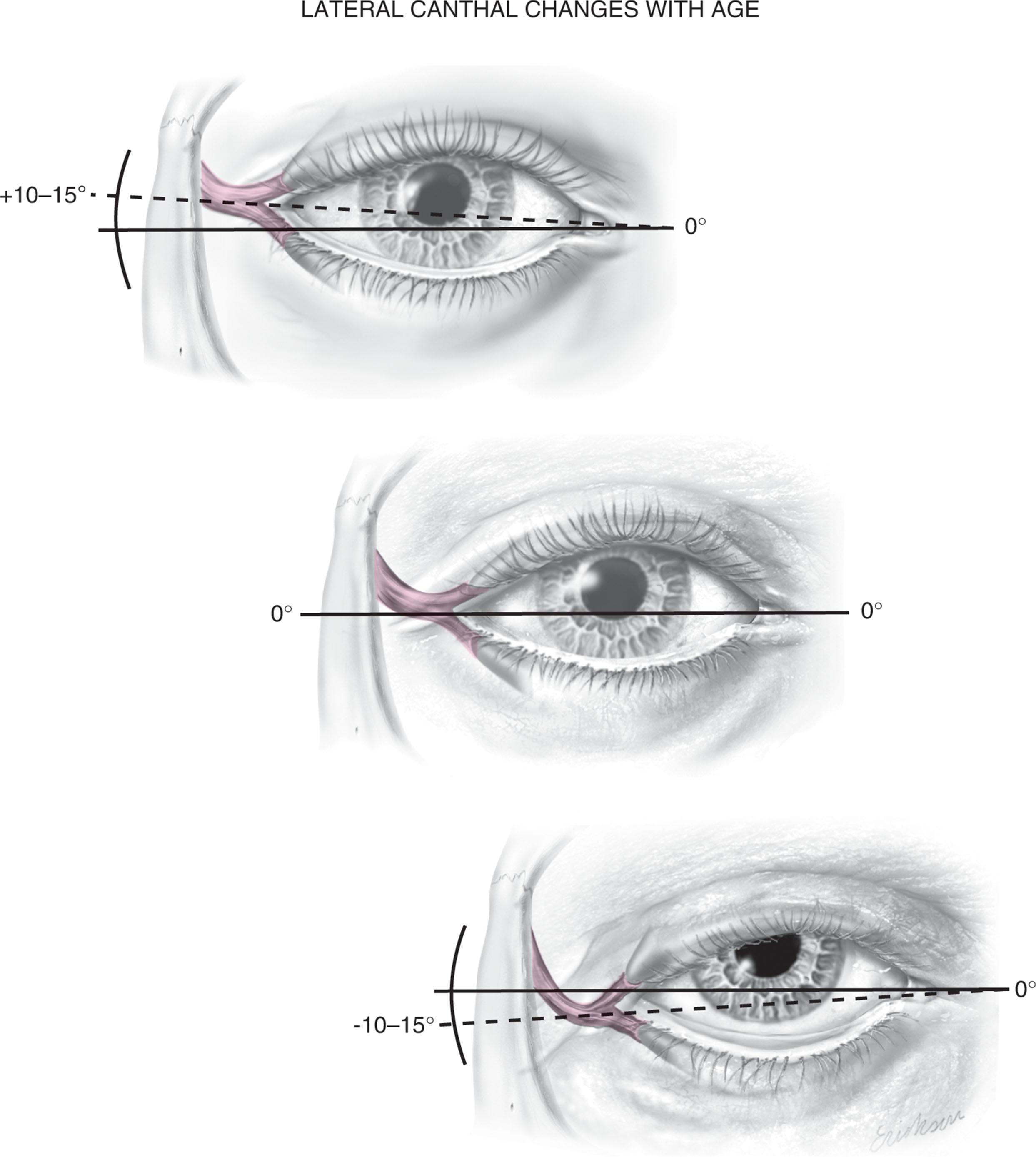
The ideal position of the lateral canthal tendon is 10–15° above the medial canthal tendon. All key elements of the lateral retinaculum must be addressed before mobilizing the lateral canthus for any repositioning or tightening procedures. Fig. 14.7A shows a patient with lateral canthal effacement and displacement after three blepharoplasties; she also had levator dehiscence, upper lid ptosis, and ectropion of the lower lid. Fig. 14.7B demonstrates correction of the lateral canthus, lid ptosis, and ectropion with levator advancement and canthoplasty.
