Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Acknowledgments: The authors would like to acknowledge Nathalie Baxter for her help in revising this chapter. We thank the authors of the seventh edition chapter: Paul Feldon, Andrew L. Terrono, Edward A. Nalebuff, and Lewis H. Millender. Parts of their work have been incorporated into this text.
Among the different inflammatory diseases, rheumatoid arthritis (RA) is one of the most prevalent forms. RA has an incidence of 0.5% to 1% depending on the population; it is more common in the northern hemisphere and its prevalence decreases from north to south. Although RA affects mainly the joints, it is considered a systemic disease because of extraarticular manifestations like vasculitis and muscle, heart, and lung involvement, among other medical comorbidities. ,
RA is best characterized as an immune-mediated inflammatory disease. The disease seems to be initiated by a complex combination of genetic and unknown extrinsic factors. Although a genetic predisposition is likely, its exact influence is still unclear. Even in monozygotic twins, the range of concordance is only 15% to 35%. However, a positive family history increases the risk of RA roughly three to five times. The seropositive forms have a higher degree of inheritance than the seronegative forms. Regarding extrinsic factors, smoking seems to be a significant risk factor for triggering the disease. Bacterial infection has often been cited as a possible cause of RA, but it has never been proven to be the single driving factor.
The main tissue involved in RA is the synovial membrane in joints and around tendons. In RA, the synovial membrane is hypertrophied in all its layers, is heavily infiltrated by inflammatory cells, and shows angiogenesis. The hypertrophied synovium, also called pannus, erodes cartilage and bone to leave significant defects. The driving cytokines in this process are interleukin-1 and -6 (IL-1 and IL-6) and tumor necrosis factor-alpha (TNF-α). Bone destruction is mainly mediated by macrophage-induced osteoclast activation. A major development in the identification and prognosis of RA is the detection of antibodies to cyclic citrullinated peptides (anti-CCP), which are part of the autoimmune reaction. The presence of anti-CCP is more than 98% specific for the diagnosis of RA and generally represents a more aggressive phenotype of the disease. Although not all patients with RA develop anti-CCP, these antibodies can be present up to 15 years before the first clinical symptoms. Rheumatoid factors are less specific for RA and are also found in other chronic inflammatory diseases, such as hepatitis C and tuberculosis. The most important inflammatory mediators in RA are cytokines, including IL-1, IL-6, and TNF. These cytokines are released in the synovial membrane and are responsible for many systemic manifestations of the disease, in addition to local destructive processes in bone and cartilage. ,
There are many different pathways leading to this disease, and no single disease agent explains the pathogenesis. Interleukins, T and B cells, and macrophages interact in a complex manner to initiate and sustain the inflammatory process.
This probably explains the different success rates of the various pharmaceutical agents. Even years before the clinical onset of disease, there may be raised levels of autoantibodies and cytokines in the blood.
Knowledge of the complex interactions among the different cell mediators has increased significantly over the last decade. This facilitates the development of new therapeutic approaches including biologics. The multiple immunologic and inflammatory pathways that seem to be active in RA may explain the effectiveness of different medications.
Among the different inflammatory diseases affecting the hand, the most common besides RA are psoriasis, systemic lupus erythematosus (SLE), systemic sclerosis, and crystal arthropathies (gout and pseudogout). Each of these diseases has specific patterns of hand involvement and requires an individual approach. However, the general techniques used to treat these diseases and RA are similar because the form of joint and soft tissue destruction is often comparable.
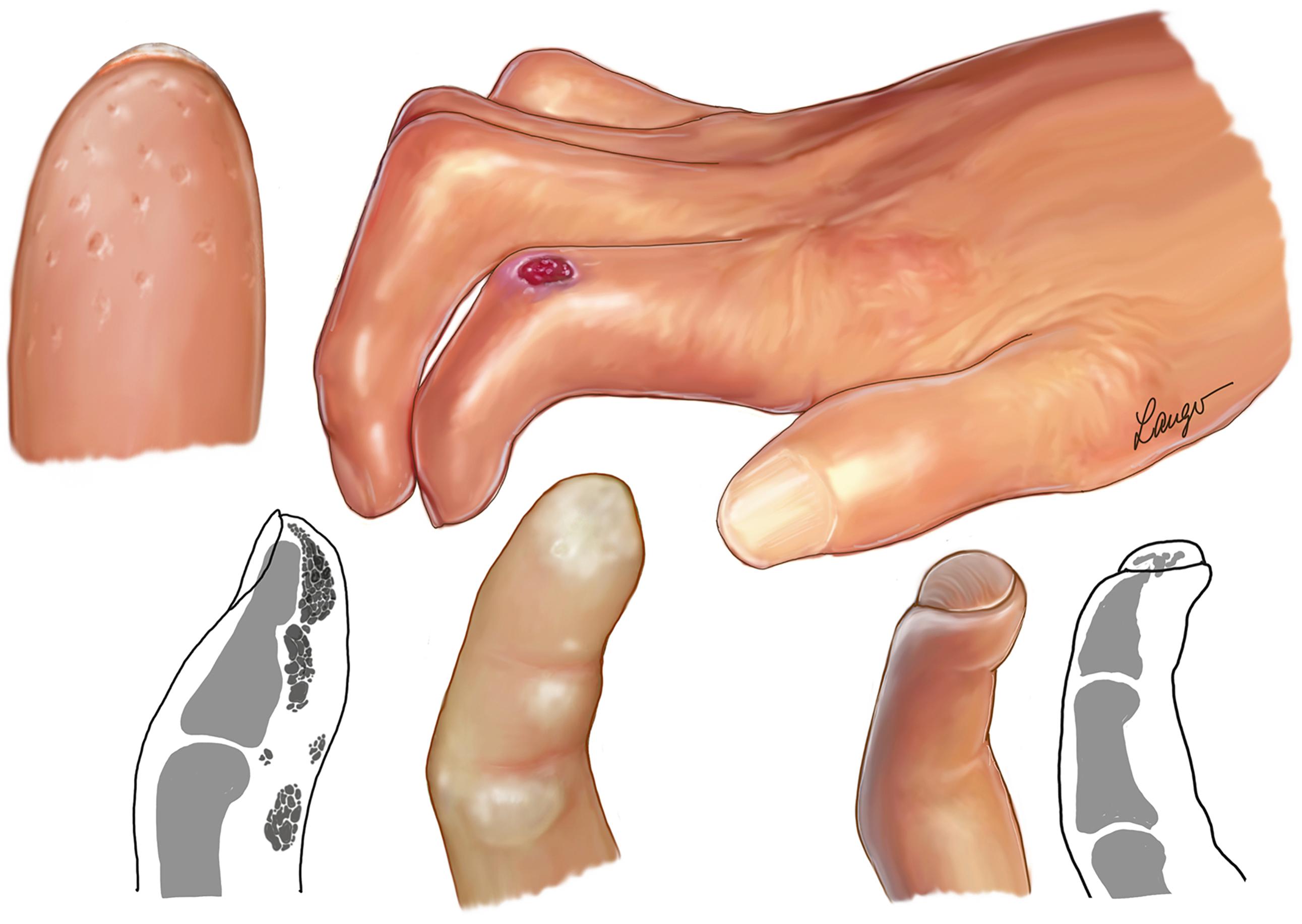
Thirty percent of patients who have psoriasis, a common skin disease, develop psoriatic arthritis. The course of disease is devastating on peripheral joints, as well as the spine and tendon insertion areas (e.g., Achilles tendon). In its most aggressive form, psoriatic arthritis causes arthritis mutilans, which is characterized by bone resorption or osteolysis. This leads to telescoping or flail or unstable fingers, and it is sometimes called “opera-glass” deformity. It is also called a “pencil-in-cup” deformity because of the radiographic appearance of the finger joints. Compared with RA, psoriatic arthritis shows oligoarticular and more distal joint involvement. A typical appearance is the dactylitis, a form of finger inflammation, which mainly involves the distal interphalangeal (DIP) and proximal interphalangeal (PIP) joints and surrounding soft tissue. This gives the fingers a sausage-like appearance ( Fig. 55.1 ).

Psoriatic arthritis is classified as one of the seronegative arthritides with no specific biomarker for detection. It typically starts around the age of 30 to 40 years but can also have an onset in childhood. Skin involvement usually precedes joint involvement, but there are cases in which the joint disease occurs first. This presents a challenge in making the diagnosis. In 2006, the CASPAR study group published classification criteria for the diagnosis of psoriatic arthritis. These include current skin psoriasis or a positive (family) history of psoriasis, dactylitis, juxtaarticular bone formation, nail dystrophy, and seronegativity. The specificity is 99% and the sensitivity is 92% using this classification system.
Psoriatic arthritis is a severe form of joint disease and spontaneous remission is extremely rare. The current treatment follows the similar approach as in RA. The pyramid of treatment includes nonsteroidal antiinflammatory drugs (NSAIDs), disease-modifying antirheumatic drugs (DMARDs) including Hydroxychloroquin, methotrexate, leflunomide, and biologics or biosimilars. The biologics in particular, if given early in the disease, proved to have a suppressive effect on skin and joint inflammation and may retard radiographic joint destruction. In cases of severe bone erosions in the finger joints, the bridging of bone defects is a challenge in treating the psoriatic patient.
SLE is a multisystem autoimmune disease affecting different organ systems including the skin and the joints. The course of the disease is variable and often starts in childhood. It is a potentially fatal inflammatory disease involving inner organs like the heart, lungs, and kidneys. Ninety percent of the patients suffering from SLE are females. The disease is much more common in African Americans and Asian Americans and in the Hispanic population. Although the cause of SLE is unknown, sun exposure, infection, and some medications have been identified as triggers of the disease. The butterfly-like rash on the face is a typical manifestation but may not be present in all patients. In the hand, an erythematode maculopapular rash might be present, especially after sun exposure. In the fingers, Raynaud phenomenon is often observed.
The typical finger joint deformity in SLE is often called Jaccoud disease, which consists of metacarpophalangeal (MCP) joint subluxation and ulnar deviation with or without swan neck deformity and Z-deformity of the thumb.
In contrast to RA, erosive destruction of the bone is not present, and there is little or no synovitis (dry joints) with passively correctable deformities. The disease seems to affect mainly the ligaments and the periarticular soft tissue.
The diagnosis of SLE involves a combination of clinical observations and additional laboratory markers. The most common but nonspecific sign of the disease is fatigue, fever of unknown origin, the typical skin rash, and arthralgia. The antinuclear antibodies (ANA) have a high sensitivity, and a titer of 1:80 is a sufficient criterion to make the diagnosis.
The treatment of SLE requires a team approach. Besides NSAIDs, hydroxychloroquine, with or without a glucocorticoid, is the first medical treatment of choice for patients diagnosed with SLE. Newer biologic medications are available, but because of the complexity of the disease, none of the current medications have been established as a standard treatment option. Treating the serious internal medical complications often takes priority over the arthritis symptoms.
When the patient’s medical conditions are stable, the hand surgeon can participate in treatment by correcting or preventing ongoing joint destruction in the hand. There is a limited role for conservative treatment. Passively correctable deformities can be treated with protective devices, especially during the day and in activities, with soft antiulnar drift straps. However, progressive deformity is not averted with these conservative measures. There is very little information about surgical joint preserving procedures in the literature, but it seems that there is high recurrence of joint deformity after such procedures at the MCP joint level. ,
Systemic sclerosis (SSc) is an autoimmune disease in which hand involvement is common. It affects females more often than males and its etiology is unknown. The hypothesis assumes a vascular disorder of the small blood vessels and of the connective tissue, leading to fibrosis. The medical treatment is based on the goal to fight the inflammatory process. Classically, therapy is based on glucocorticoids, methotrexate, and occasionally tumor necrosis factor inhibitors.
In the hand, SSc often starts with Raynaud phenomenon. Through inflammatory arthritis and fibrosis of the skin and the underlying soft tissue, disease progression ends in severe finger deformity. It typically produces PIP joint contractures that, together with a compensatory hyperextension of the MCP joints, causes a claw hand deformity. The inverse deformity, with MCP flexion and compensatory PIP hyperextension, is much less frequent. A contracture of the first web space limits the abduction of the thumb and inhibits the grasping of larger objects. Overall, the function of the hand is severely affected in the course of the disease ( Fig. 55.2 ).
Ulcers can occur at the tip of the fingers as a result of poor vascular circulation. They are often extremely painful and have only limited healing capacity. Through the fixed joint contractures, the skin over the MCP or PIP joints gets thin and can rupture. This leads to tendon and joint exposure, which increases the risk of severe infection. With splinting, meticulous wound care, and sometimes surgical debridement, the ulcer may heal. A combination of sympathectomy and vascular bypass procedures has the potential to improve the circulation to give a more durable solution for the healing of skin ulcerations. It is recommended, in cases of severe symptomatic finger ulcers, to perform an arteriography of the hand. When the radial or ulnar artery is occluded, an arterial bypass with vein grafting combined with sympathectomy is indicated. Sympathectomy is performed on the ulnar as well as on the radial artery at the wrist level. It might be combined with a digital sympathectomy for the most severely involved fingers.
In cases of progressive ulcerations, it is prudent to wait for auto-amputation to preserve maximum length of the digit. The fingers should be kept warm to prevent vasoconstriction.
Surgical interventions are rarely indicated in these patients. The fixed flexion contracture of the PIP joint is difficult to treat. In severe cases of PIP joint contracture, correction of the joint position to a straighter joint angle can be functionally meaningful. The functional gain of such an intervention depends mainly on the mobility of the MCP joints; the more residual movement they offer, the better the functional result of PIP joint straightening. If the MCP joints are already stiff, MCP joint procedures, such as joint resection or replacement, should be considered. It is preferred to perform the PIP joint correction first because the fibrotic skin over the MCP joint may cause additional problems. In the classic case of MCP joint hyperextension, a simple joint resection without implant arthroplasty, similar to interventions for feet deformities in RA, can be considered. A simple resection of the metacarpal heads from the volar approach overcomes the possible wound healing problem with a dorsal approach. In PIP joint correction, shortening of the bone is mandatory to facilitate repositioning and offers better wound healing because of dorsal skin redundancy. A too straight joint position, although esthetically nicer, should be avoided because it can compromise function. A flexion posture of around 50 degrees seems preferable.
PIP joint replacement is a rare procedure in scleroderma patients and seems to be associated with a high complication rate. The amount of bone resection for implant insertion is significant and may lead to substantial finger shortening, which can be a major problem for revision. The poor condition of the extensor tendon limits function.
Another problem that may require the need for surgical treatment is subcutaneous calcinosis. Calcium deposits can be intra- or subcutaneous, leading to skin breakdown and spontaneous discharge of the rather firm, toothpaste-looking white material. Unlike RA nodules, the calcium deposits do not respect any anatomic barriers and have a diffuse invasive characteristic. Partial removal through curetting using a small incision can provide pain relief. Extensive irrigation of the area and secondary wound healing are required in certain patients.
First web space contracture is often part of the hand deformity in SSc. Surgical correction is rarely indicated, and the results are often disappointing. The concept follows the classic principles of first web space release with adductor detachment and insertion of a skin graft, and in selected cases even the removal of the trapezium. The most gain is seen from the correction of a Z-deformity of the thumb. Fusion of the MCP joint, with or without release or simultaneous fusion of the interphalangeal (IP) joint, improves thumb function substantially.
One needs to be careful when considering surgical intervention for this condition because there is a lack of high-quality studies to support outcomes. The main concern is the vascularity and the subsequent healing potential of the tissue. With good preoperative planning and evaluation, the complication rate can be reduced.
