Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Sports-related injuries to the rotator cuff are fairly common, especially partial tears, which are most often traumatic injuries but can also be due to “overuse” of the glenohumeral joint. Treatment of rotator cuff tears is variable and depends upon the degree of the tear, but it is standard for non-surgical management to be the first treatment option for a rotator cuff tear. If non-operative treatment and rehabilitation fails, then surgical intervention is suggested. Surgical intervention is most common and useful in younger patients that participate in over-hand throwing activities. There is still much to be learned and improved in the treatment of rotator cuff injuries, especially when it comes to partial-thickness tears.
Keywords: contusion; epidemiology; partial cuff tear; rehabilitation; rotator cuff.
Sports-related injuries to the rotator cuff are relatively common, with complete rotator cuff tears being uncommon.
Rotator cuff contusions are most commonly traumatic injuries.
Partial rotator cuff tear can be the result of a single traumatic event or created by repetitive use, or what is commonly referred to as “overuse” seen in the overhead throwing athlete. The nonoperative treatment strategies need to be based on the mechanism of injury as well as the various factors contributing to the pathophysiology of the partial rotator cuff tear.
Identifying the predisposing factors, such as loss of internal rotation and scapula dyskinesia in an overhead throwing athlete, directs treatment strategies.
Adaptive changes occur to the rotator cuff in athletes so it is important to be able to distinguish these “normal” changes from pathologic conditions.
Nonoperative treatment successfully manages the majority of contusions and partial tears of the rotator cuff in athletes.
In the treatment of rotator cuff injuries in athletes, identifying the patient in whom nonoperative treatment has failed can be challenging.
The prevalence of rotator cuff tears, both partial and complete, increases with age. Magnetic resonance imaging (MRI) of asymptomatic patients has identified rotator cuff disease in 4% of those younger than 40 years and in 54% of patients 60 years or older ( ). reported a prevalence of 13% for partial-thickness tears of the supraspinatus tendon in a cadaveric study and 7% for full-thickness tears. In this group, 55% of the partial tears were intratendinous, 27% articular sided, and 18% bursal sided. In another study, partial articular-sided tears of the superior portion of the subscapularis tendon were identified in 37% of cadavers studied ( ). Articular-sided partial tears of the rotator cuff are much more common in young athletes. demonstrated that 91% of the partial tears seen in their study of overhand throwing athletes were based on the articular side. A study performed at the National Football League Combine demonstrated that 47% of the players had sustained a shoulder injury, 12% of which involved the rotator cuff ( ).
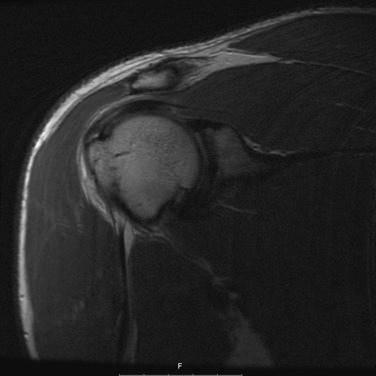
The prevalence of rotator cuff contusions is less defined in the literature. retrospectively reviewed shoulder injuries in collegiate football players. Contusions of the rotator cuff accounted for over half of the shoulder injuries. A direct blow was identified to be responsible for 70% of the contusions noted on MRI ( Fig. 6A.1 )
Rotator cuff tears, either partial or complete, are a different disease in young athletes. In a systematic review of the literature concluded that injuries to the rotator cuff in athletes younger than 40 years are the result of either direct blows to a healthy tendon with consequent injury or of chronic overuse that creates microtrauma in the overhead throwing athlete. reported on 10 athletes playing contact sports who sustained rotator cuff injuries due to a direct blow for whom nonoperative treatment failed. The initial diagnosis was a contusion in two patients and a partial rotator cuff tear in five.
described the extrinsic theory to explain rotator cuff pathology, which is not likely applicable to the young athlete. initially classified partial-thickness rotator cuff tears on the basis of location, grade, and size of the tear. proposed a simpler classification determined by the location of the tear and the tear severity based on a scale from 0 to 4 with greater than 3 being the highest grade. Further awareness of the importance of the intratendinous extension of the tear has been recommended ( ). The interstitial tendon tear has also been described to be an important factor determining the treatment of partial rotator cuff tears ( ).
The mechanism of injury in overhead throwing athletes is due mostly to repetitive microtrauma. Extreme loads are placed on the shoulder in the such athletes. Forces at the shoulder of up to 108% of body weight ( ) as well as peak humeral angular velocities up to 7000 degrees per second ( ) have been recorded in throwing athletes. Since most partial tears in athletes are on the articular side or intrinsic in nature ( ), the two most likely mechanisms are tensile overload and internal impingement. ( ) found that most of the partial tears they have treated included the posterior portion of the supraspinatus and the anterior portion of the infraspinatus tendons several millimeters proximal to the tendon insertion. They concluded that the injury is created by compression with shearing of the tendons. The deceleration phase of throwing creates high eccentric loads on the rotator cuff that mostly involve the supraspinatus. If the timing and force of the contraction are not adequate, the tensile forces placed on the rotator cuff can lead to injury ( ). The fact the tendon has poor vascularity is believed to contribute to an increased risk of injury due to microtrauma ( ).
