Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The application of laparoscopic technology for advanced gynecologic operations resulted in significant patient benefits including reduced blood loss, shorter hospital stay, and a faster recovery as compared with laparotomy. Laparoscopic technology, however, had inherent drawbacks, which resulted in slow incorporation into the surgical practices of most gynecologists for the performance of advanced, and sometimes not so advanced, gynecologic operations. The limitations imposed by two-dimensional vision, instrument rigidity, and counterintuitive movements were among the reasons that precluded its widespread use.
Robotic technology was designed to facilitate laparoscopy and improve surgeons’ laparoscopic skills by eliminating the technologic drawbacks of laparoscopy, particularly by providing three-dimensional vision, instrument articulation, and intuitive movements. Other important additions were surgeon comfort (by providing a surgeon console where the surgeon can perform the operation sitting down, Fig. 118.1 ), tremor ablation, and downscaling of movements, which improve the surgeon’s precision. Because robotic technology is an improved form of laparoscopy, the terms “robotic-assisted laparoscopy” and “laparoscopy with robotic assistance” are used instead of robotic surgery. I prefer the use of robotic surgery to designate an operation performed entirely by robotics and the use of a hybrid procedure when a portion of the operation is by robotics and another portion is by laparoscopy.
Numerous studies comparing laparoscopy versus robotic technology with laboratory drills have shown improved surgical accuracy, faster intracorporeal knot tying, , , a reduction in skill-based errors, , and a shorter learning curve , , associated with robotics. However, reduced to its lowest common denominator, robotics is a refinement of the laparoscopic approach.
On July 11, 2000, the U.S. Food and Drug Administration (FDA) approved the da Vinci Surgical System (Intuitive Surgical, Inc., Sunnyvale, Calif.) for the performance of procedures in the abdominal and pelvic cavity, and in 2005 the device received specific FDA approval for the performance of robotic hysterectomy. The original Standard system was subsequently replaced by the S system and recently by the Si, which is the present model ( Fig. 118.2 ).

Improvements from the Standard system are longer instruments; lighter robotic arms with increased flexion-extension and lateral excursion, thus expanding the range of movement in the operating field; high-definition imaging; telestration; digital zooming; and a motor-powered robotic column. New instrumentation has included articulated vessel sealing device, suction irrigation, and a stapler for intestinal surgery. An innovative form of teaching was introduced with the teaching console. The teaching console is identical to the surgeon console, and both are interconnected, allowing the control of the robotic instruments to be switched back and forth between the surgeon and the trainee. The surgeon also manipulates a small cone to point where the trainee needs to dissect, cut, or prevent injury to tissues, facilitating surgical learning.
The da Vinci robotic system was designed for complex procedures in small spaces. Therefore manipulating large specimens and requiring a wide operating field are not optimal uses for the device.
I have performed more than 2000 da Vinci operations for benign and malignant conditions at Mayo Clinic Arizona since March 16, 2004. I have found specific advantages of the da Vinci system over laparoscopy in some conditions, both benign and malignant. Among them are advanced endometriosis, sacrocolpopexy, vaginal fistulas, radical hysterectomy, pelvic and aortic lymphadenectomy, excision of diaphragm and liver metastases, segmental bladder and ureteral resection, rectosigmoid resection, and other procedures in small spaces or areas of difficult reach such as presacral tumors or recurrent pelvic wall lesions.
In obese patients, because of the lack of tactile feedback of the robotic instruments, the console surgeon is unable to detect the additional resistance of the instruments through a thick abdominal wall, resulting in the surgeon’s effort and precision remaining unaffected. I did not find a lengthening of the operating time for robotic hysterectomy with increasing patient’s body mass index (BMI).
In gynecologic oncology, robotic radical hysterectomy has a shorter operating time than by laparoscopy, while other perioperative outcomes are similar. In endometrial cancer, the conversion rate of robotics is 3% compared with 9% for laparoscopy while other perioperative outcomes are similar. In early ovarian cancer, robotics and laparoscopy provide similar perioperative results. However, robotics is preferable for advanced ovarian cancer, in particular for resection of liver and diaphragm metastases.
The introduction of robotics resulted in a rapid decrease of the open hysterectomy, a fact that laparoscopy had not achieved, and demonstrates surgeon preference for robotics over laparoscopic technology. I do not recommend the use of robotic technology for a benign, large uterus requiring more than bisectioning for its vaginal removal. A vaginal hysterectomy is preferable. I do not recommend the supracervical technique because the short benefits do not outweigh potential risks. I do not recommend the use of any morcellator device to remove uterine or fibroid tissues due to its potential long-term consequences and risk of intraoperative injuries. I prefer vaginal hysterectomy for a benign uterus of any length as long as the anteroposterior and lateral diameters are shorter than the diameter of the pelvic brim, which will ensure enough descensus of the uterine fundus into the pelvis to complete the operation vaginally.
The robotic column is kept away from the operating table until ready for docking ( Fig. 118.3 ). It can be positioned centrally or sidedocked, right or left. When placed between the patient’s legs at the level of the patient’s knees, with the patient in the semilithotomy position, it impedes the access to the vagina, such as for removal of specimens or uterine manipulation. When placed lateral to the patient’s right or left knee, sidedocked ( Figs. 118.4 and 118.5 ), this drawback is eliminated, and the operation can be performed with the same ease as when centrally placed. Sidedocking is our usual placement of the robotic column. I have designed a platform for sidedocking ( Fig. 118.6 ) that facilitates placement of the robotic column in the same location for every pelvic operation.




