Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
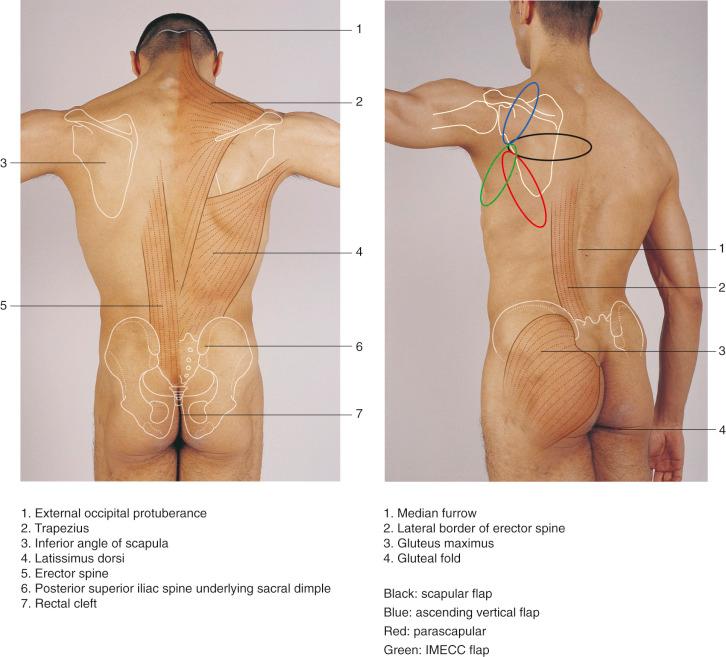
The skin and subcutaneous tissue of the back may be harvested as a flap supplied by the cutaneous or superficial branch of the circumflex scapular artery, originally named by Manchot. This branch is termed the “superficial circumflex scapular artery.” This skin artery divides into several branches: the horizontal (transverse) and vertical (descending), as well as the ascending and lateral branches. The horizontal and vertical branches supply the scapular and the parascapular cutaneous flaps, respectively.
Although the scapular flap was first described by dos Santos and the parascapular flap by Nassif et al., the cutaneous arteries, which irrigate these flaps, were first demonstrated by Manchot in his work on the arteries of the skin and later by Michel Salmon. The name of Iginio Tansini is frequently coupled with the latissimus dorsi musculocutaneous flap; nevertheless, it was later observed from his published diagram of the surgical technique that he was actually performing a parascapular flap. He eventually added the latissimus dorsi muscle to the original technique. A combined scapular and parascapular flap was first described by Koshima et al.
The use of the main trunk of the superficial circumflex scapular artery with all its branches allows harvesting of a larger skin surface from the hemi-back (extended circumflex scapular flap). Local and distant uses of these flaps have been extensively reported in the literature.
There is a direct vascular connection between the circumflex scapular vascular pedicle and the scapular bone. It is possible to elevate and irrigate a segment of the lateral scapular bone from the spine up to 2 cm inferior to the scapulohumeral joint based on this vascular network. This bone flap may be elevated independently or combined with the cutaneous flap. Alternately, the angular branch of the thoracodorsal artery supplies the inferior angle or tip of the scapular bone and can serve as the vascular blood supply for a bone flap that includes the tip as well as the adjacent medial and/or lateral scapular bone. There are numerous possibilities for chimeric flaps involving the scapular bone and skin in combination with other muscle, skin, and bone flaps arising from the subscapular system.
The subscapular artery is a branch of the axillary artery. At 2–3 cm after its origin, it divides into the thoracodorsal and circumflex scapular arteries. The circumflex scapular artery reaches the lateral border of the scapula; at this level it gives off a superficial cutaneous branch (the superficial circumflex scapular artery), which passes toward the subcutaneous tissue through a triangular space bounded by the triceps muscle laterally, the teres minor superiorly, and the teres major inferiorly. The lateral border of the scapula might be considered to be the medial border of a “quadrangular space.” The main trunk of the circumflex scapular artery continues toward the lateral border of the scapular bone. At this level it gives off several branches: a descending branch to the lateral border of the scapular bone (which eventually anastomoses at the tip of the scapula with the angular branch of the thoracodorsal artery), a branch to the teres minor muscle, another to the teres major muscle, a branch to the infraspinatus muscle, a cutaneous or superficial branch to the skin, and a main terminal branch that enters the subscapularis muscle and distributes in the periscapular arterial network. The branch to the subscapularis muscle and to the periscapular arterial network should be considered the main trunk of the circumflex scapular because it is always larger in diameter than the other branches, including the cutaneous branch.