Internal impingement refers to compression of the articular side of the rotator cuff by the superior glenoid during the throwing motion ( ). Most writers believe that this compression occurs in the late cocking and acceleration phases of the throwing motion. Several observations have provided insight into the cause of this “pinching” effect. Initially proposed as a contributing factor in internal impingement is subtle anterior shoulder instability related to attritional changes to the anterior band of the inferior glenohumeral ligament ( ). The increased anterior translation of the humeral head in an abducted and externally rotated position results in entrapment of the rotator cuff between the greater tuberosity and the glenoid. Subsequently it has been proposed that athletes with contracted posterior capsules are predisposed to internal impingement. This results in a loss of internal rotation (glenohumeral internal rotation deficit [GIRD]) ( ). Repetitive forces on the infraspinatus and the posterior shoulder capsule during the deceleration and follow-through phases of throwing create hypertrophy and stiffness in these structures. The result of these changes shifts the center of rotation of the shoulder to a more posterosuperior position. This abnormal position then creates the internal impingement. Poor scapula control may also lead to internal impingement. During the late cocking phase of throwing upward, scapula rotation helps maintain glenohumeral articular congruency ( ). Scapular dyskinesia allows the scapula to move into a protracted and upwardly tilted position, directing the glenoid anteriorly and superiorly ( ). The resulting greater external rotation during the throwing motion can produce internal impingement ( ).
Adaptive changes occur in the throwing shoulder. observed that “the throwing athlete can be considered on the edge of a cliff in terms of the demands of the throwing motion on the anatomic structures.” Signal abnormalities involving the rotator cuff on MRI are common in asymptomatic overhead throwing athletes. A study of asymptomatic minor league baseball players demonstrated that 40% had abnormal rotator cuff findings ( ). Studies also show changes to the rotator cuff can take up to 6 days to normalize after a pitcher throws ( ) Most writers agree that losses of internal rotation and of total arc of motion place the athlete’s shoulder at risk ( ). demonstrated that a loss of more than 5 degrees in total arc of motion in pitchers put them at increased risk of injury and that associated loss of internal rotation increased risk of injury at least twofold.
Rotator cuff contusions and partial rotator cuff tears in the athletes have various mechanisms. This diagnosis has resulted from direct injury or trauma in contact sport athletes. The overhead throwing athlete is at increased risk for this injury owing to microtrauma related to the forces generated in a repetitive nature. It is also likely, on the basis of literature findings, that various factors, possibly in combination, create the observed pathology. Knowledge of all the possible contributing factors is key to direct treatment strategies. An understanding of the adaptive changes that are seen in the overhead throwing athlete is necessary for the clinician to assure an accurate diagnosis.
There is currently a lack of guidelines based on randomized, prospective studies to aid the clinician treating partial rotator cuff tears and contusions. Also, most of the available studies lack adequate statistical power. The results of nonoperative management of partial-thickness tears are largely unknown because there are no long-term follow-up studies using a standardized treatment protocol. Nonsurgical treatment is still regarded as the initial management step. The goal of treatment in athletes with a partial rotator cuff tear is to eliminate pain and restore function. Treatment of the athlete with a rotator cuff contusion has the same objective. The goals could evolve if biologic interventions are developed that lead to a true healing response ( ).
Determining whether the injury is traumatic or is related to overuse is the first step to frame the treatment strategies. In the athlete with a trauma history, the initial goal is to control the pain and to restore full shoulder/scapula mobility and strength. The treatment for a partial rotator cuff tear in the overhead throwing athlete centers on the underlying deficiencies seen, such as loss of shoulder motion, scapula dyskinesia, and rotator cuff weakness. Mechanical flaws in the throwing or overhead motion may also need to be corrected.
The majority of patients in the study by examining rotator cuff contusions showed quick responses to treatment with modalities such as, pulse ultrasound and cuff/scapula strenthening. It was noted that the athletes who had significant subentheseal bone bruises and what the researchers called “chronic tendinopathy” had more prolonged recovery. In the patients who did not demonstrate significant improvement by the third day after injury (23%) a subacromial corticosteroid injection was utilized; this step was described to be of benefit, because only one of the six athletes who received a cortisone injection later needed surgery. Minimal morbidity was noted overall as a result of the contusions but 11% of the patients required later surgical intervention.