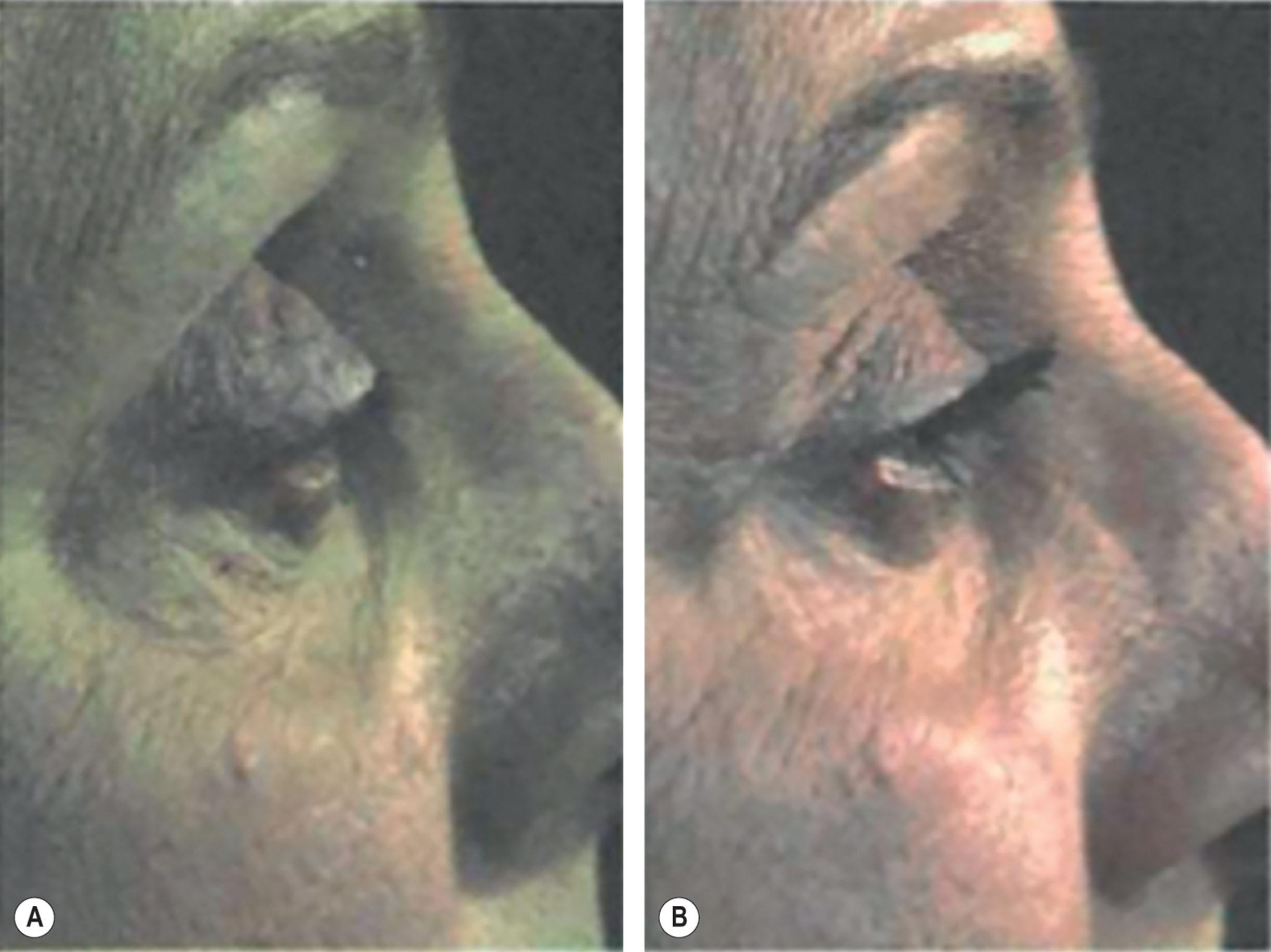
The treating surgeon should also note the position of the lateral canthus as a three-dimensional construct. The structure is supporting the eyelids laterally hanging in space. The lateral commissure (angle) lies within millimeters of the orbital rim and disruption of this anatomy can be noted in the repeat blepharoplasty patient. This disruption is especially notable after failed lateral canthopexy or canthoplasty procedures ( Fig. 14.8 ).