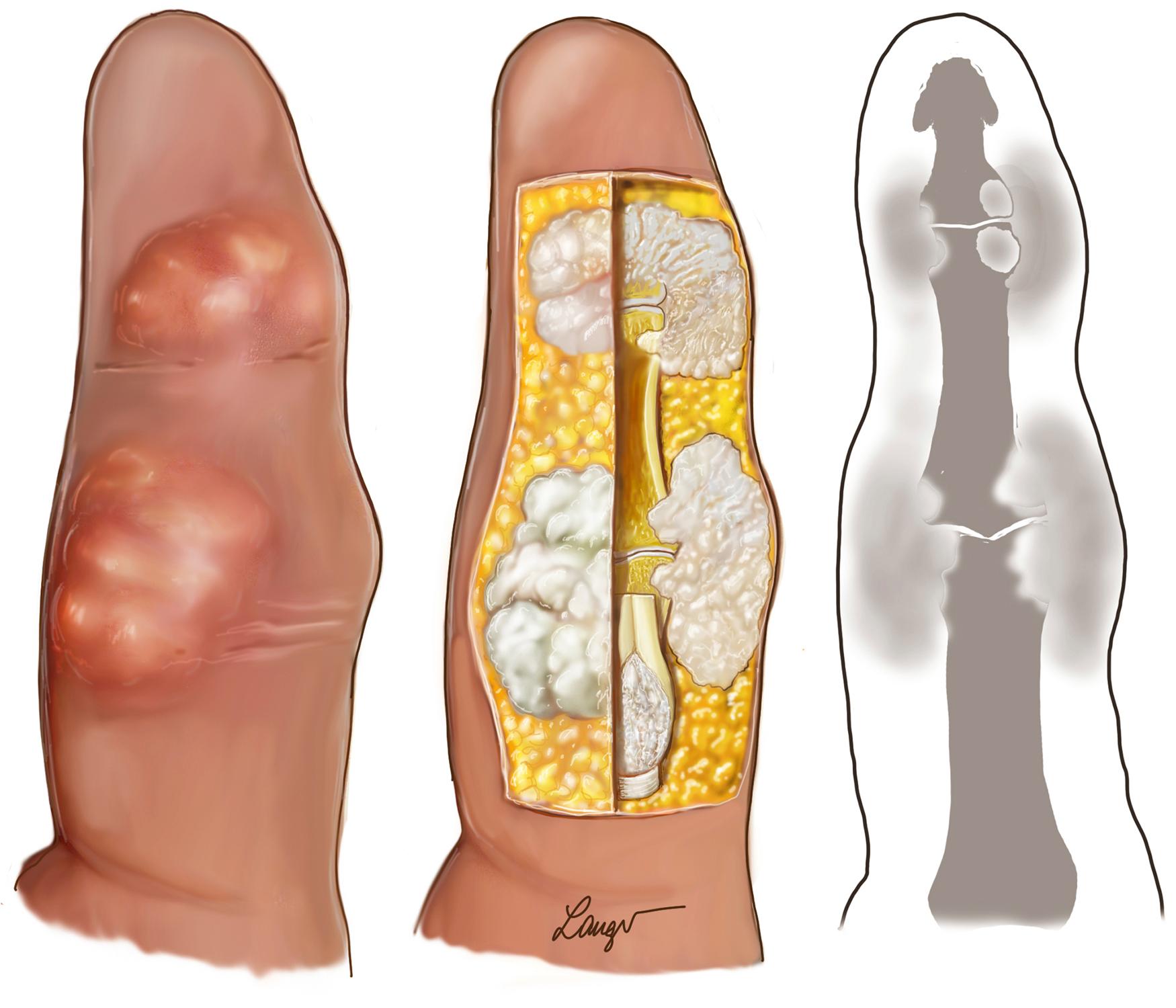
Gout is the most common type of inflammatory arthritis. Ninety percent of cases occur in men between the ages of 40 to 60 years. Gout classically affects the first metatarsophalangeal joint in the foot (called podagra) and distal joints in the hand, whereas the axial joints are typically spared. High blood levels of uric acid, a product of the protein metabolism, may produce the typical sharp and needle-like crystals, which can deposit in or near joints and cause inflammation. About one-third of the patients with a high uric acid blood level develop symptomatic gout. Known risk factors are dehydration, increased consumption of alcohol and meat, or trauma including surgery. The diagnosis is confirmed through aspiration of joint fluid and the proof of negative birefringent needle-like crystals. A normal blood level of uric acid does not exclude the presence of gout. The inflammation symptoms often appear as acute joint attack with redness, swelling, and substantial pain, mimicking an infection. In long-standing and progressive cases, bone destruction and deformity occur, especially in the distal finger joints. Some patients develop gout tophi, an accumulation of uric acid crystals in the soft tissue. Through its aggressive characteristics, gout can penetrate into joints and leave a substantial destruction ( Fig. 55.3 ).
The treatment of gout is primarily conservative, with the goal to lower the uric acid blood concentration and to fight inflammation. The medication to control the uric acid in the blood is allopurinol, which prevents the formation of uric acid. In the acute attack, typical antiinflammatory medications are administered, including corticosteroids given systemically or as local injections. Colchicine has proven to be effective in the acute gout attack, but due to its possible toxicity, it is the second line of defense.
Surgery of gout joints follows the principles of surgery of finger joints affected by other pathologies. Substantial bone defects are a challenge to overcome, but because of the inflammatory character, bone healing is not compromised. A difficult problem is the removal of gout tophi. Like in SSc and unlike in RA, the nodules penetrate all anatomic layers and produce significant soft tissue defects. During surgery it is almost impossible to remove all of the involved tissue, even with meticulous preparation. Nevertheless, by reducing the amount of inflamed material and maintaining good medical therapy, the operated sites have a good potential to heal.
Like gout, pseudogout or chondrocalcinosis (calcification of cartilage) mainly causes inflammation in the joints, which leads to marked joint destruction over time. The deposits in this disease consist of calcium pyrophosphate dehydrate crystals (CPPD). In contrast to gout, the crystals are microscopically birefringent and of rhomboid shape. The joints affected by pseudogout are the knee and the scaphotrapeziotrapezoid (STT) joint in the wrist. , Wrist x-rays showing calcification of the triangular fibrocartilage complex (TFCC) are almost pathognomonic for CPPD, especially in combination with STT joint arthritis. The cause of the disease is still unclear. It is more often observed in older individuals and can be associated with hyperparathyroidism or hemochromatosis. It is unknown whether CPPD causes osteoarthritis or if osteoarthritis favors CPPD deposits.
Scapholunate advanced collapse of the wrist establishes the diagnosis of CPPD, especially if it is bilateral and the patient has no history of relevant trauma.
There is no preferred medication to treat pseudogout and only little advance has been made in treatment. Once formed, calcium pyrophosphate crystals cannot dissolve, and therefore, management relies on the control of crystal-derived inflammation. Besides the classic medications such as NSAIDs, corticosteroids, and colchicine, IL-1β inhibitors have a potential to be effective, whereas methotrexate is not beneficial.
Table 55.1 summarizes the different disease pattern and their joint involvement.
| Characteristics | RA | Psoriasis | Gout | Pseudogout | Lupus | Osteoarthritis |
|---|---|---|---|---|---|---|
| Symmetry | ||||||
| Symmetric | + | + | ||||
| Asymmetric | + | + | + | + | ||
| Number of Joints Involved | ||||||
| Pauciarticular | + | + | + | |||
| Polyarticular | + | + | + | + | ||
| Hand Joints Involved | ||||||
| Wrist | ++ | + | + | (+) | ||
| CMC fingers | ++ | + | ++ | |||
| PIP | + | (+) | + | |||
| DIP | ++ | + | ++ | |||
| Thumb CMC/STT | ++ | ++ | ||||
| Other Joints Involved | ||||||
| Spine | + | + | ++ | |||
| Elbow | + | + | ||||
| Shoulder | + | + | ||||
| Hip/Knee | + | + | ++ | ++ | ||
| Ankle/Toes | + | ++ | ++ | + | ||
| Other Findings | ||||||
| Radiographic erosions | + | + | ++ | (+) | ||
| Nodules | (+) | ++ | ||||
| Dactylitis | ++ | |||||
| Calcifications | ++ | |||||
The goal in treating RA is to gain control of the inflammatory processes in the synovial membrane and prevent joint destruction. The common principles that guide management and the choice of medications have been derived from an increased understanding of the disease process, evidence provided by clinical trials, and other studies. Treatment is intended to lower disease activity and provide more sustained control of inflammation. This often requires initiating DMARD therapy early. The fact that the inflammatory pathways may be active years before the disease manifests clinically underscores the importance of early and aggressive control with agents that efficiently inhibit the devastating inflammatory process. The antiinflammatory potency of the different drugs can be defined in a therapeutic pyramid ( Fig. 55.4 ).
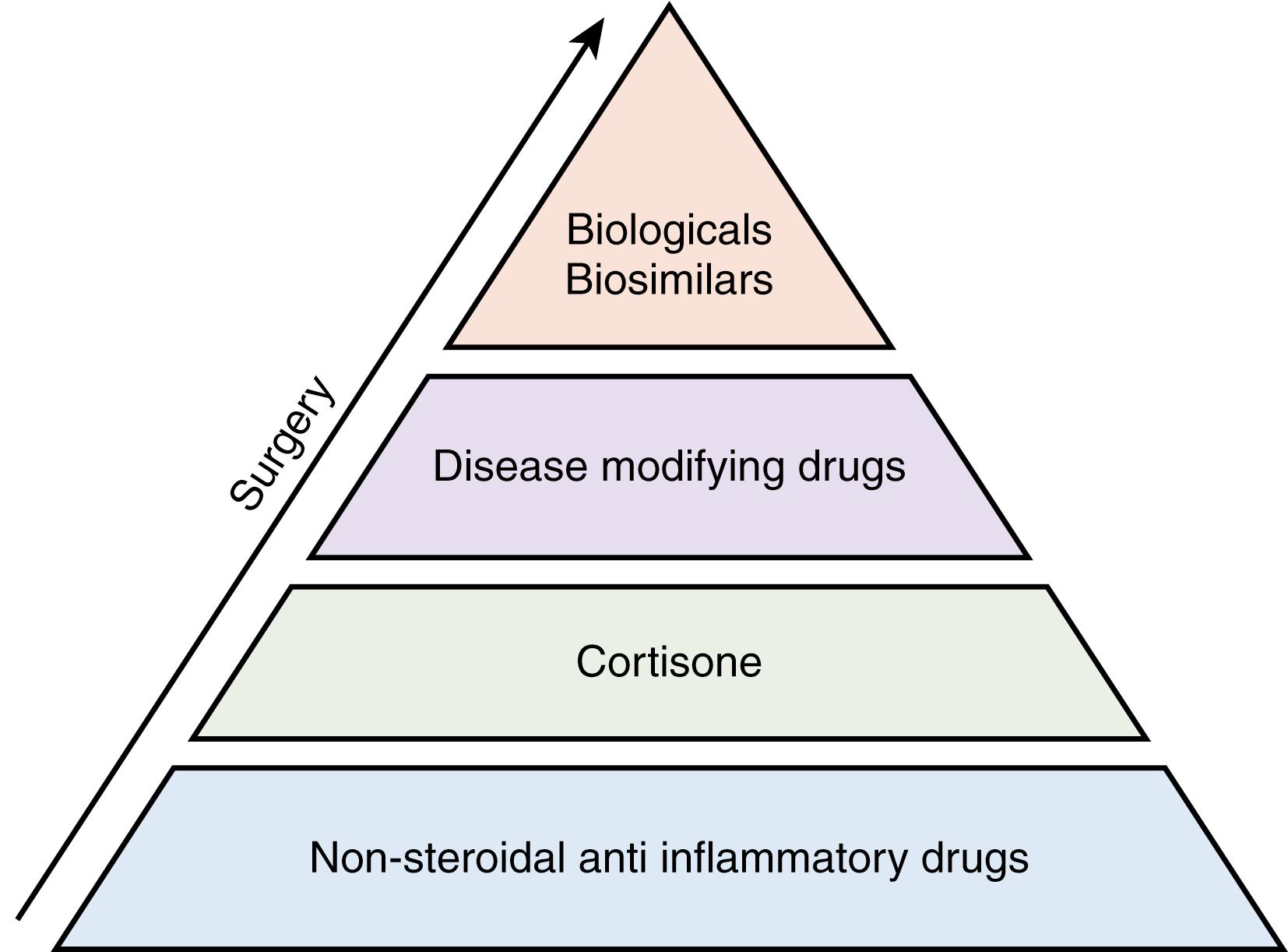
The first stage of pharmacotherapy includes NSAIDs, which mainly act as prostaglandin synthesis blockers. The next level consists of glucocorticosteroids, and then come the DMARDs. As well as having antiinflammatory effects, corticosteroids act by an immunosuppressive mechanism in RA. Methotrexate (MTX) is the best-known and most popular DMARD. It acts as an antimetabolite in the form of a folic acid analog. Its main effect in RA depends on the inhibition of T cells. Liver function should be monitored regularly because of its hepatotoxicity. MTX is often used in combination with corticosteroids and together with certain biologics in newer treatment regimens. There are also recent trends to use MTX in patients with severe forms of inflammatory osteoarthritis. Sulfasalazine is another popular DMARD. The precise reasons why sulfasalazine is effective in various forms of arthritis are not clearly understood. Chloroquine is the third classic drug in the triad of DMARDs; it seems to be most effective in combination with MTX and possibly as triple therapy with sulfasalazine and MTX. It was originally developed as an antimalarial medication but proved to inhibit lymphocyte proliferation in RA.
Biologics, at the next level in the RA medication pyramid, were developed in the late 1990s. Their name stems from the way in which they are synthesized, as genetically engineered proteins derived from human genes. TNF-α inhibitors are the first-line treatment after DMARD failure. Other biologics are not usually considered unless the therapeutic effects of anti-TNF-α are not sufficient. Several targets besides TNF-α are used to combat the complex inflammatory process in RA. Medications include IL-6-blocking agents. Tocilizumab (Actemra®) is one of the most popular exponents of this class. It is often combined with MTX but can also be used as monotherapy in cases of intolerance or contraindications to MTX. Another mechanism of action is found in B-cell inhibitors such as rituximab (MabThera®). First developed as cancer therapy, it showed good effects in RA patients and also proved safe in long-term treatment. Other modes of action are found with T-cell inhibitors such as abatacept (Orencia®) and the IL-1 inhibitor anakinra (Kineret®). This last-mentioned biologic is approved only in combination with MTX.
The newest developments are the bio-similars. These drugs are based on the different action modes of existing biologics. Because the older generation of biologics no longer has patent protection, the bio-similars are copying the mode of action, but the bio-genetic engineering is different and cheaper. With this group of pharmaceuticals, a parallel market is opened, similar to generic drugs.
Even without complete remission, most patients experience a substantial reduction in their physical disabilities, with significant pain relief 2 to 3 months after starting medication. The average cost of biologics is up to $2000 per month, compared with about $70 per month for MTX alone. To justify the high cost, prediction of the individual response to treatment has become a major clinical challenge in RA.
There is some evidence for identifying biomarkers that predict the response to biopharmaceuticals. Identifying and monitoring these biomarkers could enhance the efficacy of medical treatment significantly. On the other hand, the existence of these antibodies may also explain why some people are nonresponders. Knowing these patients’ bio-profiles helps when tailoring a medical treatment plan. There is also some evidence that the effects of biologics diminish over time. One of the reasons for this may be the body’s antibody production against the artificially administered antibodies.
Ideally, the goal of all of these drugs is remission of the disease, which is defined as the absence of disease activity, but with the possibility of return. , , The remission rate of all biologic substances is around 50%, compared with a remission rate of around 30% for MTX alone. Even in remission, however, it is recommended that biologics are continued at a reduced dosage instead of switching to MTX or placebo. ,
The adverse effects observed in RA patients treated with biologics are of concern. , Besides the general adverse reactions, surgeons are especially interested in the patient’s susceptibility to surgical site infections while taking immunosuppressants for RA. Adverse reactions to MTX and biologics can lead to infections by opportunistic pathogens such as atypical fungi and mycobacteria, in particular. An increased risk of malignancies including melanoma is also suspected. However, because the incidence of these adverse reactions is low, most studies lack sufficient statistical power to provide evidence of a strong correlation. The increasing number of patients being treated with this type of medication will result in greater knowledge about the outcomes of long-term treatment. This fact underlines the importance of collecting data from patient cohorts in large-scale studies and ideally in the form of a registry.
The risk of infection while on immunosuppressive drugs is an important discussion among the different physicians involved in the treatment of RA patients. Although several studies and long-standing personal experience show that MTX, even in combination with corticosteroids, does not increase the risk of surgical site infections, there are major concerns about the use of biologics in a perioperative setting. In their review, Polachek et al. concluded that it seems safe to use anti-TNF-α and IL-6 receptor blockers during surgical interventions in RA. They admitted, however, that most studies have small sample sizes, retrospective designs, and different comparison groups. Similar comments were made in a more recent study by Berber et al. In 2011, the Japanese Orthopedic Association Committee on arthritis published data on a large cohort of RA patients undergoing joint arthroplasty. They found a twofold risk of surgical site infection for patients on biologics, although the absolute number of infections (2.1%) was still relatively small. A study published by Scherrer et al. analyzed 48,000 cases of interventions for degenerative osteoarthritis versus 2500 interventions in patients suffering RA. They could show an operation-related infection risk that was two times greater in the inflammatory patients. The highest infection rates were in elbow (4.3%) and foot surgery (3.4%), whereas in hand surgical procedures the infection rate was low at 0.5%. The risk was especially high if the last dose of anti-TNF-α was given less than one administration interval before surgery. In addition, patients with multiple conventional DMARDs had also increased rates of infections. In conclusion, the authors recommended mandatory, careful planning of the discontinuation of the immunosuppressive therapy, especially TNF-α inhibitors with long administration intervals. It was advised to wait at least one administration interval after the last dose before undertaking the planned orthopedic surgery.
Based on these studies and personal experience, there is an informal expert consensus that interruption of biologic therapy is advisable for major surgical interventions such as joint replacement surgery, especially of larger joints. , , There is some debate as to whether corticosteroids and/or MTX should be given in the perioperative phase to reduce the chances of disease flare-up. Interruption of biologics prior to surgery should be managed according to the administration time of the medication. Usually one cycle is omitted prior to surgery. The medication is restarted after the delay of another cycle or once wound healing is assured.