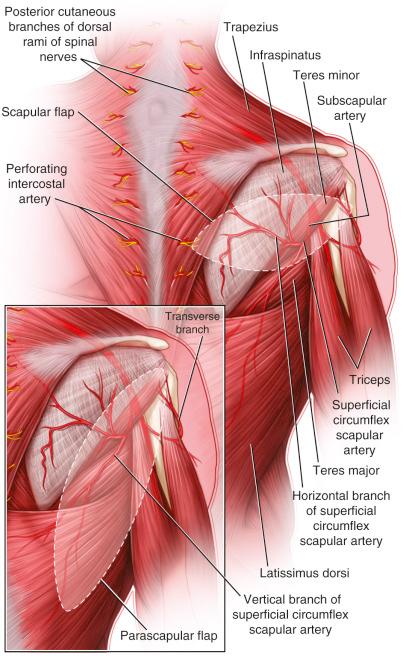
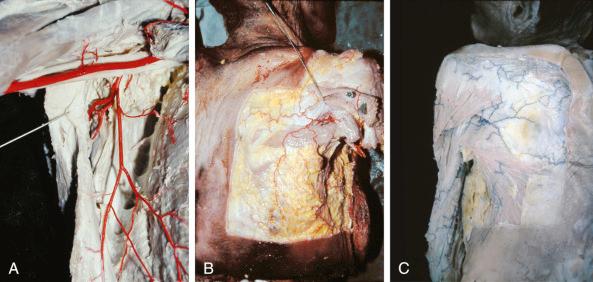

The superficial branch emerges and arborizes in the subcutaneous tissue of the back. There are two main branches in that arborization, the horizontal and the vertical, that distribute in the subcutaneous tissue of the back and anastomose with neighboring cutaneous arteries such as the perforators of the latissimus dorsi muscle, the perforators of the intercostal arteries, etc. ( Figs 40.1 , 40.2 ). The superficial circumflex scapular artery does not pierce any fascia or septum while coursing through the areolar tissue of the triangular space from its origin to the surface; however, it does pierce the deep fascia with terminal small branches to the muscles (infraspinatus, teres major, and latissimus dorsi). Once it reaches the subcutaneous tissue, it distributes above the deep fascia of the back. The deep fascia receives blood supply from the subcutaneous level via the cutaneous branches.
The vascularization of the lateral aspect of the scapular bone comes mainly from the main trunk of the circumflex scapular artery and its descending branch. Although the descending osseous branch supplies the lateral border directly, the main trunk gives profuse blood supply to the bone through its muscular branches.
The blood supply of the medial border of the scapular bone primarily comes from the deep branch of the dorsal scapular artery. The dorsal scapular artery is also known as the deep branch of the posterior scapular artery or transversa colli. There are interconnections between the dorsal scapular artery end branches and the circumflex scapular artery.
There is a branch of the thoracodorsal artery that supplies the tip of the scapular bone, which can be elevated independently with this pedicle. This branch is known as the angular branch and travels deep to the latissimus dorsi muscle within a fat pad lateral to the scapular bone. The branch terminates at the dorsal surface of the angle of the scapular bone.
As was mentioned above, there is a profuse vascular anastomosis between the lateral and medial vessels around the scapula; therefore, it is possible to perfuse different segments of the bone by any of these sources. However, it is technically difficult to raise a medial bone flap supplied by the circumflex scapular or, vice versa, a lateral border bone flap supplied by the dorsal scapular, as it would be necessary to disrupt the normal anatomy to a large degree.
Although the circumflex scapular artery most commonly originates from the subscapular artery, it may originate directly from the axillary artery (3% of the cases reported by Rowsell et al. ). Upton et al. reported the variation of the emergence of the descending branch; in some cases it pierces into the subcutaneous tissue inferior to the teres major muscle between this muscle and the superior border of the latissimus dorsi muscle.
To our knowledge, there is no “dominance” of either of the two main cutaneous branches. The superficial branch of the circumflex scapular artery truly bifurcates into the horizontal and vertical branches. Clinical observation demonstrates that equal flap length is supplied by these branches. Numerous anatomic dissections in injected specimens revealed that the horizontal and vertical branches are almost equal in diameter, although there are variations in different specimens.