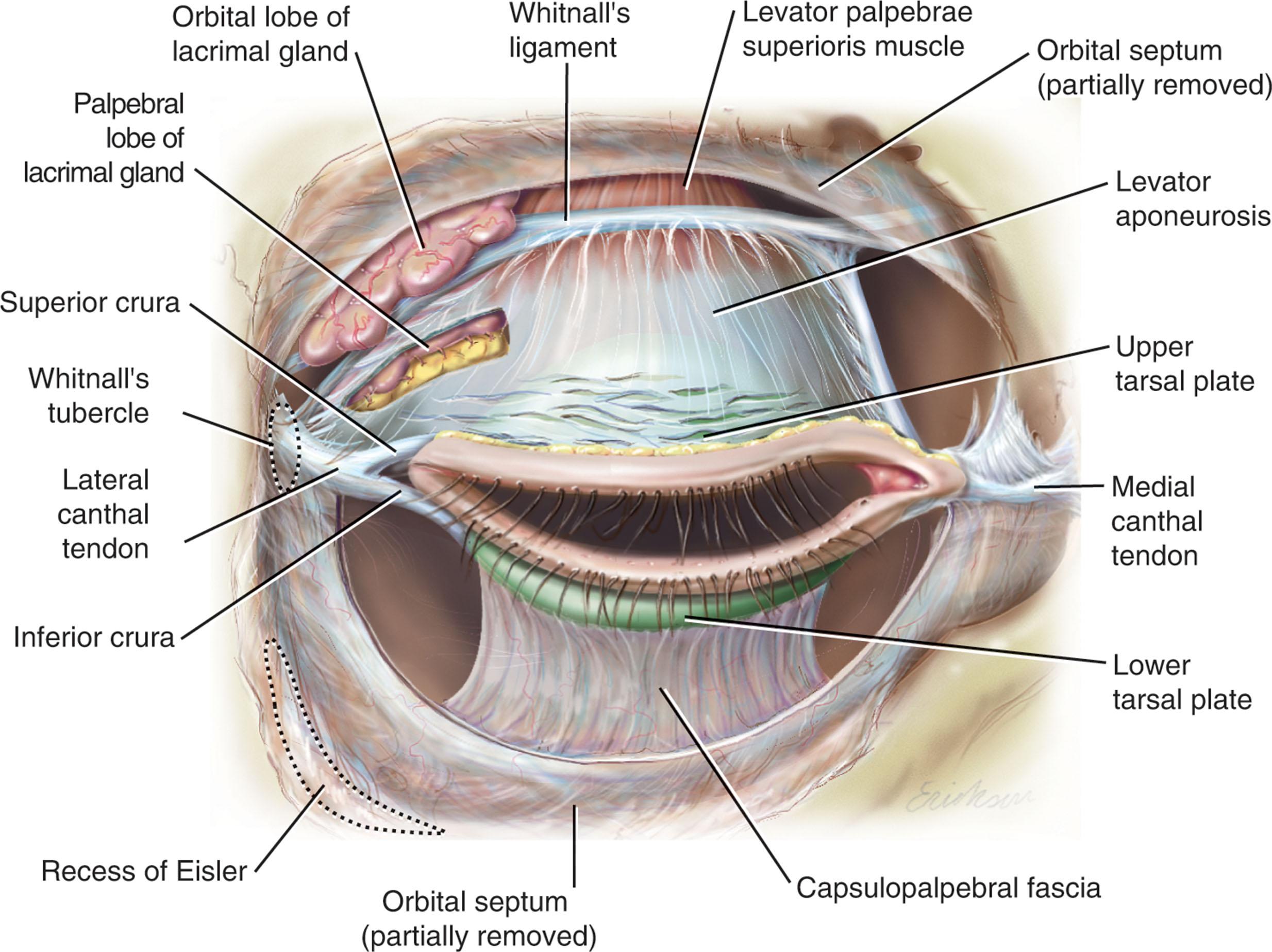
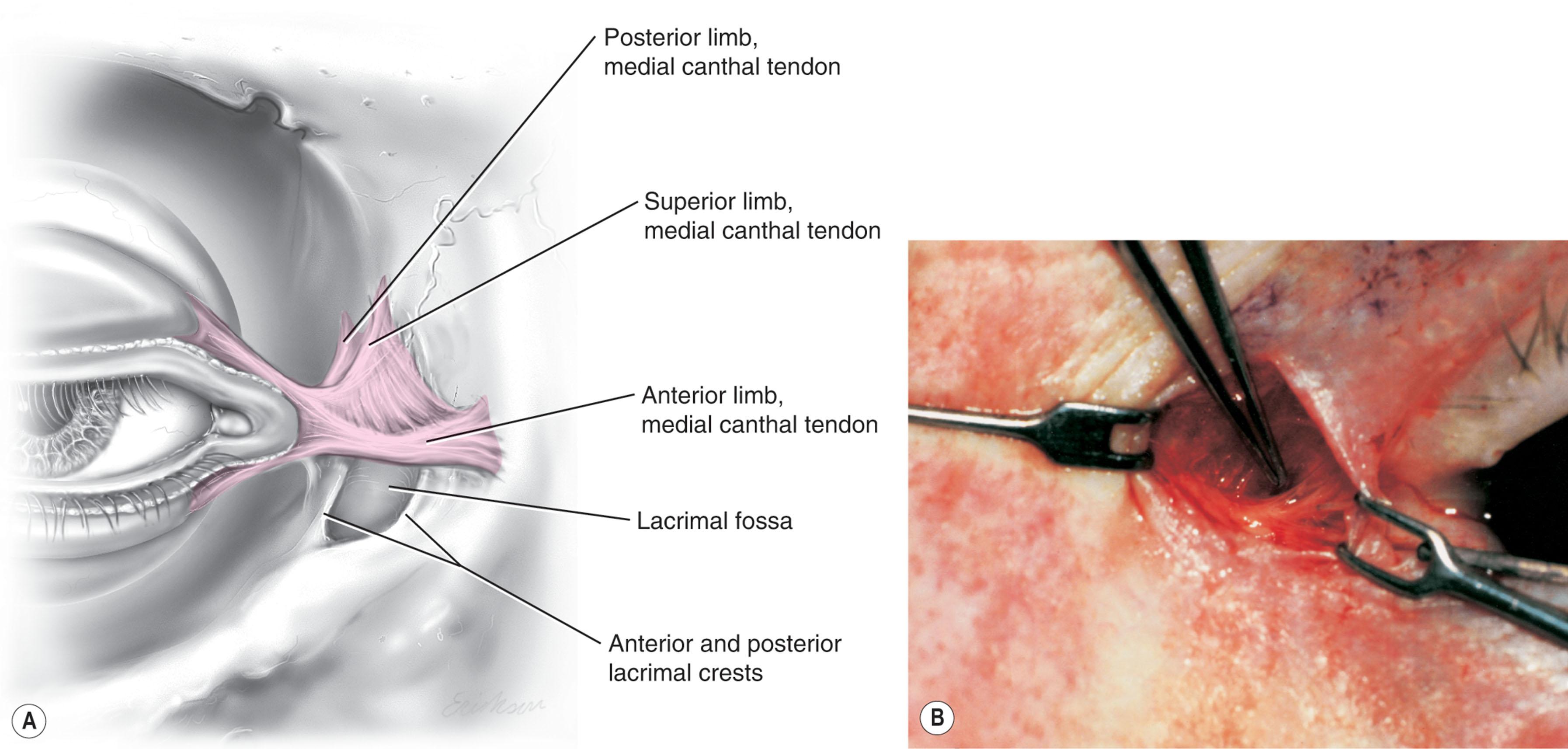
The medial canthal tendon inserts into the bony orbit with three leaflets: anterior and posterior horizontal leaflets and a vertical leaflet. The medial canthal tendon is the culmination of the medial canthal retinaculum, the confluence of the deep head of the pretarsal orbicularis, the orbital septum, the medial end of Lockwood’s ligament, the medial horn of the levator aponeurosis, the check ligaments of the medial rectus muscle, and Whitnall’s ligament. The upper, lower, and common lacrimal canaliculi are closely approximated to the medial canthal retinaculum and care must be taken to ensure their integrity when altering its position ( Fig. 14.9 ).