Destruction is nearly universal in patients with RA. Diffuse changes in the wrist and stretching of the scapholunate ligament leads to scaphoid subluxation. This progresses to carpal supination and collapse of the radial wrist, followed by volar subluxation of the wrist joint. Wrist destruction occurs quite early in rheumatoid disease progression. Deterioration of the distal radioulnar joint and ligaments of the TFCC causes the complex itself to weaken. The MCP joints are also affected early. They typically undergo ulnar deviation and palmar subluxation, which eventually leads to dislocation of the MCP joints. The proximal phalanx descends below the metacarpal, making the metacarpal head quite prominent. The MCP joint dislocation makes it difficult for the patient to extend the MCP joint. The decrease in hand volume interferes with a patient’s ability to grasp large objects. Dorsal subluxation of the ulna, combined with radial deviation of the metacarpals and compensatory ulnar deviation of the fingers, induces the common zigzag deformity. Swan neck or boutonnière deformities arise when the tension in the tendons attaching to the PIP and DIP joints becomes imbalanced. Distinguishing between correctable and fixed deformities is a fundamental concept in rheumatoid hand surgery. A patient with a stage I condition, who has synovitis and no deformity, can be treated medically. If a patient has a stage II condition, which consists of synovitis and a passively correctable deformity, then synovectomy can be performed to balance the soft tissue around the joint and slow the progressive joint destruction. Fixed deformities require an altered approach. If the joint is fixed and without articular wear, then it is necessary to remove the synovitis and release the joint. This converts the joint into a flexible deformity, which can be corrected with soft tissue reconstruction. However, if articular destruction is present, then joint replacement surgery or fusion is necessary.
The tendons are also target of destruction in RA patients. Tenosynovitis around the synovial tissue of the tendons limits excursion and causes pain. As a result, the patient may have some passive, but no active, motion in the affected fingers. Good passive motion indicates that the joints are still mobile. If left untreated, the synovial tissue will curtail tendon movement and active motion will diminish. Perpetual invasion of the synovial tissue into the tendon leads to tendon ruptures and significant functional loss.
Clinical observations indicate that the course of disease in patients with RA has become milder during the past decade. Less severe symptoms as well as the diminishing need for orthopedic interventions are most likely the result of the availability of more potent drugs as described earlier in this chapter. There is ongoing debate about whether the type and frequency of surgical intervention has changed significantly in RA patients in recent years. Because the hand is still the main treatment target in these patients (almost 90% have affected hands 10 years after the onset of disease), hand surgery procedures are seen as index interventions.
Several studies indicated a decline in the number of orthopedic interventions in RA patients over the last two decades, whereas the overall number of procedures for osteoarthritic patients has dramatically increased. , Soft tissue procedures on larger joints in RA patients have become rare in Western societies with wide access to new treatment regimens; this is also observed for hand and foot joint interventions. , Yet changes in this trend have been noted, particularly in Japan. Momohara et al. found a decline in large joint replacements whereas the number of wrist and foot interventions gradually increased. There are various explanations for this phenomenon. Firstly, new medications improve patient quality of life, which increases their level of participation in social activities and work. These highly motivated patients place greater demands on both the functionality and appearance of their hands and feet and therefore tend to seek surgical assistance more often. The appearance of the hands and feet is highly valued in societies like Japan, and deformities can lead to social isolation. Therefore the esthetic aspects of these interventions should not be underestimated as highlighted by Waljee and Chung. Another explanation could be the fact that fewer than 50% of patients achieve complete remission. Residual synovitis of one or more joints or tendons in the hands is often observed in these individuals. Because the inflammation process cannot be completely controlled, ongoing destruction of the joints, especially the wrist, is likely. Despite achieving adequate pain relief, inflammation seems to continue and can cause remarkable destruction. This process could, in fact, be termed “silent destruction.” It appears that soft tissue reactions to the available new medications are also unevenly distributed among the different anatomic areas. It is not uncommon to find residual synovitis localized to only certain anatomic regions, whereas other regions are in long-term remission. Why this pattern is seen more often in patients taking biologics is still unclear. One possible explanation might be that different cell mediators are involved in the inflammatory processes, and they may not be distributed evenly. Together with possible intrinsic or extrinsic mechanical factors, there may be differences in the synovial inflammatory processes. This is all speculation and further studies are required to explain these observations, especially in nonresponding patients.
Regular clinical and radiographic monitoring is advisable, even in patients reporting a tolerable to pain-free response to medication treatment. Not only has the number of surgical interventions changed since the introduction of new medications, but also the types of procedures have changed. Previously common procedures such as wrist fusion and MCP arthroplasties have become rare, whereas wrist arthroplasties and PIP replacements are now done more often to treat RA patients. Motomiya et al. reported differences in the clinical and radiographic appearance of patients treated successfully with biologics. Radiographs in the follow-up resembled those from individuals with osteoarthritis rather than with chronic inflammatory disease. This has changed the indications for certain interventions because the positive effect of a medication also has the potential to improve long-term surgical outcome. In particular, interventions such as partial wrist fusion rely on stable inflammatory conditions to achieve optimum long-term results for the patient. Surgical options such as wrist arthroplasty have therefore regained in popularity not only as a result of the development of new implants but also because less aggressive bone destruction ensures better fixation of an implant.
Indications for surgical interventions in RA should be based on evidence combined with the individual patient’s needs. The idiom “too little, too late” is quite relevant to the history of RA hand surgery care. Patients are often unaware of the surgical options for correcting rheumatoid deformities, and rheumatologists do not always refer patients for a hand surgery consultation. For these reasons, hand surgeons often lament that patients present for an evaluation “too little, too late.” This is not only a phenomenon in the United States; an international qualitative assessment indicated that lack of knowledge and communication barriers prevent access to rheumatoid hand surgery care around the world. Alderman and colleagues studied surgical practice patterns for rheumatoid-related fusion, arthroplasty, and tenosynovectomy procedures across the United States. The study reported that the procedure rates varied from ninefold to 12-fold across states, though the rates of various reconstructive procedures were highly correlated within each state. Furthermore, there was minimal association between surgeon density and procedure rates. In other words, the increase in the number of hand surgeons within a geographic region did not increase the rate of rheumatoid hand surgery. These findings led to another study, published in the Journal of Rheumatology, that assessed the association between rheumatologist or orthopedic surgeon density and procedure volume within the Medicare population. Patients who lived in areas with more orthopedic surgeons were more likely to undergo arthroplasty or arthrodesis. Meanwhile, patients in areas with more rheumatologists were less likely to have surgery. These results suggested that in general, rheumatologists do not refer rheumatoid patients for surgical consultation presumably because there is a lack of evidence-based data supporting the effectiveness of surgery. Considering that rheumatologists track patients over an extensive period of time, they often have a more precise understanding of long-term surgical outcomes than surgeons. Therefore it is possible that they consider the benefits of hand surgery to be short-lived.
This same study by Zhong et al. also revealed that African Americans were less likely to have rheumatoid joint surgery than Caucasians. This disparity in care is quite concerning, especially for individuals who live in regions of the country where surgery is underutilized. These nationwide studies are important for determining accurate procedure rates and elucidating the barriers to care. Furthermore, it is incumbent on the hand surgeon to produce high-quality data to justify the effectiveness of surgical intervention for RA.
A landmark survey study, published by Alderman and colleagues in 2003, challenged the lack of consensus in surgical care for the rheumatoid hand. The survey was designed to quantify physicians’ attitudes toward the effectiveness of hand surgery for RA. It also compared hand surgeons’ and rheumatologists’ exposure to each other’s specialty. The findings were quite startling. Hand surgeons were largely unaware of the medical treatment options for RA, and similarly, rheumatologists did not know the surgical options. Even more concerning was that hand surgeons considered the evidence justifying surgery to be excellent, but rheumatologists felt that surgical outcomes research was lacking. With limited evidence, rheumatologists were dissuaded from referring patients to hand surgeons.
Subsequent qualitative assessments indicate that there is a lack of interaction between rheumatologists and hand surgeons in all regions of the world. Kotsis and Chung completed a qualitative study to determine how economic, social, and cultural factors affect rheumatoid hand treatment. Their semistructured interviews with hand surgeons in various countries indicated that the lack of coordination in rheumatoid hand surgery care is an international phenomenon. Again, barriers in access to care are related to the difference in opinions between rheumatologists and hand surgeons regarding the effectiveness of operative intervention. The pattern of care for rheumatoid hand problems also depends on a country’s health care structure, economy, and culture.
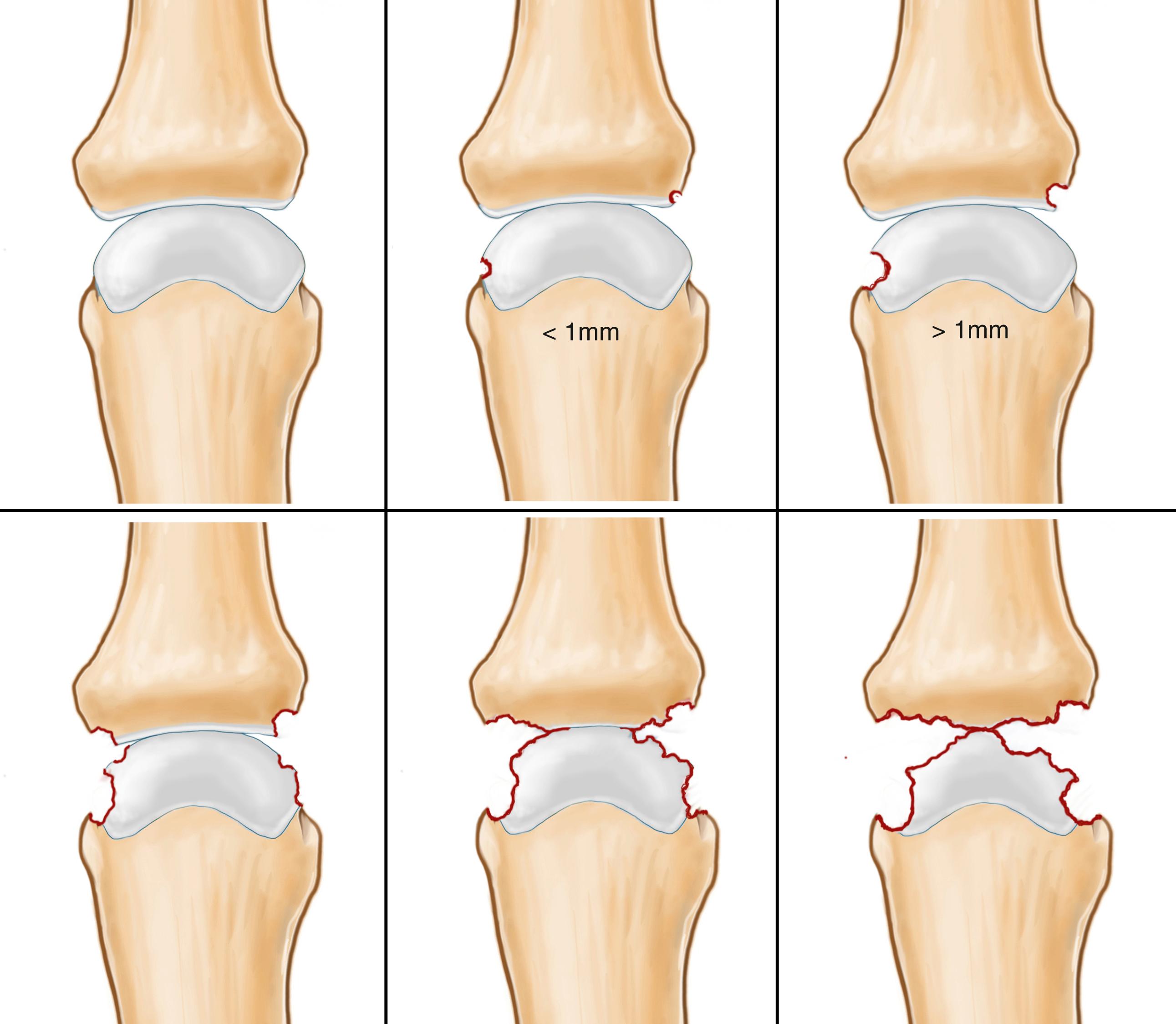
There are two main goals of any classification system used in medicine: to standardize communication among clinicians to group different patient populations and to provide treatment recommendations. In RA, a third dimension is crucial because it is a chronic disease; the anticipation of future disease development must be considered within the framework of a classification system. In 1977, Larsen, Dale, and Eek (often cited as LDE classification) published a grading of RA, which is still widely used due to its simplicity in describing the severity of destruction. It built a score for the most important joints involved in RA and calculates a single general number over all these joints. This was modified in 1995 to facilitate the classification, including osseous and joint space changes. Table 55.2 gives an overview of the grading of joint and bone destruction. Grading has the advantage that it can be applied to different joints and may be used to quantify the severity of the disease with a total scoring of the most often involved joints. This is mainly helpful in the course of the disease to judge the progression of the destruction and its distribution.
| Points | Description |
|---|---|
| 0 | Intact bony outlines and normal joint space |
| 1 | Erosion less than 1 mm in diameter or joint space narrowing |
| 2 | One or several small erosions, diameter more than 1 mm |
| 3 | Marked erosions |
| 4 | Severe erosions, no joint space left but the original bony outlines are partly preserved |
| 5 | Mutilating changes, where the original bony outlines have been destroyed |
In the era before effective medication for RA existed, the orthopedic and hand surgeons often saw patients late, when they had severe joint involvement and destruction on multiple extremities. The timing and sequence of interventions are crucial to offer patients maximum benefit with the minimum number of interventions. Although surgery of the lower limb restores mobility, surgery at the upper limb provides more independence to the patient because personal hygiene and self-feeding depend on a basic function of the upper extremity. Missing lower limb mobility can be compensated more easily than an inability to use the hand. More proximal joints of the upper limb place the hand in space, whereas the fingers are needed to complete the actual task. Therefore at least in the upper limb, as a general rule, proximal interventions come before distal surgical procedures. For example, it is meaningful to mobilize a stiff elbow before starting a complex hand reconstruction. Because lower joint replacement often requires walking stick support, the sequence of upper and lower extremity surgery needs to be evaluated according to the weight-carrying capacity of the upper limb.
The proximal-before-distal concept is also considered when treating the hand. A wrist deformity may influence the posture and function of the fingers and often needs to be corrected first, or at least at the same time as finger reconstruction. This is also true for finger deformities like the swan neck deformity, where the more proximal MCP joints need to be corrected to guide the more distal PIP and DIP joints.
Another discussion is the possible combination of interventions in RA patients. Again, we have to face the fact that these patients will likely have multiple interventions at different locations in their musculoskeletal system. Thus it is often meaningful to combine as many interventions at the same time as possible. We tend to combine wrist and finger surgery whenever the rehabilitation protocol for one is not compromised by the other. It may even be reasonable to use more than one tourniquet time.
In 1979, Souter published his concept of ranking interventions for the treatment of RA. The criteria to evaluate the value of the interventions were elimination of pain, improvement in function, preventive character of the intervention, hazard of complications, and cosmetic improvement. A four-point scale was used with a maximum score of 20. Based on this system, three interventions were clearly ranked as “winner interventions” in the treatment of RA: caput ulnae resection, dorsal tenosynovectomy, and thumb MCP joint fusion.
This concept is still valid because the indication criteria for the three interventions have remained the same to date. There is only one missing dimension that has an important impact, especially for RA patients: the longevity of surgical outcome. The long-term postoperative results are crucial for patients who are likely to undergo multiple operations at different parts of their musculoskeletal system. Table 55.3 summarizes a novel adaptation of this ranking system founded on both scientific evidence and eminence-based opinion. Although this proposed system has an element of personal preference, it may help structure the decision-making process based on specific indications. This is exactly the type of information we need to deliver to patients when considering the surgical procedures to treat RA.
| Surgical Goal | Intervention | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| MCP I Fusion | Caput Ulnae Resection | Tendon Reconstruction | Total Wrist Fusion | Wrist Synovectomy | RSL Fusion | MCP Arthroplasty | PIP Arthroplasty | Total Wrist Arthroplasty | Swan Neck Correction | Boutonnière Correction | |
| Pain reduction | +++ | +++ | ++ | +++ | ++ | ++ | + | +++ | +++ | + | + |
| Functional improvement | +++ | +++ | +++ | ++ | ++ | + | ++ | ++ | ++ | ++ | + |
| Esthetics | +++ | + | ++ | + | + | + | +++ | + | + | ++ | + |
| Prevention | +++ | +++ | +++ | +++ | ++ | +++ | + | − | − | + | + |
| Long-lasting result | +++ | +++ | +++ | +++ | ++ | ++ | + | ++ | + | + | + |
| Complication potential a | +++ | +++ | + | ++ | +++ | ++ | + | + | + | + | + |
| Total score | 18 | 16 | 14 | 14 | 12 | 11 | 9 | 9 | 8 | 8 | 6 |
Timing and treatment priority should always be discussed with the rheumatologist and other treating physicians. Medical treatment may interfere with surgical procedures. It is especially important that a patient in remission does not experience a disease flare-up because of poor planning. Achieving the optimal effects of medical and surgical treatment requires collaboration among all health professionals.
Juvenile rheumatoid arthritis (JRA) is one of the subtypes of the heterogeneous group of conditions, which are called juvenile idiopathic arthritis (JIA). It is characterized by joint inflammation of unknown etiology that lasts at least 6 weeks and starts before the age of 16. JIA contains different disease categories with distinguished manifestations and different pathologic backgrounds. Three major groups of the disease were defined, and further subtypes were described: oligoarticular involvement, polyarticular involvement, and a group with seropositive rheumatoid factor (RF). The amount of joint damage varies substantially within the different groups. Although 10% to 30% joint damage is expected in the oligoarticular group, it increases up to 70% in the polyarticular and up to 80% in the seropositive population. Although JIA is the most common chronic disease of childhood, there is remarkable variation in its incidence and prevalence in different geographic regions and ethnic groups. About 10% of children with JIA have a special subgroup of the disease called Still disease. Patients with Still disease present with fever for at least 2 weeks. Other possible clinical manifestations are a characteristic skin rash, generalized symmetrical lymphadenopathy, enlargement of the liver/spleen, and fluid effusions (e.g., pericarditis). The fever has a typical pattern with one or two daily spikes followed by a return to the normal baseline. Arthritis is often polyarticular and symmetrical in Still’s disease patients but may develop much later than the other systemic symptoms.