A transumbilical open technique is used in all our patients for the insertion of the robotic laparoscope to avoid a major vascular injury. The upper abdomen is explored, and the head of the table is tilted until the small bowel and sigmoid are out of the pelvic cavity.
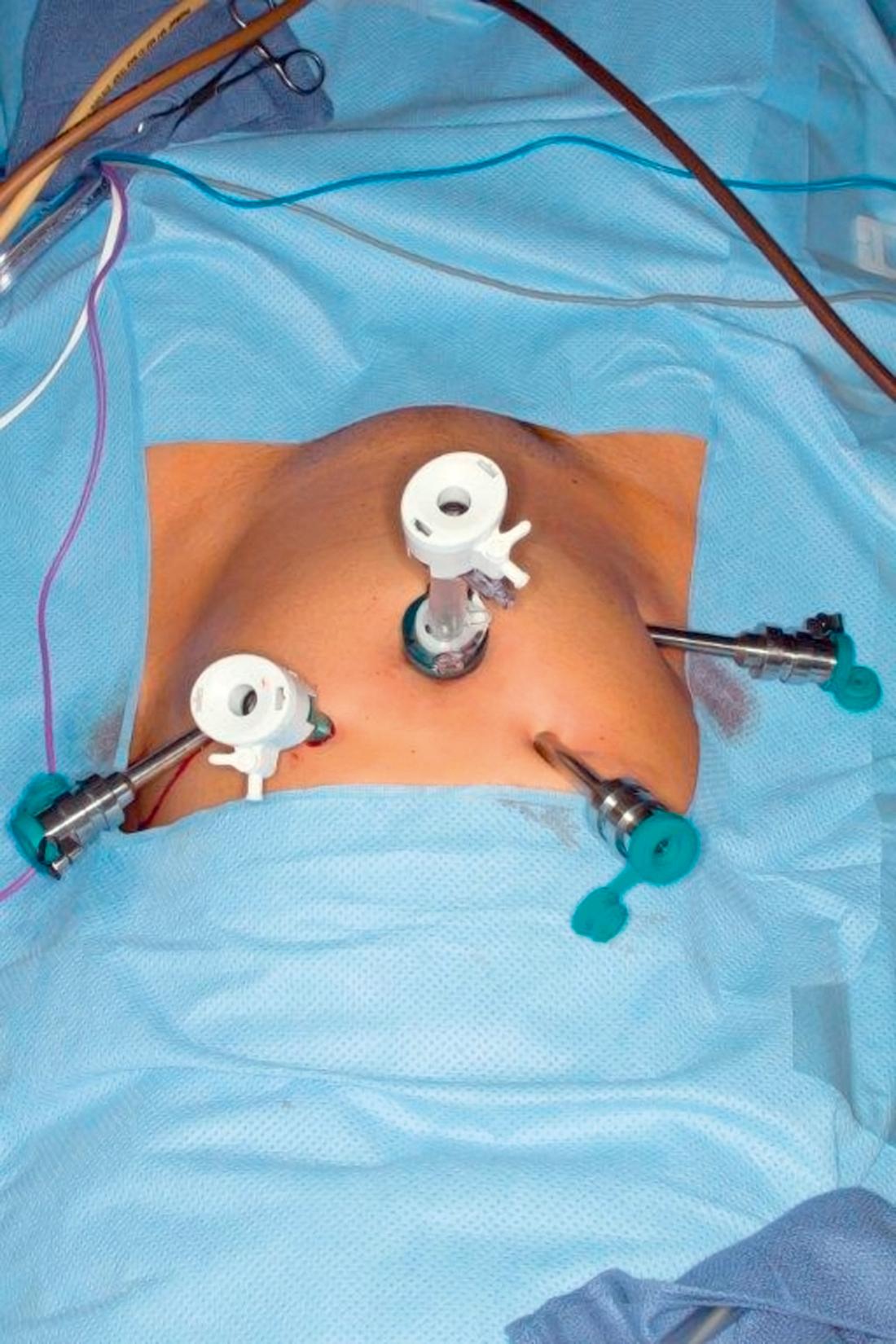
In all operations, a minimum of four trocars are used, three for the robotic arms (including the optical trocar) and one for the assistant. A fourth robotic trocar is used whenever the console surgeon requires additional assistance ( Fig. 118.7 ). My common trocar placement for pelvic operations , consists of two robotic trocars placed at the level of the umbilicus, 12 cm to the right and left, respectively. A 10-mm assistant trocar is placed equidistant and 3 cm cranial between the umbilicus and left robotic trocar. A fourth robotic arm, whenever used, is placed symmetric to the assistant trocar on the patient’s right side. The robotic arms are then attached to the robotic trocars. Once completed, the operating table cannot be moved and care must be taken to prevent the patient from sliding on the operating table ( Fig. 118.8 ).

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here