In any surgery involving the eyelids, corneal protection is necessary. Protective lenses are a routine part of any blepharoplasty procedure as these lenses function to prevent desiccation and injury to the cornea which can result in devastating consequences. Additionally, care must be taken to avoid corneal abrasions which may be incurred with any internal sutures; all knots should be buried or placed externally as to avoid inadvertently scratching the cornea as the sensitive corneal tissue will only tolerate opposition with conjunctival or mucosal tissues.
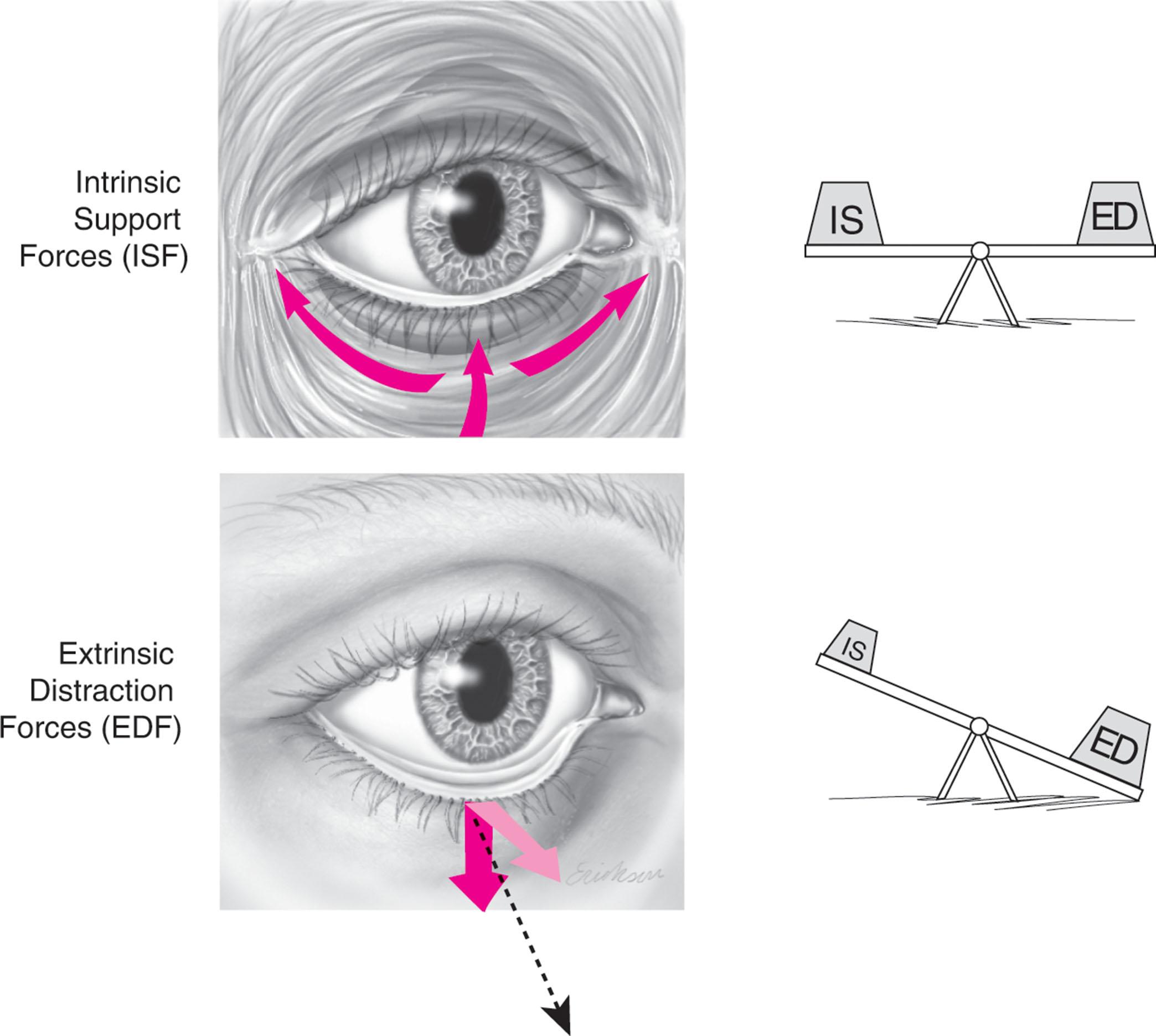
In performing blepharoplasty, it is essential to have a full understanding of how normal periocular anatomy changes with aging to select the right procedure for each patient. Especially important to understand is the fact that eyelids are a functional component of the larger face and their function is directly affected by anatomical neighbors. Specifically, as the upper lid is connected to the eyebrow and the lower lid to the cheek, as we age all of these tissues simultaneously undergo a predictable pattern of anatomical change related to loss of intrinsic support and gravitational forces.
With aging, the eyebrow, which is composed of skin, muscles (procerus, corrugator supercilii, depressor supercilii, frontalis, and orbicularis oculi), galea, and the brow fat pad (ROOF) undergoes attenuation of its ligamentous attachments which leads to eyebrow ptosis and descent onto the upper eyelid. This condition is termed dermatochalasis. Additionally, with aging the orbital septum develops laxity and the orbital fat pads protrude anteriorly (steatoblepharon), which lowers the upper eyelid fold position. The ligamentous attachments to the lacrimal gland (Soemmering’s ligaments) may also become attenuated leading to gland ptosis. While a low or absent upper eyelid fold is a component of age-related pathophysiology in occidentals, it