The most common form of JIR is the oligoarticular form, present in 50% to 80% of patients. It manifests in four or fewer joints in the first 6 months of the disease. Mainly the lower limbs, especially the knee and the ankle, are affected. Patients are often ANA-positive. The arthritis is asymmetric and the disease often starts early, under the age of 6 years. There is a female predominance and a high risk of iridocyclitis, which can turn into chronic uveitis. Wrist and ankle involvement, together with a high erythrocyte sedimentation rate (ESR), has shown to be a predictor for a more extended course of the disease.
JIR is different from acute rheumatic fever (ARF). ARF is an autoimmune response to a group A streptococcal infection, usually coming from the throat. In addition to the joints, it can affect the heart and the skin (erythema marginatum). The affected joints are often limited to the large joints, starting at the lower limb. The typical age for ARF diagnosis is between 5 and 14 years old. The prognosis of the disease depends on the heart involvement and possible heart valve destruction, especially if several diseases are present.
The diagnosis of JRA is based on exclusion of other joint diseases. Conventional x-rays remain the standard for assessing joint damage. However, ultrasound and MRI are gaining importance in the detection of early disease and quantification of the joint damage. Owing to the different cartilage thickness in these young patients, it is important to compare the findings with age and gender-related normal values. Ultrasound can be used to guide local injection into the joints. Intraarticular corticosteroids rapidly ameliorate the inflammatory symptoms like pain and swelling. In cases of oligoarthritis, injections may prevent the need for systemic medical treatment.
The treatment of JIA patients is always multidisciplinary and should be initiated as early as possible to avoid major joint damage. Hand and occupational therapists play an important role in preventing joint deformities. Selective splinting, mainly at night, may reduce pain. Overall, the majority of young patients with JIA will go into spontaneous or medical-induced remission. Within the group of DMARDs, MTX plays the most important role in medical therapy because of its effectiveness and relatively low toxic profile. Systemic corticosteroids use is mainly restricted to the treatment of the extraarticular manifestations of JIA, particularly in the heart. They can also be used if the patient has a high fever and is unresponsive to NSAIDs. Newer studies show a potential for better outcomes with the use of biologics in patients with aggressive disease. , However, their long-terms effects in these young patients need to be monitored.
The surgical management of JRA is limited to the patients for whom the destruction of joints is too advanced and causes a significant functional deficit or uncontrollable pain.
Special considerations and precaution are needed because these patients often have spine involvement and high cervical spine instability (C1-C2 or subaxial) that complicate safe airway management. In addition, mandibular hypoplasia may cause difficulties for intubation. Similar to adult patients, medical treatment needs to be coordinated so that the danger of infection versus the risk of a disease flare-up is well balanced. Biologics have the same potential for increased infection rate and delayed wound healing in children and adult patients.
Knee and hip involvement are present in about two-thirds and one-third of JRA patients, respectively. Disease in these joints is most often the reason for a patient’s limited mobility and independence. About 10% of patients suffer from severe, disabling lower extremity involvement. Total knee or hip replacement in these young patients is a special challenge because the patients often have abnormally shaped bones. In addition, surgeons have to consider the need for future joint revisions. The bone quality in these joints is often poor, and premature growth plate closure from inflammation leads to trumpet-shaped femurs and tibias.
Even if disease activity is low, many children with JIA present with hand- and wrist-related symptoms and functional impairments. The majority suffers from pain, stiffness, and reduced grip strength. Unlike in adult RA, involvement of the MCP joint is less frequent than the PIP joint. Before the widespread use of DMARDs and biologics, studies showed that radial deviation of the MCP joints was more common in JIA patients than the classic ulnar deviation seen in adult RA patients. Swan neck and boutonnière deformities are rare, but stiffness of the PIP and MCP joints is often present. In general, the reduced mobility of the joints of the hand is typical of JIA.
Surgical treatment in these patients follows the principles of RA surgery in adults. However, there are very few reports on surgical results in JIA surgery for the hand and wrist. Synovectomy, tendon rupture repair, and tendon reconstruction are the most common procedures. Joint fusion and arthroplasty are reserved for older adolescents. Surgery should be postponed until patients reach skeletal maturity, which is typically delayed by JIA. In these patients, the hand bones are osteopenic and brittle, with a very narrow medullary canal. Spontaneous fusion of the joints is often seen, especially at the wrist ( Fig. 55.5 ). Unfortunately, many patients, mainly those with polyarticular disease, have rapid radiographic changes as the JIA progresses. This again emphasizes the importance of early diagnosis and early, aggressive medical treatment.

There are two common sites of RA involvement that may be associated with neurologic problems: the cervical spine and peripheral nerves in the upper limb. This includes the median nerve at the carpal tunnel, the ulnar nerve at the elbow, and the posterior interosseous nerve (PIN) in the forearm. In the cervical spine, the disease and its manifestation range from asymptomatic radiologic changes up to life-threatening situations with gross instability of the upper cervical spine. All levels of the cervical spine may be involved, but the most severe areas are the atlantooccipital joint (C0-C1) and atlantoaxial joint (C1-C2). The inflammation process produces a so-called pannus formation with bone erosions. The ligaments subsequently weaken, leading to subluxation of the mentioned joints. This causes compression of the spinal cord, compromises the vertebral arteries and the spinal nerve roots, and may even provoke impingement of the brainstem. Up to 80% of patients with RA have cervical spine problems. It tends to occur in long-standing disease but can start 2 years after the onset of the disease. Adequate use of DMARDs or biologics can limit this process and prevent cervical spine instability. An atlantoaxial interval (distance between the anterior arch of C1 and the odontoid) of >3.0 mm in adults and 4.5 mm in children is pathologic. The spinal canal can also be compromised, and the risk for cord compression increases if the spinal canal is less than 14 mm in diameter (distance between the posterior arch of C1 and the posterior aspect of the odontoid). Atlantoaxial subluxation can be asymptomatic, and neck pain is nonspecific in these patients. Muscle weakness and sensory symptoms in the upper and lower limbs, with or without sphincter dysfunction, are signs of myelopathy. The most severe form of instability is the vertical penetration of the odontoid into the foramen magnum. This may lead to sudden death due to medullary impingement.
Plain radiographs play a role in the assessment of the rheumatoid cervical spine, especially in patients who are asymptomatic. The classic set includes an anteroposterior and lateral view, a flexion-extension functional view, and a transoral view of the odontoid. However, plain radiographs have their limitations in detecting bone erosions. Even in minimally abnormal plain radiographs, relevant soft tissue problems may be present. Therefore an MRI of the cervical spine should be performed when there is suspicion of unexplained neurologic deficits. In patients with longstanding disease, especially before any major surgical intervention, a cervical spine MRI should be performed to serve as a baseline. This may prevent complications from oral intubation. In cases of confirmed deformity with neurologic deficits, surgical stabilization of the cervical spine should be performed because myelopathy evolves rapidly and can leave residual deficits.
The other source of neurologic problems is compression neuropathy of the upper extremity, namely of the ulnar nerve at the elbow and the median nerve in the wrist (carpal tunnel syndrome [CTS]). A metaanalysis showed an approximately twofold increased risk of developing CTS in RA patients. However, similar risks for CTS were reported for patients with wrist osteoarthritis and gout. , In RA patients, CTS is often caused by flexor tenosynovitis or carpal bone malalignment in unstable wrist conditions. The diagnosis of CTS in RA follows the same principles as in idiopathic CTS. It is mainly based on the patient’s history, the clinical examination, and nerve conduction studies. Because tenosynovitis can cause tendon attrition, ultrasound examination of the wrist is recommended. An MRI is recommended in more severe cases. The flexor pollicis longus (FPL) is usually the first tendon at risk of rupturing because of bony spurs or tenosynovitis. Special attention to this tendon in the diagnostic workup is advisable. Shinoda et al. proposed a grading system of CTS in RA patients. Three groups of patients were categorized based on their clinical signs and amount of tenosynovitis. A subgroup was added to indicate the presence or absence of tenosynovitis ( Table 55.4 ). According to this classification, a possible treatment regimen can be proposed. Patients in group 1a, with mild clinical signs and minimal tenosynovitis, are candidates for conservative treatment. This consists mainly of splinting with or without occupational therapy. Some patients within group 1b have the same clinical presentation but more severe tenosynovitis. It is recommended that these patients receive steroid shots. Patients in group 2a, with clear clinical signs and mild synovitis, are candidates for carpal tunnel release. Patients in groups 2b and 3a/b, with advanced disease and more obvious tenosynovitis, are candidates for open carpal tunnel release with tenosynovectomy. In the daily practice of hand surgeons, most patients with RA and CTS have more advanced disease; open carpal tunnel release with inspection of the tendons and the floor of the carpal canal for compressive bone spurs is recommend. Bony spurs, mainly in the radial corner of the scaphoid, are often found and can be a source of tendon attrition. The bone spurs are resected and local wrist capsular tissue is used to shield the carpal tunnel content. It is important to inspect and palpate the carpal canal in RA patients undergoing carpal tunnel release.
| Group | Clinical Signs a | Tenosynovitis | Treatment |
|---|---|---|---|
| 1a | + | − | Splinting, OT |
| 1b | + | + | Splinting, OT, local steroids |
| 2a | ++ | − | ECTR or minimal open |
| 2b | ++ | + | OCTR |
| 3a | +++ | − | ECTR or minimal open |
| 3b | +++ | + | OCTR |
a Numbness, paresthesia, weakness in thumb opposition, thenar atrophy.
Cubital tunnel syndrome, with compression of the ulnar nerve at the elbow, is much less frequent in RA patients. Rheumatoid synovial cysts arising from the elbow joint are a possible cause of cubital tunnel syndrome. There is no published study that assesses a large series of RA patients with cubital tunnel syndrome.
Another rare condition of neurologic manifestation of RA is PIN palsy. Ishikawa and Hirohata described three cases of PIN palsy in RA patients due to forearm synovial cysts with nerve entrapment at the arcade of Frohse. It is worth mentioning this rare pathology because it is difficult to diagnose. The inability to extend the fingers may arise from extensor tendon ruptures and/or MCP joint subluxation. The diagnostic criteria for PIN palsy are swelling and synovial proliferation at the elbow joint, no sensory disturbance in the hand along the radial sensory nerve territory, positive tenodesis test of the wrist, and lack of substantial deformities of the wrist and the MCP joints. The diagnosis is confirmed with an electrophysiological examination and an MRI of the elbow and proximal forearm.
Besides the CTS, peripheral neurologic conditions in RA patients are rare. The hand surgeon should always consider cervical spine involvement if unclear neurologic signs are present. Due to the development of new medications, synovial-induced compression neuropathies will be seen less frequently. In mild cases, appropriate medications to decrease the synovitis can solve the problem. If the symptoms persist or relevant electrophysiological deterioration is determined, a rather quick surgical decompression procedure is recommended.
Standardized documentation of outcomes is important not only for research but also in clinical routine. The effectiveness of an intervention cannot be quantified unless outcomes are measured across individual patients and patient groups. Such data are the basis for further development and improvements of hand surgical treatments. In addition, socioeconomic consequences of an intervention can be calculated. This is especially important with the increasing focus on health care cost containment. Outcomes data can form the basis for the dialogue with health authorities. Patient-Reported Outcome Measures (PROMs) are used to measure patient-centered outcomes. PROMs can be site-specific, disease-specific, or general quality-of-life measures. The systematic use of information from PROMs leads to better communication and decision making between doctors and patients. It also leads to improvements in patient satisfaction.
In her 2020 paper, Marks gave an overview of the different PROMs and their possible use in assessing hand surgical procedures. A good example for a hand-specific PROM is the Michigan Hand Outcomes Questionnaire (MHQ with 37 items), which also exists in a brief version (bMHQ 12 items). , It is a comprehensive instrument for assessing the effect of treatments for different hand conditions. The widely used Disability of the Arm, Shoulder, and Hand (DASH) questionnaire (30 items) or its short version Quick-DASH (11 items) became popular because of its good measurement properties for different hand conditions. However, it contains items concerning shoulder and elbow function, which influence the score and makes the DASH less hand-specific. A different category of PROMs is used to assess quality of life, which is considered a secondary treatment outcome. Quality-of-life PROMs are mainly used for economic evaluations. The most popular are the EuroQol EQ-5D (5 items), the short form SF-36 (36 items), and the SF-12 (12 items). The EQ-5D asks five questions about mobility, self-care, normal activity, pain, and anxiety and is well investigated for different musculoskeletal disorders. The data from these PROMs are used to calculate quality-adjusted life years (QALYs), which serve as the basis for cost-effectiveness analysis.
The following combination of PROMs would give a comprehensive outcome view of different interventions in RA patients:
Global assessment of the upper extremity PROM: DASH or the Quick-DASH
A hand-specific PROM: MHQ or the brief-MHQ
Quality-of-life PROM: EQ-5D or the SF-36
Studying the outcomes of a common procedure such as silicone MCP joint arthroplasty is critical to bridge the gap between rheumatologists and hand surgeons. Silicone implants were first introduced in the 1960s to restore hand function in patients with MCP joint deformities. Although there were some outcomes studies of arthroplasty procedures, research on silicone arthroplasty in the MCP joint of the fingers was lacking in the early 2000s. A systematic review of patient outcomes following silicone MCP joint arthroplasty supported rheumatologists’ stance regarding the lack of outcomes data. In fact, in 2000 at the time of the review, no study had used a validated health-related quality of life questionnaire to assess outcomes from the patients’ perspectives. Additionally, no studies had a control group, and follow-up time varied across the literature. Although most articles stated that MCP joint arthroplasty was beneficial, existing studies did not use clinical data to justify their claims.
The MHQ was created in 1998 specifically to measure patient-reported outcomes of hand surgery in rheumatoid patients. The questionnaire measures the right and left hand independently because deformities often present differently on each side. It also takes into account the esthetic considerations of rheumatoid patients. Although esthetic improvement is typically not the primary goal of rheumatoid hand surgery, focus groups revealed that many patients are bothered by the stigma surrounding the appearance of RA in the hand. Therefore the MHQ became the first assessment tool to incorporate both esthetic and functional needs, as well as patients’ overall satisfaction. The MHQ has withstood the test of time and is currently used around the globe to measure hand outcomes.
In 2003, Goldfarb and Stern published a chart review study that assessed long-term outcomes of MCP joint arthroplasty in RA patients. Their findings showed that more than 60% of implants fractured over an average follow-up time of 14 years. Nevertheless, the average MHQ satisfaction score was 55/100, which is a rather satisfying long-term result. Although the authors concluded that silicone arthroplasty for MCP joint RA is effective, the overall quality of the data needs more validation. Therefore the MHQ was implemented again in a 2004 prospective study of silicone MCP joint arthroplasty outcomes. The study revealed that traditional measures of functional improvement, such as grip strength, pinch strength, and the Jebsen-Taylor test, did not increase significantly after surgery. However, patient-reported outcomes, measured using the MHQ, improved in the 6-month postoperative period and remained stable 1 year after surgery. These findings indicated that functional measures alone might not reveal the patient’s improvement and satisfaction after surgery. The MHQ, which asks patients about their function, esthetic, satisfaction, and ability to return to work after surgery, is much more pertinent to the overall assessment of the effectiveness of rheumatoid hand procedures.
The MHQ was also carefully assessed for reliability, validity, and responsiveness during the Silicone Arthroplasty in Rheumatoid Arthritis (SARA) clinical trial. SARA was a 10-year, National Institutes of Health (NIH)-funded multicenter study with sites at the University of Michigan, Curtis National Hand Center in Baltimore, and the Pulvertaft Hand Centre in Derby, UK. It was one of the first collaborative studies between rheumatologists and hand surgeons. A paper about the SARA trial, published in Arthritis Care & Research, concluded that the MHQ does have good reliability, with some redundancy of items. The MHQ subscale scores were well correlated with another outcomes tool, and it showed strong responsiveness to clinical change.
A series of papers published across rheumatology and hand surgery journals demonstrated the effectiveness of silicone MCP joint arthroplasty with respect to esthetic improvement and function. Investigators found that hand appearance most closely correlated to patient satisfaction after the procedure. This indicated that a majority of patients had unspoken expectations regarding not only function but also the esthetic needs of their hands. After 6 months of follow-up, surgical patients who began with low overall MHQ scores surpassed nonsurgical patients, who had higher scores to begin with. These scores were maintained up to 3 years postoperatively. Surgical patients also showed significant improvements over nonsurgical patients with respect to ulnar drift and extensor lag. This example shows that different outcome studies are necessary to compare and monitor a treatment effect, especially for a disease as complex as RA.
The wrist is one of the main targets of RA that may deteriorate rapidly, despite the current medical management strategies available. With cumulative incidences of wrist involvement of over 70% and 95%, 3 and 11 years after the onset of the disease, respectively, wrist treatment is key to preserving hand function.