Separate Cochrane Systematic Reviews evaluating the benefits of electrotherapy modalities as well as assessing the value of manual therapy and exercise for rotator cuff disease have been performed ( ). Modalities such as transcutaneous electric nerve stimulation, therapeutic ultrasound, low-level laser therapy (LLLT), and pulsed electromagnetic field therapy are examples of the modalities potentially utilized in the electrotherapy evaluation. On the basis of low-quality evidence, therapeutic ultrasound may have short-term benefits for patients with calcific tendinitis, and LLLT may have short-term benefits in patients with rotator cuff disease. The review of the literature identified only 1 of 60 trials to be of high quality regarding manual therapy and exercise, and no benefit was noted.
In the overhead throwing athlete, shoulder rehabilitation should be directed at the underlying deficits, most commonly loss of shoulder internal rotation and poor control of the scapula. A four-phase approach is described by in the nonoperative treatment of throwing shoulder injuries. In phase 1, the “acute phase,” the primary goals are to diminish pain/inflammation, improve motion, activate the appropriate muscles, create dynamic stability and muscle balance, and restore proprioception. The athlete’s level of activity is adjusted according to symptoms, which usually require the athlete to abstain from activity. Internal rotation motion is addressed; the preferred stretches are the modified sleeper’s stretch and supine horizontal adduction with internal rotation stretch ( Fig. 6A.2 ). A horizontal adduction stretch with manual patient assistance into internal rotation is performed. Assessment of scapula positioning is also recommended, with strengthening of the scapula retractors and the lower trapezius and additional stretching of the pectoralis minor. The primary goals of phase 2, the “intermediate phase,” are to progress the strengthening program, improve the range of motion, and facilitate neuromuscular control. Core strengthening is also initiated during this phase. have emphasized the need to evaluate and treat the entire system to restore the athlete’s kinetic chain. Phase 3, the “advanced strengthening phase,” involves aggressive strengthening drills to promote power and endurance as well as functional drills, and throwing is gradually introduced. “Return to throwing phase,” phase 4, incorporates the progression of an interval-throwing program. This program controls for distance, intensity, and surface, in that for pitchers, throwing from the mound is the last advancement. It is important to be aware that when athletes are told to throw with 50% effort, they actually throw at 83% of their maximal speed, and when asked to throw at 75% they are actually throwing at 90% of their maximal effort ( ).

Corticosteroid injections have been commonly utilized in treating rotator cuff disease. performed a systematic review of the literature and analyzed nine randomized controlled studies comparing subacromial corticosteroid injection with placebo. One study demonstrated significant pain relief and two studies showed an increased range of motion in the injection group. No significant complications were identified. In a study comparing a corticosteroid injection with a platelet-rich plasma (PRP) injection for subacromial impingement syndrome, the investigators found the Constant score and VAS for pain to be significantly better at both 6 weeks and 6 months in the corticosteroid-treated group. Good patient candidates for a single subacromial corticosteroid injection to achieve pain control are those with significant night pain or patients who will not tolerate phase 1 rehabilitation because of pain.
PRP injections are being utilized for partial rotator cuff tears. There are mixed results in the literature. A randomized controlled trial (level I evidence) with a 1-year follow-up demonstrated no benefit from a single PRP injection in comparison with placebo ( ). Biologic type injections may have a role in the treatment of partial rotator cuff tears; however, the exact platelet count and leukocyte concentration in PRP for optimal growth factor activity has yet to be definitively proven in the literature.
Consensus has been reached on the correct management of patients with rotator cuff tears ( ). There are data showing that rotator cuff repairs in younger patients with a traumatic history are more successful than those in older patients with chronic tears ( ). Rotator cuff repair has not been as successful however in young overhead throwing athletes. ( ). Level I evidence is not available for surgical repair of partial rotator cuff tears in athletes. , in a level IV therapeutic study, reported that 55% of elite throwing athletes were able to return to their previous levels of competition or better, and 85% were determined to have good or excellent results following debridement of partial-thickness rotator cuff tears.
The other consideration is that the natural history of a partial-thickness tear is not fully known. demonstrated that 80% of partial tears they studied did progress during a 2-year period, 10% decreased in size, and 10% resolved. Concern exists that potential tear progression and possible muscle atrophy may compromise future surgical results. A randomized controlled trial in patients diagnosed with impingement syndrome was performed comparing a structured exercise program with arthroscopic acromioplasty. An MRI study performed at baseline was then compared with a study performed 5 years later for each patient. The nonsurgically treated patients did not demonstrate increased frequency of complete tears, and the two groups were similar in terms of muscle volume ( ). The mean age in the study was 47 years so these data may not be fully applicable to the young athlete.
Surgical intervention should be considered in the athlete whose injury does not respond to nonoperative treatment in 8 to 12 weeks. In a group of contact sport athletes undergoing surgery for rotator cuff injury, the average time from the time of injury to surgery was 9 weeks ( ). In the overhead throwing athlete, all deficiencies should be identified and corrected before surgical intervention is considered. This approach would mandate improving shoulder flexibility and strength as discussed, requiring at least 8 to 12 weeks.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here