The circumflex scapular artery can be dissected proximally to the level of the subscapular artery to extend the pedicle length and diameter (10–12 cm and 4 mm). However, this is usually not necessary and requires extensive effort.
The skin and subcutaneous tissue is an organ that provides protection and sensation. As with any other organ in the body, it has its own vascular anatomy, which is a regular uniform flexible vascular network. This network is irrigated by numerous arteries and drained by numerous veins that reach this organ from the depth. Once they enter the integument organ (the skin and subcutaneous tissue) they belong to, they are part of that uniform vascular network. What we observe by anatomic dissection of integument vascular pedicles is just a picture of the state of the vasculature at a determined moment or the artifact that we produced by the injection, which may have a similarity to the normal vascular physiology. The vertical branch of the superficial circumflex scapular (parascapular) forms a real vascular arcade with the thoracodorsal perforator, while the horizontal branch forms an arcade with the medial intercostals. These arcades are consistent all over the body in the subcutaneous tissue. They are “choke” anastomoses. It is therefore difficult to pinpoint the exact length of certain vessels. If we raise a 30 cm long flap irrigated by the parascapular artery, it would be logical to think that the artery has that length. However, it is overlapping with the anatomy of the thoracodorsal perforator and the lower intercostals. Do we assume that there is a simultaneous double arterial parallel pathway? It is more logical to accept the vascular network idea; in this case the vertical branch is part of that network. The cutaneous artery is the superficial or cutaneous circumflex scapular and the vertical, horizontal, and ascending arteries are arborizations of the former one. The superficial circumflex scapular artery is one of the largest skin arteries of the body.
horizontal branch of the superficial circumflex scapular artery
Length: 20 cm (range 10–24 cm)
Diameter: 1.2 mm (range 0.8–1.4 mm)
The superficial branch of the circumflex scapular artery reaches the subcutaneous tissue at the level of the triangular space, which is approximately two-fifths of the distance from the scapular spine to the scapular tip. At this point, it arborizes into several branches. The main two branches (considering their diameter) are the horizontal and the vertical ones; there are also an ascending branch and two or three lateral small branches to the shoulder area and axilla.
The horizontal branch runs parallel to the superior border of the latissimus dorsi muscle, 5–6 cm superiorly approximately, above the deep fascia almost attached to the fascia. In Figure 40.2 , the injected anatomic specimen shows the position of the horizontal and vertical branches.
The same pedicle irrigates the extended scapular flap. The vertical ascending branch of the superficial scapular artery irrigates the ascending scapular flap. The extended circumflex scapular flap is irrigated by all the branches of the superficial circumflex scapular artery.
second and third intercostals medial perforator
It is possible to raise this flap in reverse medial form irrigated by these vessels.
Length: 10 cm (range 8–12 cm)
Diameter: 1.0 mm (range 0.8–1.2 mm)
The scapular flap horizontal design can be vascularized from the medial side through the intercostal skin perforator of the second space.
vertical branch of the superficial circumflex scapular artery
Length: 20 cm (range 10–26 cm)
Diameter: 1.2 mm (range 0.8–1.4 mm)
The vertical branch of the superficial circumflex scapular artery originates at the level of the triangular space. It descends parallel to the lateral border of the latissimus dorsi muscle, approximately 6–8 cm medially. A few centimeters from its origin, it gives off an anterior branch, which is directed toward the inframammary fold and the anterior axillary line.
The anterior branch of the vertical branch of the superficial circumflex scapular artery is the vascular base of the inframammary extended circumflex scapular (IMECC) flap.
superficial circumflex scapular artery
Length: 20 cm (range 10–26 cm)
Diameter: 1.2 mm (range 0.8–1.4 mm)
The circumflex scapular artery gives off multiple branches that supply the lateral border of the scapula before dividing into horizontal and vertical branches, which supply the scapular and parascapular cutaneous flaps. While an identifiable medullary artery is often not found, there are multiple small vessels that have been observed by dye injection studies that clearly show vascularization of the scapular bone. A medial scapular bone flap vascularized by the horizontal branch of the superficial circumflex scapular artery has been described, although the primary blood supply to this region of bone is the dorsal scapular artery. The lateral scapular bone flap is usually preferred over the medial scapular bone flap due to its thicker bone stock and more versatile pedicle blood supply, allowing for many combinations of chimeric flaps.
angular branch of the thoracodorsal artery
Length: 7 cm (range 6–8 cm)
Diameter: 2.5 mm (range 1–3 mm)
The angular branch most commonly arises from the latissimus dorsi pedicle, but may also arise from the serratus anterior pedicle, as a trifurcation with the latissimus dorsi and serratus anterior pedicles, or proximal to the latissimus dorsi and serratus anterior pedicles. The angular branch of the thoracodorsal artery may be up to 7 cm long and is about 2.5 mm in external diameter. The pedicle can be extended up to 17 cm if the proximal thoracodorsal artery and subscapular artery are included.