The classic pattern of deformity and destruction involves the radiocarpal and radioulnar joints with destabilization of the carpus caused by attenuation of the extrinsic wrist ligaments ; the result is ulnar-palmar translocation and wrist supination. Three main pathophysiological factors play the greatest role in the process of wrist deformation: cartilage destruction, synovial expansion, and ligamentous laxity. Cartilage thinning is caused by cytochemical effects with continuous degradation. , Bony erosion arises due to synovial expansion, particularly at the site of vascular penetration into the bone such as the radial origin of the Testut ligament. This causes stretching of the retaining intrinsic and extrinsic wrist ligaments with deformation. , One of the essential intrinsic structures—the scapholunate (SL) interval—starts to dissociate and continues to disintegrate the internal carpal architecture. The force vector across the wrist predominately acts in a palmar-ulnar direction. With ongoing destruction of the wrist, surrounding muscles lose their physiologic moment arms to produce deforming forces. ,
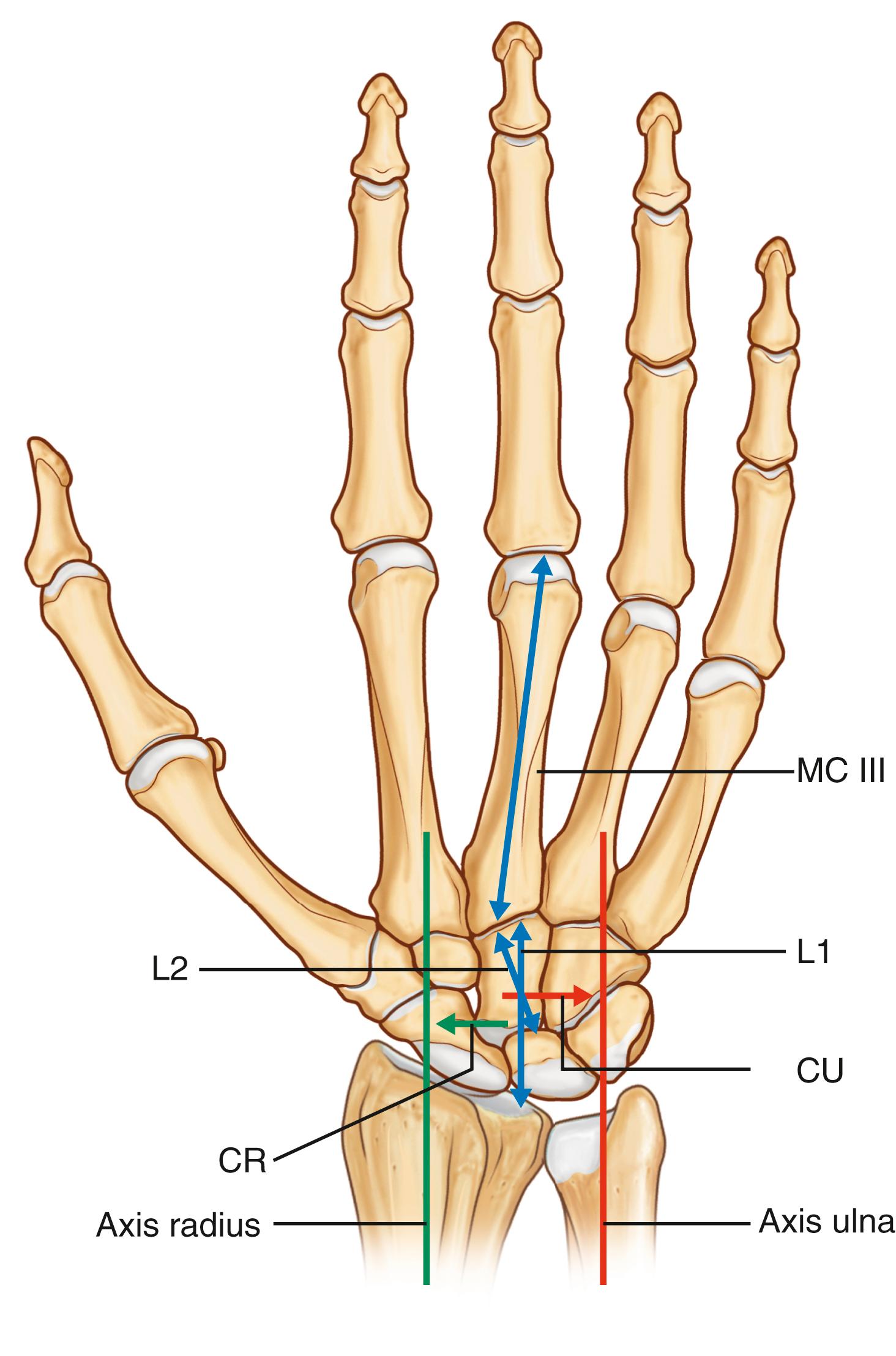
Taleisnik described flexion of the scaphoid through the weakening of the SL ligament with subsequent collapse of the radial column. Additional stretching of the wrist ulnar collateral ligament also attenuates the ulnar column support. These two events ultimately lead to a typical carpal supination pattern. The consequence of carpal supination is the collapse of the radial wrist, which contributes to radial deviation of the metacarpals and accentuates ulnar deforming forces on the fingers at the MCP joints. This concept is based on the early ideas of Shapiro who initially proposed a set of chain reaction events affecting the wrist through to the MCP joints, which give rise to the typical appearance of rheumatoid fingers ( Fig. 55.6 ).

The RA wrist appears to adopt a complex pattern of deformity caused by intrinsic and extrinsic ligament attenuation and disruption. Muramatsu et al. reported a volar flexion of the lunate relative to the scaphoid in 100 early-to-midstage RA wrists; this event was caused by intrinsic ligament laxity, mainly of the SL ligament. This pattern resembles the volar intercalated segment instability (VISI) observed in trauma wrist injuries. At later RA stages, the capitate tends to flex dorsally due to midcarpal instability as a result of extrinsic ligament weakening. This leads to a significant decrease in the carpal height of RA wrists.
The LDE scoring system, , as outlined earlier, remains a suitable instrument for grading the destruction associated with a RA wrist. This classification defines the degree of joint space narrowing and number of erosions localized to the wrist as well as the ulna ( Fig. 55.7 ).
Within the wrist, the pattern of involvement is more complex than in single fingers or foot joints. Hence, the LDE classification neither provides adequate information on the actual disease status nor distinguishes the varying progression states of the destruction and deformity observed in different patients. To quantify the amount of deformation, various radiographic parameters are essential in daily practice, that is, the carpal height ratio (CHR) (as the index for carpal height) and either the carpal translation index (CTI) or ulnar carpal translation (UCT). For CHR, the length of the third metacarpal is divided by the height of the carpus. Normal values range from 0.51 to 0.57. An alternative way in case of missing of the complete third metacarpal bone on x-ray is the division of the capitate length by the height of the carpus. The CTI is calculated by a line from the center of the capitate to the center axis of the ulna divided by the length of the third metacarpal; the normal CTI value lies between 0.27 and 0.33. The UCT is the distance from the center of the proximal capitate to the line bisecting the longitudinal axis of the radius. To compensate for varying hand sizes, the UCT is divided by the length of the third metacarpal. The UCT normal values are 0.07 to 0.11 ( Fig. 55.8 ). Alternate carpal measurements of the RA wrist are often difficult to perform due to advanced destruction and missing anatomic landmarks. A single measurement is often inferior to serial assessments made over time for determining the advancement of destruction as well as and the aggressiveness of the disease.
In 1994, Simmen and Huber described a classification system based on follow-up radiographs, which defines three different types of wrist involvement in RA: ankylosing, osteoarthritic, and disintegrative ( Table 55.5 and Fig. 55.9 ). This classification was subsequently confirmed as a valuable tool for categorizing the possible progression pattern of RA. In an attempt to combine the LDE and Simmen classification systems, Stanley and coworkers created a universal classification of inflammatory wrist arthropathy ( Table 55.6 ). This tool permits the classification of the RA wrist in conjunction with providing treatment recommendations based on the expected development of the disease. Flury et al. showed that a change in CHR of more than 0.015 and/or the increase in ulnar translation of greater than 1.5 mm per year is indicative of an unstable type III wrist. With these criteria, it is possible to classify most wrists, although some cases of type II involvement with a shift from stable to unstable has been observed during the course of the disease. Zangger et al. investigated the applicability of this classification system in patients with early RA. Intra-observer agreement was good with some consistency over time, yet this classification could only be applied to the radiographs of about 50% of patients with early disease.
| Type | Characteristics | X-Ray Characteristics |
|---|---|---|
| I | Spontaneous tendency for ankylosis | Bone fusion |
| II | Osteoarthritic destruction pattern | Space joint narrowing |
| Preservation of bone stock | ||
| Stable wrist condition | ||
| III | Disintegration of the wrist | |
|
Ligamentous destabilization | Ulnar drift; carpal bone dissociation |
|
Bony disintegration/mutilans type | Bone resorption; joint disintegration |

| Type of the Disease | |
| A: Destructive type | Slow progression type without significant OA |
| B: Reactive type | Slow progressive type with marked OA |
| C: Ligamentous type | Progressive soft tissue disruption |
| D: Mutilans type | Progressive bony destruction |
| E: Juvenile type | Spontaneous intercarpal ankylosis |
| Stage of the Disease | |
| I | Early, erosions ± reducible translation |
| II | Translation/subluxation, nonreducible ± radiocarpal OA |
| III | + midcarpal joint loss |
| IV | Disorganized wrist ± significant bone loss |
Although such classifications have their limitations, they help provide discussion points for both the patient and physician when considering the indications for treatment as well as the treatment options available. In addition, with the new type of medication, especially the biologics, the course of the disease may be radically influenced, especially if treatment is started early.
Although standard radiographs of the wrist are still mandatory for RA patients, these images have the disadvantage of only revealing established and more advanced destruction; joint space narrowing and erosions are late and unspecific events. Therefore MRI with intravenous gadolinium application and high-resolution power Doppler sonography are more sensitive techniques, particularly in defining an early disease state. Diagnosis, staging, and monitoring of RA in the hand are important steps in the management of affected patients. MRI has an important role in the management of RA, even during remission phases. , Subclinical inflammation can be detected and is pertinent in the prognosis of disease development with a high predictive value. In addition, MRI allows the surgeon to visualize the extent of soft tissue damage to better plan imminent surgery as well as obtain further information for optimizing the timing of further interventions. For example, MRI provides important information about the level of disease activity in surrounding tendons, which allows the surgeon to plan an intervention optimally in patients with wrist problems and established tendon ruptures.
Ultrasound is gaining popularity in the daily clinical practice of hand surgeons and is already a routine diagnostic tool for the rheumatologist. Although this technique requires extensive experience from the examiner, it facilitates real-time imaging of fluid and inflammation masses and detects tendon irregularities with a high sensitivity. Furthermore, ultrasound can be used to improve the accuracy in applying therapeutic injections around tendons or within intraarticular spaces.
The indications for surgical treatment of the rheumatoid wrist are based on the following criteria: pain, functional disability, deformation including its esthetic aspect, and possible future development of the disease. The intensive use of current modern medication often provides notable pain relief and greatly improves the quality of life of these patients. Nevertheless, as described earlier in this chapter, the destruction induced by subclinical inflammation persists, and is commonly known as the “silent” destruction. To prevent ongoing damage to joints and tendons, prophylactic surgery may need to be considered even for patients with minor pain and disturbances. As early as 1975, Millender and Nalebuff reported on the concept of preventive surgery in RA patients. Okura et al. observed a positive patient-reported, long-term effect of surgical interventions on various joints including the elbow, wrist, and hand; 10 years after the surgical procedure, 85% of the patients reported a better wrist condition than prior to surgery.
The two main concerns associated with the rheumatoid wrist are tendon ruptures and irreversible joint damage. There are a number of key risk factors in determining the possible occurrence of a relevant complication of the inflammation process. This includes long-standing disease (>5 years), persistent synovitis (>1 year), and a LDE stage 4 or higher wrist. If the carpus is subluxated with an ensuing prominent ulna, and this is associated with local synovitis of the ulnar tendons and/or distal radioulnar joint, surgical intervention should be considered. Three dimensional-CT scans can help improve the ability to predict the risk of extensor tendon rupture around the ulnar side of the wrist.
The first attempt to standardize a surgical procedure to treat rheumatoid wrists was introduced by Backdahl. He described the term “caput ulnae syndrome” and recommended the surgical resection of the ulnar head together with a synovectomy of the wrist extensor tendons to prevent tendon rupture. This concept worked for a significant number of patients; however, continued carpal collapse was reported. Seven years after dorsal wrist synovectomy and distal ulna resection, Thirupathi et al. observed adequate pain relief, stable tendon conditions, and preserved functional range of motion in 38 wrists. Nevertheless, carpal collapse and translocation could not be predicted by preoperative x-rays and the progression of carpal dislocation continued in a linear fashion throughout the follow-up period. Similar results were noted by Masada et al., who recommended distal ulnar resection only for patients with a stable wrist configuration. Ishikawa and coworkers treated 43 patients with a distal ulna resection and wrist extensor synovectomy. Significant long-term acceleration of ulnar translation was observed in treated compared with the untreated wrists, whereas carpal collapse and palmar subluxation progressed less frequently with the untreated opposite wrist. As such, a stabilizing procedure was recommended to prevent ulnar carpal shift.
The classic interventions used to stabilize rheumatoid wrists are partial wrist fusions.
The challenge in routine practice is to consider those patients with little or no wrist pain who seek advice from the hand surgeon for their finger deformities. As outlined earlier, it seems likely that wrist deformity influences the outcome of finger interventions. In an analysis of 381 MCP finger joint arthroplasty patients, Trail et al. found, among other factors, better long-term results when concomitant wrist alignment was performed. Beyond this study, there is little information about the outcome of combined wrist and finger interventions and how they influence one another.
Overall, the indication for RA wrist surgery is mainly based on clinical and radiographic findings. When relevant risk factors for future deterioration are present, the indication for wrist stabilization should be given precedence even for oligosymptomatic patients.
Surgical procedures for the radiocarpal and radioulnar joints are either preventive or reconstructive. Preventive procedures include synovectomy of the radioulnar and radiocarpal joints, balancing of the wrist extensors, and tenosynovectomy. Reconstructive surgery includes distal ulnar excision, reconstruction of the ulnocarpal ligamentous complex, radiocarpal joint arthroplasty, partial wrist fusion, and total wrist arthrodesis.
Soft tissue procedures of the rheumatoid wrist can be classified as follows:
Removal of inflammatory tissue: joint and tendon synovectomy
Realignment procedures of the wrist
Tendon transfer and reconstruction
The indications for wrist joint synovectomy are not clearly established. To date, there is no evidence conclusively demonstrating that synovectomy changes the natural course of RA. In addition, total synovectomy is impossible to perform because the wrist is a multiarticulated, complex joint. The indicators used for diagnosing wrist synovectomy vary among hand surgeons. Some recommend several months of conservative therapy before synovectomy. Flatt advocated early synovectomy because of the rapid joint destruction that can occur when active synovitis does not respond to medical therapy. Hindley and Stanley found relative sparing of the midcarpal joint and suggested that early synovectomy may prevent progression. Further studies have shown that synovectomy can provide significant pain relief, even for patients with advanced disease. Synovectomy, in some cases, is an adequate alternative to wrist salvage, even in the case of relatively advanced destructive changes. Wrist synovectomy may be more effective and durable in the era of biologics and disease-modifying agents.
Radiocarpal and radioulnar joint synovectomy can be performed either with an open technique or arthroscopically. Open synovectomy is usually combined with extensor tendon synovectomy, tendon repair, or reconstruction and surgery at the distal radioulnar joint (DRUJ), the latter typically involving ulnar head resection. In addition, this open procedure seems to have a certain denervation effect, which involves the reduction of sensory nerve fiber density in the synovial tissue. However, open wrist synovectomy has the disadvantage of creating extensive scarring at the wrist capsule, which is often associated with decreased postoperative range of motion, especially in flexion. Conversely, arthroscopic synovectomy has the advantage of faster recovery and less scar-inhibited wrist mobility. With the reduction of wrist synovitis and the application of novel biological medications to treat tendons, the arthroscopic technique yields benefit for cases of isolated wrist and DRUJ synovitis.
The wrist is exposed with a straight, longitudinal incision as described for dorsal tenosynovectomy. Partial denervation involves resection of the terminal branch of the PIN, which is consistently located on the floor of the fourth dorsal compartment, deep to the extensor tendons.
A transverse or “U”-shaped incision is made in the wrist capsule and the distal-based flap is elevated to expose the wrist and intercarpal joints. This capsular flap is used to permit reefing of the redundant stretched dorsal capsule for joint stabilization. Synovium is usually seen bulging from the proximal and distal carpal rows. Traction applied to the hand distracts the joints and allows the synovectomy to be performed with a small rongeur. A small, blunt periosteal elevator can be used to ensure better exposure within the joint. Periarticular erosions are treated by curettage. The synovium is removed from the area between the triquetrum and triangular fibrocartilage.
The DRUJ is exposed through a longitudinal incision proximal to the triangular fibrocartilage. The forearm is rotated to provide exposure as the synovectomy is performed. Bone spurs are removed from the distal end of the ulna and periarticular erosions are also treated by curettage. After the synovectomy is complete, capsular incisions are closed with interrupted nonabsorbable sutures. Closure is performed with the forearm in supination to minimize the tendency for the ulna to subluxate, and to allow tighter closure of the DRUJ capsule. Tendon rebalancing and dorsal tenosynovectomy are performed, if necessary. The dorsal retinaculum can be divided into two parts, whereby the distal section is used to construct a floor for the extensor tendons and reinforce the wrist capsule to a degree. The proximal part can be used to form the anatomic extensor tendon tunnels.