is anatomically physiologic in Asian individuals wherein the levator fibers insert into the pretarsal skin more caudally, if at all. Furthermore, with aging the levator aponeurosis may attenuate or dehisce from its insertion site in the skin, leading to upper eyelid drooping, termed blepharoptosis, associated with elevation or loss of the upper eyelid fold. The levator muscle has tethering attachments to the overlying orbital fat pads and thus dehiscence of the levator aponeurosis can result in fat pad retraction and a superior sulcus deformity.
In the lower eyelid, the thin skin is prone to developing dermatochalasis with aging due to decreasing levels of collagen and elastin. With aging, the orbital septum develops laxity and the inferior orbital fat pads protrude anteriorly; the suborbicularis oculi fat (SOOF) may also contribute to lower eyelid fullness above the orbitomalar ligament and tear trough deformity in the nasojugal groove. In addition, the medial canthal tendon can become attenuated with age, which leads to inferior and lateral displacement of the lacrimal puncta resulting in inferior and medial descent of the tendon, which results in a further decrease in lateral canthal inclination. Descent of the lateral canthal tendon also shortens the intercommissure distance leading to horizontal lower eyelid laxity. Over time, this is exacerbated by downward distraction forces from the cheek and may result in malposition, causing conditions such as increased scleral show, ectropion, or entropion ( Fig. 14.10 ).
Midface aging also results in descent of the malar fat pads causing prominence of the orbital rims and bulging of the prezygomatic space from edema (malar mounds) or orbicularis oculi muscle redundancy (festoons). These two conditions can be very difficult to treat and may cause significant patient distress and consternation for the surgeon.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here