Paired venae comitantes are intimately associated with the circumflex scapular and subscapular arteries and ultimately drain into the axillary vein. The venous drainage of the back has two main watersheds: the axillary region and the intercostal vein perforators, especially at the second, third, and fifth intercostal spaces near the vertebral column where large vein perforators accompany the cutaneous branches of the intercostal arteries. The laterally oriented veins eventually drain into the axillary vein.
venae comitantes of the horizontal and vertical branches of the circumflex scapular artery
The horizontal and vertical branches drain into the circumflex scapular vein, then the subscapular vein, and then the axillary vein.
Two venae comitantes are always present. In more than 250 cases we have never observed absence of the venae comitantes. They may vary in diameter following the compensatory law of Dubreuil Chambardell. If one is larger than usual, the other is smaller.
the intercostal veins, especially in the superior part of the thorax, have a large diameter.
There is a large perforator pedicle at the second intercostal space near the midline, which can be used easily as an arterial and venous donor vessel for a free flap.
The venous drainage of the flap parallels the arterial supply. The angular branch of the thoracodorsal artery is accompanied by paired vena comitantes.
the third, fourth, and fifth intercostal nerves through the lateral and posterior branches supply this region.
There is no single nerve that innervates a large region and it is therefore not used as a sensitized flap. When used for face and neck reconstruction, the scapular flap regains very good sensation without any special nerve connection.
there is no motor nerve involvement in these procedures.
If muscles supplied by the same vascular pedicle are included with the flap such as the latissimus (thoracodorsal nerve), serratus (long thoracic nerve), or teres major (lower subscapular nerve, a branch from the posterior cord of the brachial plexus), the corresponding nerves would have to be included with the harvest ( Fig. 11.1 ).
The flap is a skin and subcutaneous flap that may include bone (lateral border up to and including the tip, which can be irrigated by the same pedicle), fascia (deep fascia, dorsal thoracic fascia), and muscle (part of the latissimus dorsi, teres minor or infraspinatus, etc.). Although raising the serratus and the rib with this pedicle is technically possible, it requires including the latissimus pedicle plus the teres major muscle, which has to be sectioned, plus the serratus muscle, and is not of practical use.
These flaps are extremely reliable with a consistent vascular pedicle of good length and large caliber.
It is one of the best options when a large skin and subcutaneous flap is needed.
There is no functional morbidity at the donor site. There is no impairment of shoulder motion at all. Some discomfort and minimal pain are present in the first week postoperatively.
Depending on the individual, this area may provide non–hair-bearing skin.
The color of the back skin may provide a better match for head and neck reconstruction than the radial forearm or thigh flaps.
Two team approach can be used in cases of lower extremity reconstruction
When large flaps are harvested (such as extended scapular), the donor area may not be closed directly and has to be skin grafted. Therefore, aesthetic sequelae must be considered. Pre-expansion of the donor site avoids this inconvenience but adds a secondary operative procedure as well as possible complications.
The flap cannot be harvested with a single sensory nerve for sensory reinnervation.
The flap can only be harvested in the lateral decubitus or prone position, making it inconvenient when anterior defects are to be reconstructed.
No special studies are required prior to the operative procedure.
Deep scars at the flap pedicle area are contraindications to raising the flap. Superficial burns do not provide a contraindication to harvesting of these flaps even if the burn reaches the deep dermis.
There is no special preparation required except for adequately assessing the clinical condition of the patient and providing medical management accordingly.
Age in itself does not provide a contraindication to harvesting these flaps as clinical cases have been reported for patients ranging from 2 to 76 years old. There are no limitations as far as the size of the patient is concerned, but it must be borne in mind that obese patients have considerable thick back subcutaneous tissue. Patients with diabetes or arteriosclerosis are candidates for this type of flap because this area is normally not involved by disease in the medium-sized arteries.
Black : scapular flap
Blue : ascending vertical flap
Red : parascapular flap
Green : IMECC flap
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here