A bulky compression dressing is applied, and the wrist is placed in a neutral position with a splint. Some physicians prefer the sugar-tong splint with the forearm in full supination to obtain more stability at the DRUJ. The splint is worn for approximately 3 weeks and removed thereafter, followed by physical therapy consisting both active and progressive passive forearm and wrist range-of-motion exercises, as needed.
The length of postoperative splinting depends on the extent of preoperative wrist ligament laxity and the degree of ligament disruption found at the time of surgery. The greater the laxity, the longer the wrist needs to be splinted postoperatively. Splinting for 4 to 6 weeks may be necessary to ensure sufficient capsular healing with stability. The range of flexion and extension after surgery varies, but averages around 30 to 40 degrees each.
Volar wrist synovectomy can be done when flexor tenosynovectomy is indicated. Volar wrist synovectomy, in conjunction with wrist flexor tenosynovectomy, to prevent destruction of the deep volar ligaments and secondary rotation of the scaphoid, has been advocated by some groups. When present, volar wrist synovitis manifests as bulging of the volar capsule. The skin incision described for volar tenosynovectomy is used; that is, a transverse incision is made over the bulging volar wrist capsule. Traction is applied to the hand, and the synovium is removed from the volar portion of the wrist with a rongeur. Postoperative management is the same as that described for dorsal tenosynovectomy.
Arthroscopic debridement is conducted in a similar manner to a standard wrist arthroscopy using a 2.9 mm, 30-degree arthroscope and motorized shavers ranging from 2.0 mm to 3.5 mm. Some surgeons use a radiofrequency probe to remove the synovial mass. Through the standard 3 to 5 and 4 to 5 portals, the radiocarpal joints are debrided. The 1 to 2 and 6 U portals are used for better viewing of the DRUJ. Midcarpal joints are approached via both midcarpal radial and ulnar portals. An accessory STT portal is often used to complete the debridement step. The DRUJ can often be approached through a hole in the triangular TFCC, where synovial tissue often penetrates into the ulnar-carpal space. The classic DRUJ portal often provides a limited view and surgical working space.
To rebalance the rheumatoid wrist and provide additional stabilization, additional soft tissue procedures may be done in combination with synovectomy and possible radioulnar surgery. There are two classic tendon procedures for treating RA wrists: the extensor carpi radialis longus (ECRL) to extensor carpi ulnaris (ECU) transfer and the ECU tendon relocation. There is some evidence that ECRL to ECU transfer in combination with synovectomy provides good pain relief and prevents further radiocarpal destabilization. This procedure alleviates the deforming force from the ECRL tendon on the radial side of the wrist; it also aligns the wrist because the volar subluxation of the ECU tendon is modified from a wrist-flexion to a wrist-extension function. The prerequisite for this procedure is a reducible radiocarpal joint dislocation with an intact radiocarpal joint not more advanced than Larsen stage 2. Although the benefits of this procedure may be temporary, it is an intriguing option for patients with a flexible wrist deformity that still can be corrected with soft tissue reconstruction techniques.
After dorsal tenosynovectomy, distal ulna excision and ligamentous reconstruction are performed, and the ECRL is divided at the base of the second metacarpal. This can be done either via a separate small incision or the primary surgical incision. The tendon is rerouted dorsal to the finger extensors and sutured into the repositioned ECU tendon. Upon transfer completion, the wrist should be maintained in a neutral position in the coronal plane (radial and ulnar deviation) with a slight tendency for overcorrection. The wrist is splinted in the corrected position for 4 weeks before beginning rehabilitation exercises.
During any surgical procedure on the dorsal aspect of the wrist, the ECU tendon should be released from its volar subluxated position and repositioned in its normal dorsal position. If the extensor retinaculum has been reflected radially, a strip of this fascia can be split and looped around the ECU to hold the tendon dorsal to the axis of wrist flexion, similar to the sling procedure used to correct ulnar subluxation of the ECU tendon using a slip of the extensor retinaculum that is raised radially and based on the septum between the fourth and fifth compartments. Alternately, when the retinaculum has been reflected radially and ulnarward, the ulnar portion can be placed deep to the ECU and used as a sling to hold the tendon in the corrected position. If there is still the tendency for the tendon to subluxate, it can be sutured to the capsule over the dorsal aspect of the carpus.
Tenosynovitis—in the context of RA—occurs frequently and may manifest months before signs of joint involvement are identified. , Although there has been a long-standing awareness of spontaneous tendon rupture, Vaughan-Jackson drew attention to the importance of tendon alterations in 1948 with reference to two cases of spontaneous extensor tendon rupture at the level of the DRUJ. This was followed by an increasing number of reports on the pathology of the tendons in RA. Synovial involvement of the extensor tendons has been observed more frequently than for the flexor tendons in the hand. Of note, the abductor pollicis longus (APL) and extensor pollicis brevis (EPB) are rarely affected in the region of the first tendon compartment.
The clinical picture of rheumatoid tenosynovitis depends on its localization. In the majority of cases, tenosynovitis causes pain whereby spontaneous tendon rupture can be an entirely painless event. Primarily, synovitis tends to only affect the mobile tissue of the tendon sheath. During the course of the disease, the tendon is infiltrated and ultrastructural changes take place in the tendinous tissue, which may include ischemic necrosis and may lead to loss of function with eventual rupture, even without additional mechanical irritation.
The treatment options for rheumatoid patients with tendon ruptures are fusions of various joints and tendon transfers. There are differences between tendon transfers performed in rheumatoid and nonrheumatoid patients. For a rheumatoid patient, (1) the joints to be moved by the transfer may be stiff or unstable, (2) the bed through which the transfer passes may be scarred or irregular and compromise tendon excursion, (3) the tendons to be transferred may have been weakened, and (4) if the wrist, MCP, or PIP joints (or any combination of the three) are stiff or deformed, the tenodesis effect of wrist motion or the complementary motion of the MCP and PIP joints cannot be relied on to enhance the performance of the transferred tendons. These factors must be considered carefully when planning tendon transfers to reconstruct rheumatoid tendon ruptures.
Tendon reconstruction includes tendon grafting and tendon transfer. Direct repair is rarely possible in RA patients because the inflammatory process produces extensive tendon damage. Despite the overall good response of patients to new medications for the treatment of tendon synovial inflammation, either single tendon involvement or, in nonresponders, multiple tendon ruptures are still seen. It is suitable to perform a gadolinium MRI of the wrist in cases of tendon ruptures; this procedure helps to detect ongoing disease and additional tendon attrition for planning the timing and type of surgical treatment.
Although reconstruction with a free tendon graft may be problematic due to the risk of secondary adhesions, good outcomes have been described for this technique. Possible tendon graft donors are the palmaris longus, strips of ECRL or extensor carpi radialis brevis (ECRB), and also the plantaris tendon and extensor tendon of the fourth toe. Intraoperatively, the grafts should be maintained under relatively high tension and stabilized by weave sutures to compensate for the anticipated postoperative elongation of the muscles. If muscle fibrosis with limited contractility is already present and tension is too high, but the extensibility of the fingers is good, functional restriction may result due to loss of finger flexion. Because atrophy and muscle fibrosis start soon after the rupture, the time to graft reconstruction should not exceed 12 to 20 weeks after tendon rupture. Nakamura and Katsuki recommend that tendon grafting should not be performed if there is a contracted proximal musculotendinous unit and passive excursion of less than 2 cm is present.
With regard to the technical aspects, it is important to excise the scar tissue until viable tendon is visible. It is critical that the surgeon excise the tendon ends until normal tendon is encountered. Suturing the scar tissue, rather than tendon, in the tendon juncture is a common mistake that will ultimately lead to tendon rupture because of the lack of tenocyte union.
For tendon fixation, the Pulvertaft technique is traditionally used. Here, the two tendons are interwoven with three passages displaced at 90 degrees to each other. A good alternative is the side-to-side repair introduced by Friden and Lieber, which involves inserting the transferred tendon through one incision in the tendon requiring repair, four cross-stitch running sutures back and forth down both sides, and one double-loop suture at each tendon free end. The advantage of this technique is not only the greater mechanical strength achieved compared with that of the Pulvertaft repair but also the diminished bulk with better appearance as well as the likelihood of less tendon adherence ( Fig. 55.10 ).
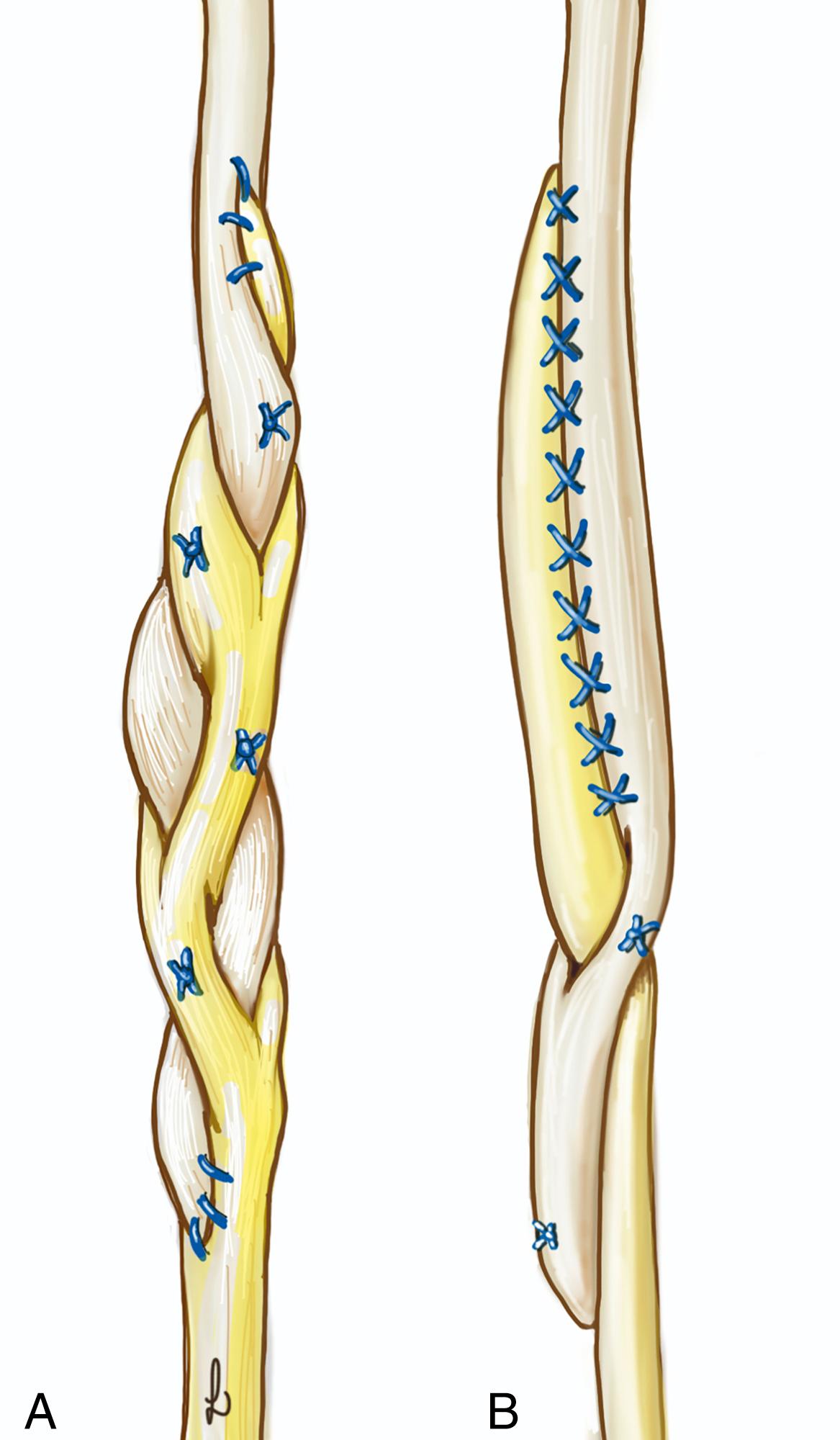
Extensor tendon rupture is a common occurrence in patients with RA. Synovitis invades and frays the tendon fibers, leading to tendon weakness. Additionally, volar subluxation of the radius causes the dorsal-riding ulna to rub against overlying extensor tendons. Attritional rupture occurs when the eroding ulna penetrates the DRUJ capsule. The combination of weakened tendons from synovitis and bone spur development over the distal ulna triggers tendon rupture starting at the little finger. Rupture progresses to the other fingers due to the ulnarly moving tendons.
Patients can often still extend the little finger to a neutral position despite tendon rupture because the juncturae tendinae links the little finger to the ring finger extensor tendon. Therefore the occurrence of tendon rupture often remains undetected until the ring finger extensor tendon fails ( Fig. 55.11 ). This causes a noticeable functional problem because the patient can no longer extend the ring and little fingers. Patients often remember the precise moment when they lost function of the two ulnar digits. An examination reveals synovitis protruding distally and proximally through the tight extensor retinaculum, forming an hourglass appearance.

Current teaching advocates for prophylactic synovectomy to be performed when synovitis is uncontrolled after 3 to 6 months of optimal medical management. As previously stated, a gadolinium MRI can help determine the timing and surgical procedure, which requires planning. Synovectomy is necessary to remove the invading synovitis and prevent attritional rupture. If the patient complains of nonspecific pain over the DRUJ or crepitus of the extensor tendon over the distal ulna, distal ulna resection is necessary along with the synovectomy.
In case of rupture, the distal tendon juncture is identified, and again one must excise the scar tissue until viable tendon is visible. Suturing the scar tissue, rather than tendon, will ultimately lead to tendon failure. It is also important that the surgeon displays the entire length of the tendons to the musculotendinous juncture to ensure all synovitis is removed. It is not uncommon for surgeons to overlook the proximal synovitis and instead focus solely on the tendon rupture site. If the frayed proximal tendon is not repaired, subsequent tendon ruptures are likely to occur.
One of most difficult tasks is the tensioning of the different transfers, especially if one motor serves several targets. As a rule of thumb, undertensioning is common, but it is almost impossible to achieve overtensioning of the tendon; this means that overtensioned transfers can nearly always be stretched with therapy, whereas a “too loose” transfer can never shrink postsurgery.
With a mobile wrist, the tenodesis effect can be used to judge the amount of tension required for correction. This degree of tension must be sufficient so that the fingers are maintained in complete extension when the wrist is flexed moderately, and the MCP joints flex only 20 to 30 degrees when the wrist is extended moderately. It is definitively more challenging to set the correct tension in an already fused or stiff wrist. In these cases, the surgeon should concentrate on following the natural cascade of the fingers, while considering that the reconstructed rays should be slightly more extended than the adjacent fingers.
If applicable, the wide awake local anesthesia no tourniquet (WALANT) anesthesia technique simplifies the task of judging the correct tensioning. After tendon suturing is complete, the patient is asked to extend their fingers actively; if there is a lag in extension, tendon tension can be adjusted at this time.
Table 55.7 summarizes the recommended repairs and tendon transfers for the different rupture scenarios.
| Rupture | Side to Side | Transfer | Alternative |
|---|---|---|---|
| EPL | − | EIP EPB |
EPB (if EIP is needed for ulnar fingers) |
| EDQ | EDQ to EDC 4/5 | EIP to EDQ | |
| EDQ + EDC 5 | EDQ/EDC 5 to EDC 4 | EIP to EDQ/EDC 5 | |
| EDQ + EDC 4+5 | EDC 4 to EDC 3 (and transfer) | EIP to EDQ/EDC 5 | |
| EDQ + EDC 3+4+5 | EDC 3 to EDC 2 (and transfer) | EIP to EDQ/EDC 4 and 5 | |
| EDQ + EDC 2+3+4+5 | EDC 3 to EIP (if present) (and transfer) |
FDS 4 to EDQ/EDC 4 | FDS 3 to index and EDC 3 ECRL/ECRB |
| All tendons to all four fingers | – | FDS 4 to EDQ/EDC 4 andFDS 3 to EDC 2+3 /EIP | ECRL/ECRB |
| Thumb and all four fingers | – | FDS 3 to EPL/EIPand FDS 4 to EDC 3-5 | – |
Although rupture of a single finger extensor can affect any finger, the small finger is most frequently affected. The extent of active extension loss at the MCP joint of the small finger depends on whether the extensor digit quinti (EDQ) only or both the EDQ and extensor digitorum communis (EDC)-5 are ruptured. An isolated rupture of the EDQ tends to cause only slight loss of active extension at the MCP joint, and it almost always remains unnoticed. The relevant function test requires the patient to extend the small finger with the fist clenched; this blocks the action of the EDC-5. An extension deficit of 30 to 40 degrees is observed with a dysfunctional EDQ.
Reconstruction of the EDQ tendon is most easily achieved by end-to-side suturing of the distal tendon stump to the adjacent tendons of EDC-5 or EDC-4. Correct initial tensioning is essential for a good outcome. The tenodesis effect tested intraoperatively during movement of the wrist must allow all four fingers to be moved simultaneously.
Another possibility for primary tendon transfer is to place the extensor indicis proprius (EIP) tendon into the tendon stump of the small finger extensors (EDQ/EDC-5). Before planning this procedure, the integrity of EDC-2 must be assessed so that the extension of the index finger is not jeopardized. The EIP tendon is located on the ulnar side of the EDC-2 tendon and both pass through the fourth extensor compartment with the EDC tendons. Because the muscle belly is situated very distally, it can easily be differentiated from the EDC tendons. Intraoperatively, the small finger should achieve somewhat greater extension at the MCP joint than the ring finger. Complete passive fist closure should be possible with the wrist in 30- to 40-degrees extension.
If there are two extensor tendon ruptures, commonly localized to the small and ring fingers, side-to-side suturing of both distal tendon stumps to the intact neighboring tendon can be inadequate. Firstly, the strength of the middle finger is hardly sufficient to achieve full extension of the three ulnar-sided fingers; and second, the stump of the small finger tendon is often too short for this reconstruction technique. In this case, tendon grafting or preferably EIP transfer can be performed to restore extension to the ring and small fingers ( Fig. 55.12 ).
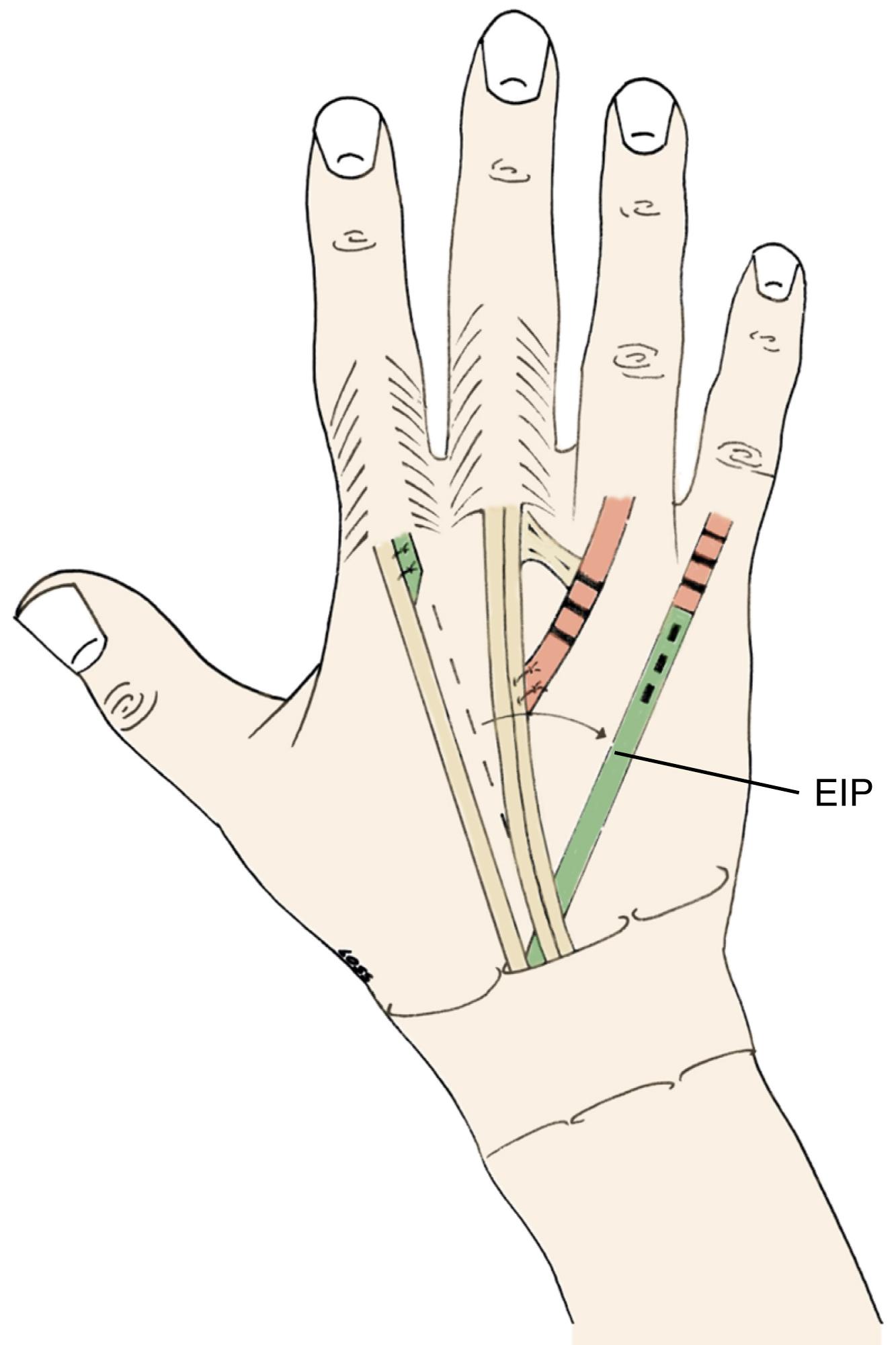
It is important to consider the functional needs of a patient with middle, ring, and little finger tendon ruptures. In the case of a low-demand patient, it is suitable to suture the ruptured distal middle finger tendon to the EDC of the index finger and transfer the EIP to the ring and little fingers. The two tendons from the index finger will serve as the motor for all four digits ( Fig. 55.13 ). Alternately, a patient either with high demand or with a small tendon caliber of the index finger may benefit from a subcutaneous transfer of the middle finger flexor digitorum superficialis (FDS) tendon to repair all three fingers. This is not a synergistic transfer, because a finger flexor tendon is used to repair the extensor tendons of the fingers. However, patients will eventually learn to activate the tendon transfer appropriately. The FDS tendon has a long excursion of approximately 70 mm, which can modulate the tendon transfer with greater ease.
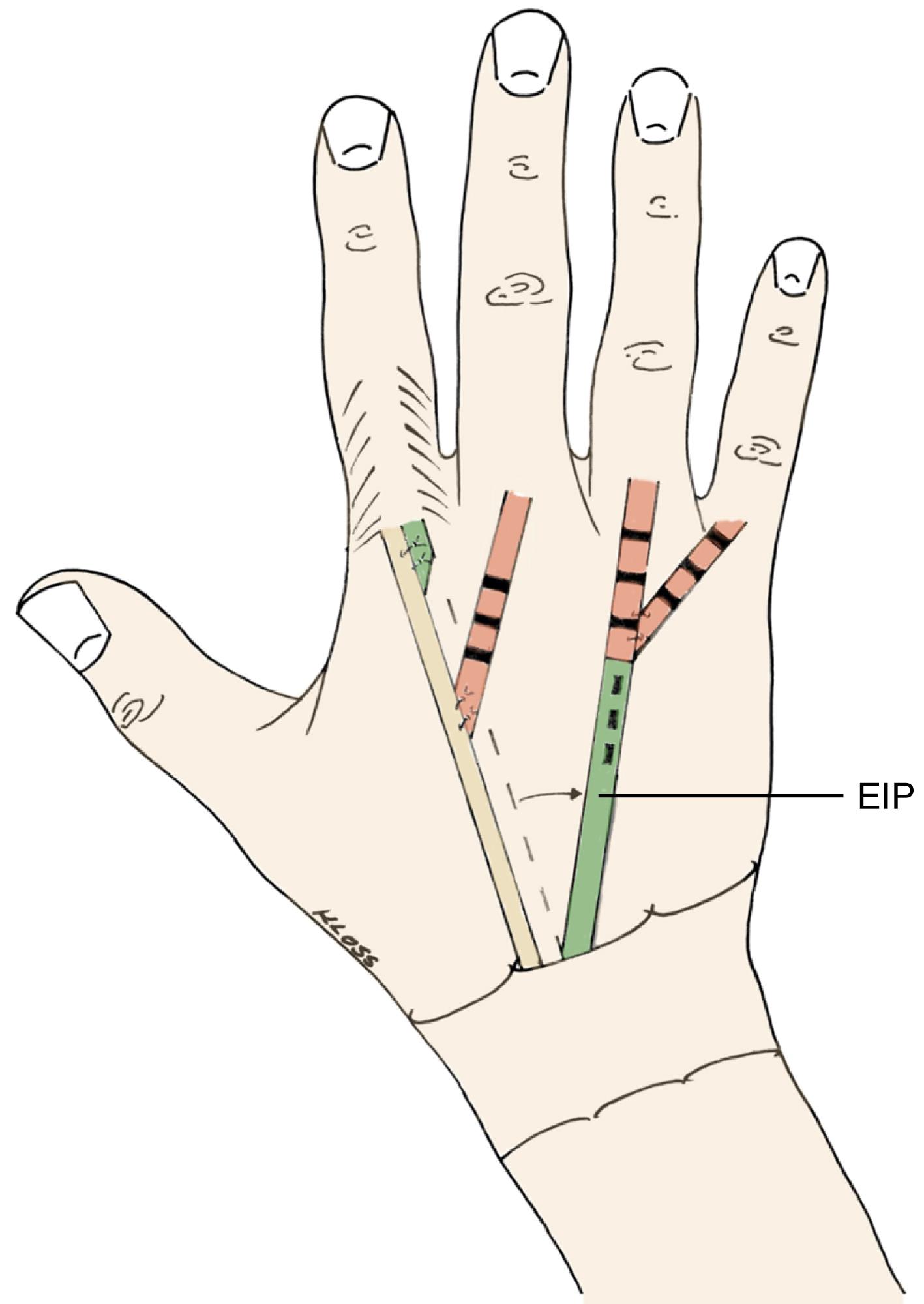
Transfer of the wrist extensors has also been described. Yet transfer of the ECU is less appropriate because this tendon is an important wrist stabilizer, and its removal would favor radial rotation of the wrist as observed in rheumatoid patients. Moreover, the wrist extensors have smaller gliding amplitude than the finger extensors; this limits functional outcome and results in insufficient flexion or extension after transfer.
If initial ruptures of the ulnar extensor tendons are left unrepaired, the radial tendons will migrate over the arthritic distal ulna and also rupture. Repairing ruptures to all extensor tendons is a difficult undertaking. In the case of rupture to all finger extensors, a bridge graft may be useful to repair all four long finger extensors. Here the same rules apply as previously outlined with regard to the time of operation and donor tendons. In the decision process for reconstructing this type of mass rupturing, it should be taken into consideration that the likelihood of tendon insufficiency and tendon adhesions increases with the increasing number of grafted tendons. Primary intercalated or “bridge” grafts can be useful, particularly for triple tendon ruptures. The palmaris longus tendon or, if the wrist is fused, one of the wrist extensors can be used for the graft. The dorsal wrist incision is extended proximally, and the proximal stumps of the ruptured extensor tendons are located and dissected free from scar and adherent soft tissue. The tendon with the best condition is selected as the motor if satisfactory excursion is available. The bridge graft is inserted between the proximal and distal tendon ends by using an interweaving technique. The graft should be positioned tightly because the muscle will gradually stretch postoperatively. One also needs to leverage those proximal tendons that are not used to serve as tendon grafting material. The ability to match the needs of the patient by using one proximal motor to power two fingers yields additional tendon grafting materials from the ruptured proximal tendons. Bora and associates reported excellent functional results (MCP joint motion: 10 to 75 degrees) in a long-term follow-up study where the palmaris longus was used as a “loop” tendon graft to bridge the extensor tendon defect after multiple tendon ruptures.
When choosing a tendon transfer, only tendons from the volar side are clearly available. A similar technique as described for the reconstruction in radial nerve palsy can be used for these patients. It is important to determine the length of the FDS tendon necessary to reach the ruptured distal tendon. Typically, the FDS tendon is harvested at the level of the A1 pulley and retracted through the carpal tunnel to the forearm. Thereafter, it is transferred subcutaneously to reach the dorsal hand.
The FDS tendons of the ring and middle fingers are detached from the distal palm and passed through the interosseous membrane from the flexion to extension side of the hand. Nalebuff and Patel modified this technique in a way that the superficialis tendon is not threaded through the interosseous membrane but passed subcutaneously radial around the radius in a dorsal direction ( Fig. 55.14 ). Although ulnar-sided transfer route is also possible, it is not recommended because it might accentuate ulnar drift of the wrist and fingers. With this technique, up to three extensor tendons can be motorized by one superficialis flexor tendon. However, if there is rupture to all the long finger tendons, then transfer of two superficialis flexor tendons is required. Extension of the ring and middle fingers can be restored with the FDS-4 tendon, and extension of the index and middle fingers can be reconstructed with the FDS-3 tendon. It is important that the integrity of the relevant deep flexor tendons (i.e., FDP-3 and FDP-4) is assessed prior to detachment to ensure that excision will not lead to finger flexion insufficiency.
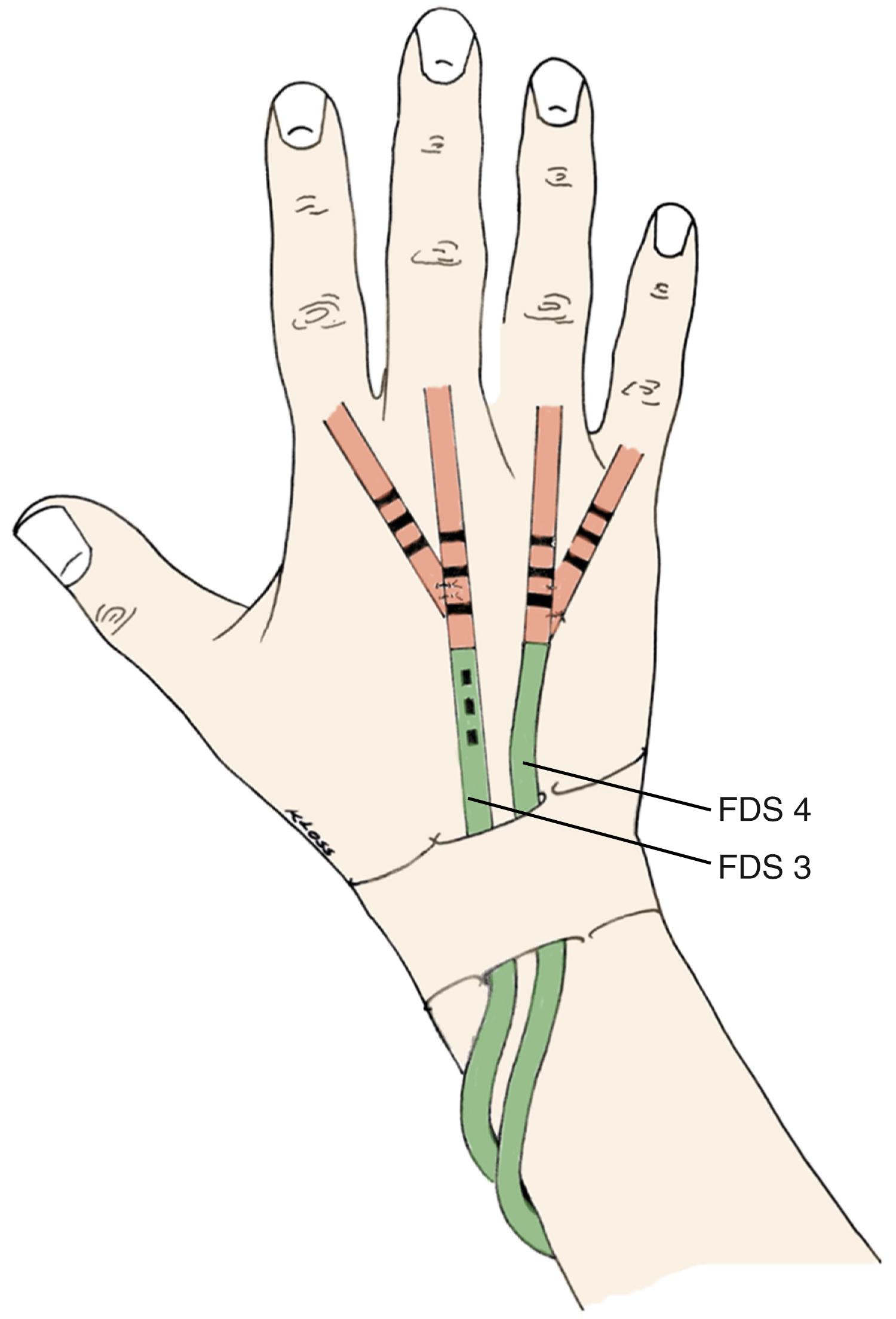
The transfer is performed through three incisions. A small transverse incision is made in the distal palmar crease, and the tendon is divided after applying proximal traction. This provides enough length to reach the MCP joints. A second incision is made on the volar aspect of the forearm and should be positioned ulnar to the midline, so that the final transfer passes deep to the skin incision and thus minimizes tendon adherence. The third incision is made on the dorsal aspect of the hand, where the transfer is attached to the extensor mechanism of the ring and little fingers. Care must be taken to route the transferred tendon deep into the superficial radial nerve; symptomatic compression of the nerve can occur as a result of the tendon passing over the nerve.
Rupture of the extensor pollicis longus (EPL) tendon is a frequent event in RA. However, the resultant functional loss can differ greatly and essentially depends on the functionality of the intact EPB as well as the status of the joints of the first ray. EPL rupture is often characterized by active functional loss at the IP joint, but more frequently, there is a reduction in extension strength and extension range at the MCP joint. Normally the EPB tendon is too weak to compensate for full extension ability of the MCP joint. In addition, the intrinsic muscles also contribute to the extension of the IP joint to neutral posture, which may obviate the need for EPL reconstruction.
Restoration of EPL function is recommended if there is severe functional disability. End-to-end suturing is generally no longer possible, even immediately after rupture, because the frayed tendon is already shortened. This applies to all spontaneous rheumatic ruptures. Tendon grafts that have been woven through tissue altered by inflammatory processes tend to adhere and therefore are not recommended for the repair of ruptured extensor tendons in the rheumatoid hand. Nevertheless, as long as a contractile muscle is still present, reconstruction of the EPL by tendon grafting can lead to good clinical outcome. The powerful FPL and its action can counteract the EPL tendon adhesion in the long term.
The treatment of choice to restore EPL function is generally tendon transfer. The most frequently used donors are the muscle-tendon unit of the EIP and, to a lesser extent, the tendons of the ECRL or EDQ. Millender and colleagues advocate EIP transfer because this tendon can be released at the MCP joint level without any apparent functional loss for this joint. Surprisingly, the patient does not lose the ability to extend the index finger independently from the other long fingers. Strength and amplitude of the EIP are almost identical to those of the EPL.
If at least two ulnar extensor tendons are ruptured in addition to an EPL rupture, then the EIP cannot be used because it is required for reconstruction of the ulnar tendons. In these cases, the reconstruction technique of choice uses a palmaris longus graft. If the palmaris longus is missing, a strip of the ECRL, plantaris, or extensor tendon of the fourth toe may serve as graft material. However, tendon grafting is only appropriate for relatively fresh ruptures, which offers good contractility of the proximal musculotendinous unit.
The postoperative care after EIP to EPL transfer follows the standard protocol of this intervention with splinting of the thumb. When the swelling is controlled, tenodesis exercises using the wrist are started. After 3 weeks, active flexion/extension exercises are undertaken, and the splint is gradually removed after 4 weeks.
Until swelling and pain is controlled, a volar splint with the wrist in 30 to 40 degrees extension and the MCP joints in slight (10 to 20 degrees) flexion is recommended. Gentle active motion of the PIP and DIP joints are then started while the wrist and MCP joints remain immobilized for 3 to 4 weeks. Because impairment of finger flexion is functionally more important than a slight extension lag, it is important to encourage full finger flexion during the rehabilitation phase. Although dynamic splints can theoretically prevent adhesions, they are not used on a routine basis because it is cumbersome to wear and difficult to construct. Nevertheless, the application of a dynamic splint might be considered to prevent tendon adhesions and protect the double-sided weave sutures in cases with multiple bridge grafts.
Functional deficit with loss of finger extension
Impending rupture of extensor tendons at the wrist
Usually the rupture starts at the ulnar side, first with the little finger in which its function may be compensated by the juncturae attachment to the ring finger.
Ruptures occur through tenosynovitis and attritional rupture at the level of the eroded distal ulna.
Additional treatment of the DRUJ is often needed.
Planning is important! Ultrasound and MRI help determine the damage. Plan for various tendon transfer options because the number and level of the rupture tendons are unpredictable.
Standard longitudinal incision to the wrist, which can be used for later surgery as well.
Synovectomy of the radiocarpal and the DRUJ is often needed. If the ulna head is intact, look for ulnar head irregularities and capsule perforations that may cause the tendon rupture.
Identification of the ruptured extensor tendons with visualization of all extensor tendon compartments by extending the incision to assess the tendons all the way to the muscles.
Options for the treatment of the DRUJ: ulnar head resection, Sauvé-Kapandjj, and occasionally ulnar head prosthesis.
Direct tendon repair is rarely possible. Evaluation for tendon bridge grafting versus tendon transfer.
If possible, one tendon, one function. Often the proximally ruptured tendons can serve as tendon graft to reserve one more normal tendon to power extension of several fingers.
The standard teaching is to make the tendon repair a bit tighter because it will often stretch out.
In fused wrists, the reconstructed finger should have greater tension but should be able to be passively flexed to make a fist.
Secure the tendon reconstruction with a strong, long suture line.
Retinaculum reconstruction is important but needed to avoid friction with the reconstructed tendon.
Active motion protocol for the PIP and DIP joint while the MCP and wrist is immobilized for 3 weeks. In mobile wrists, tenodesis can be used to move the transfers.
Flexion is functionally more important than extension and the individualized protocol should take that in consideration.
Although flexor tendon ruptures are less common than their extensor tendon counterparts, they share a similar etiology. Synovitis over the flexor tendon sheath can cause attritional rupture of the FPL and index finger profundus tendons lying close to the scaphoid. Volar subluxation of the scaphoid is common in rheumatoid patients with carpal supination of the wrist. The arthritic and eroded distal scaphoid may penetrate the volar wrist capsule and abrade the flexor tendon of the thumb and the profundus tendon of the index finger, which lie close together deep within the forearm.
Various tendon transfer rupture patterns can occur in the carpal tunnel and distal forearm when there is an extensive amount of synovitis. In these situations, aggressive synovectomy is necessary not only to remove the invasive synovitis but also to alleviate the compression over the median nerve. The synovectomy can be performed through an extensile incision from the carpal tunnel to the forearm. There is a myriad of options for tendon transfers, including a brachioradialis-to-FPL tendon transfer for thumb flexion. A creative method is to use the FDS tendons from the middle finger to repair the ruptured thumb or index finger tendons. It may be difficult to identify the exact tendons that are ruptured because the synovitis binds the tendons together, which facilitates finger motion. However, the existence of tendon ruptures becomes apparent once the synovitis is removed.
As already stated, the FPL is most vulnerable to fraying or attrition rupture as it crosses the scaphotrapezial joint. Rheumatoid joint disease and local synovitis can create sharp spikes of bone against which the tendon abrades and finally ruptures during use; this was referred to as the Mannerfelt lesion. The deep flexor to the index, and less frequently to the middle finger, is also at risk at this specific anatomic site.
Rupture of the FPL leads to serious functional impairment of the thumb and typically requires treatment. It is important to distinguish two different goals in treatment:
Restoration of thumb function
Prevention of further tendon ruptures, especially of the flexor digitorum profundus to the index finger
In addition to any reconstruction of the missing tendon, exploration of the carpal canal is mandatory to detect impending rupture of other flexor tendons caused by the presence of any bony erosion, which need to be debrided.
In particular, a single-stage reconstruction of the thumb, using a tendon graft usually taken from either the palmaris longus or FCR tendon, is most successful. As for any other tendon reconstruction procedure, it must be ensured that the musculotendinous unit is still functional and adequate tendon excursion is present.
In the case of a longstanding rupture and uncertain muscle function, a tendon transfer might be more advisable. Typically, the superficial flexor tendon of the ring finger is used for the reconstruction of thumb flexion. This is best performed by an end-to-end suture in the technique as described for extensor tendon reconstruction. For acute ruptures of the FPL tendon, lengthening at the musculotendinous junction and direct end-to-end suturing after adequate debridement may also be considered.
Alternately, the thumb IP joint may be stabilized by fusion. In these cases, it is mandatory to have a functioning MCP joint. In addition, acceptable muscle strength of the intrinsic thumb muscle must be present in order to provide satisfactory pinch force.
The volar aspect of the palm and wrist is exposed through a curved incision along the thenar crease and extended proximally in a zigzag manner. The bone spicule on the scaphoid that protrudes into the radial side of the carpal canal is removed, and the exposed bone is covered by mobilizing adjacent wrist capsular tissue. Attention is then directed toward restoration of tendon function. Surgical choices, as mentioned, include the use of a bridge graft, a standard tendon graft, or a tendon transfer. If both tendon ends can be identified at the wrist level, we prefer to insert a short bridge graft. The palmaris longus is suitable for this, but if not present, a slip of the FCR or one of the multiple slips of the APL can be used. If suturing at the level of the rupture is difficult because of its location in the carpal tunnel, incisions can be made at the level of the MCP joint and distal forearm, whereby the graft can be passed across the tunnel and sutured both distal and proximal to the stumps. If the distal tendon stump cannot be brought into the wrist incision, we either use a full-length tendon graft or transfer a superficial flexor tendon. The preference is to use the superficial flexor of the long finger as the motor because it is longer and avoids compromising the grip function of the ring and little fingers.
The superficial flexor is detached in the distal part of the palm and sutured to the volar aspect of the distal thumb phalanx with a suture passed through the distal phalanx and tied over a button on the dorsal aspect of the nail plate. Reattaching to bone is done if the distal tendon stump is too short, less than 1 cm for primary tendon repair. If more than 1 cm of distal tendon is present, then tendon-to-tendon repair is preferred. A soft rubber catheter or a tendon passer is used to bring the tendon through the sheath and pulley mechanism. The stump of the FPL is elevated, and the underlying cortex is roughened before final attachment of the graft or transfer. Carpal tunnel release and flexor tenosynovectomy are usually performed at the same time.
The thumb and wrist are immobilized in moderate flexion for 3 weeks, after which time active motion is started. If the carpal tunnel is opened to perform tendon reconstruction, the wrist is positioned in neutral for 3 weeks to prevent flexor tendon bowstringing.
Rupture of one or more of the deep flexor tendons is not uncommon but difficult to treat and can often lead to significant loss of hand function. Therefore early diagnosis is also mandatory to prevent such a devastating situation.
The treatment should match the degree of functional loss. If a patient with these ruptures can maintain superficial flexor function (in terms of both range of motion and strength), functional loss is minimal. In addition, if the distal tendon stump becomes adherent, the patient may lose active flexion but may maintain sufficient stability of the DIP joint to preclude the need for surgical stabilization.
The most important factor determining the type of treatment is the level of tendon rupture. Flexor tendon ruptures can occur within the finger, at the palm, or at the wrist. The palm is the easiest level at which function can be restored. Ruptures at the palm may be less obvious if the ruptured tendon adheres to adjacent flexors. This obscures the diagnosis inasmuch as DIP joint flexion is possible with the finger extended and the flexor mass pulls on the distal tendon end through scar tissue. However, this is not so when the finger is flexed actively or passively at the PIP joint. This situation can be mistaken for a flexor tendon nodule that blocks active excursion of the profundus tendon. Clues to the proper diagnosis include the lack of a palpable nodule and an alteration in resting finger posture, with the finger assuming a more extended position than the adjacent fingers. Ultrasound is a powerful tool to identify the varying patterns of tendon lesions and pathologies.
Flexor tendon ruptures at the palm and wrist levels are best treated by suturing the distal tendon ends to the adjacent intact tendon, although small bridge grafts can be used at the wrist level. Suturing to adjacent tendons cannot be done if the rupture occurs within the fibroosseous canal. In this case surgery is performed only to remove diseased synovium from the intact superficial flexor, which is now vital to finger function. Caution should be used when considering staged flexor tendon reconstruction of the FDP through an intact FDS. The results of this technique have been inadequate. If the DIP joint hyperextends, it is better to stabilize the DIP joint by suturing the distal FDP tendon stump to the proximal DIP volar plate with slight DIP fusion posture rather than consider a flexor tendon graft through an intact FDS tendon.
Loss of FDS function alone does not result in obvious functional loss. The diagnosis of a FDS rupture can only be made by careful clinical examination and sonography with an occasional MRI exam as required. The treatment should not jeopardize existing tendon function; however, suturing to adjacent tendons within the palm or the wrist is feasible. A tenosynovectomy should be performed to protect the FDP tendons.
Restoration of active finger flexion is a goal that is not always possible to achieve. For this reason, it is far better to be aware of early nodular tenosynovitis and to perform prophylactic tenosynovectomy before tendon rupture occurs. If ruptures have occurred at the wrist, function can be restored by suturing to adjacent tendons or by applying a bridge graft to the FDP tendon with the suture lines placed proximal and distal to the carpal tunnel area. It is not necessary to reconstruct FDS tendon ruptures at the wrist. Therefore an intact portion of it can be used for bridge grafts to reconstruct ruptured FDP tendons. If the rupture is located at the palm and the distal tendon stump is long enough, adjacent suturing to an FDP tendon offers the best option. If not, transfer of an FDS to the distal profundus stump can be done.
Within the fibroosseous canal, the same issue is encountered with tendon laceration at this level, although the RA situation is usually worse. The disease is not localized, and the dissection needed for exposure leaves a very poor surface for tendon grafting. In addition, the adjacent joints may have restricted or painful motion (or both). In our experience, free flexor tendon grafts have not produced favorable results for patients with RA. On occasion when no other alternative is available, a staged-flexor tendon reconstruction using a silicone tendon rod can be performed, particularly for younger patients who have minimal joint involvement. The technique is essentially the same as described for posttraumatic flexor tendon reconstruction.
Finally, the wisest choice is to fuse both PIP and DIP joints in a functional position for some patients with both flexor tendons ruptured within the finger, who are of advanced age, have poor IP joint status, or have a generally poor health status. In this way, satisfactory function can be restored and pain diminished. Suturing the proximal flexor tendon stumps to the base of the proximal phalanx in the tenodesis fashion may augment MCP flexor strength, if there is free excursion of the flexor tendon proximal to the rupture. Naturally, this should be considered as a last resort only to handle this challenging situation in selected patients.
Tendon rupture owing to synovitis and/or attrition
The FPL and the index finger profundus tendons often rupture by abrading over the eroded flexed distal scaphoid.
The sudden loss of flexion of the thumb and DIP joint of the index finger makes this diagnosis clear.
A variety of tendon transfer options are available, but the most suitable ones are brachioradialis to FPL and end-to-side transfer of the index profundus tendon to the long finger profundus tendon.
It is important that the source of the rupture is determined and treated. Flexor synovitis must be excised radically and the distal pole of the scaphoid debrided or removed to prevent future rupture. The rent over the volar capsule where the scaphoid has protruded should be repaired primarily or a rotational flap can be used to close it.
Free flexor tendon grafts in general do not produce good results in RA patients.
The tendon transfer can be repaired under sedation or wide awake technique so that the tension can be set precisely as the patient moves the tendon transfer intraoperatively.
The FDS of the long finger can be transferred to the FPL, which will provide this transfer much greater excursion, as the FDS is a “smart” tendon with about 70 mm of excursion.
If independent movement of the index tip is desired, the FDS of the index finger can be transferred to index profundus tendon, but the tension must be set precisely to avoid a lax tendon system.
If the tendon rupture was detected early, less than 3 months, before myostatic contracture causes loss of excursion of the proximal muscle, tendon grafting can be used, in particular when the palmaris longus tendon is available.
Staged flexor tendon reconstruction is only indicated in younger patients with minimal joint involvement. Its technique follows the principles of posttraumatic situations with the use of the silicone rod.
In cases of rupture of both flexor tendons and bad joint conditions (often happen concurrently), fusion of the PIP and DIP joint may be a good functional option. The fusion position should be determined individually and depends on the MCP joint function. Usually the DIP joint is slightly flexed and the PIP joint determines the general finger position.
RA patients have healing problems because of their immunosuppression; early active motion may risk tendon rupture. It is helpful to have an experienced RA therapist coordinates tenodesis exercises and passive flexion of the digits to achieve some tendon excursion before initiating action motion.
Active motion of the tendon transfer is not commenced until 6 weeks after surgery because tendon healing in RA patients will be slower.
The ulnar side of the wrist is another target in the treatment of RA and is often the primary site of disease activity. Resection of the ulnar head is a classic intervention, which was initially used as early as 1912 for the treatment of deformities after Colles’ fractures. , For decades, this procedure was standard in the treatment of DRUJ involvement in RA. It is almost always combined with dorsal tenosynovectomy or in advanced cases, with extensor tendon reconstruction.
There are three main issues to consider with ulna head resection in RA patients:
Ulna stump instability
Acceleration of wrist instability, especially ulnar translation
Poor esthetic aspect of the wrist
The first issue, ulna stump instability, is caused by loss of stable forearm system between ulna and radius that loses its support upon resection of the ulnar head. Although it is always more or less apparent clinically, this condition is not often perceived by the patient. Grinding of the ulna against the radius is initially detectable by both the patient and surgeon but may disappear over time due to the adaptive reaction of the radius. This is indicated by the scalloping sign over the sigmoid notch as seen on long-term follow-up radiographs. The radius presents with erosions with subsequent sclerosis opposite the ulna stump.
For patients, particularly those with higher demands, the instability may be functionally relevant and should be prevented. Although many ulna stump stabilization techniques have been described, no single procedure has proven superior over another. The most popular uses the distally based ulnar half ECU tenodesis (see operative technique), which stabilizes not only the ulna stump but also the wrist and, at least partially, corrects the deformation. , Alternately, a strip of the FCU tendon may be used, although the harvesting procedure from the dorsal aspect is technically challenging. In this instance care should be taken not to damage the ulnar nerve, which is positioned more superficially than the tendon. Even with a combined proximally based ECU slip and distally based slip of the FCU, good results have been reported, but mainly for posttraumatic cases. Ruby and colleagues transferred the origin of the pronator quadratus to the dorsal aspect of the ulna and placed the muscle belly between the radius and ulna to stabilize the distal ulna after resection of its head. The long-term results were satisfactory, but rheumatoid patients were not included in the study cohort. This technique has also been described by Bain and colleagues in combination with hemiresection arthroplasty.
For the second issue, Rana and Taylor reported about 10% more ulnar translocation of the wrist after distal ulna resection. These events did not affect clinical outcome at follow-up. Van Gemert presented similar observations but highlighted the fact that the disease itself may have been more likely to cause this effect. Similar results were reported by Melone and Taras with about 8% advanced, disabling ulnar wrist dislocation. Due to the lack of more recent studies, the evidence on this subject is rather limited. However, excessive radiocarpal instability is a relative contraindication for distal ulna resection, and should always be combined with wrist stabilization methods, typically a radio(scapho)lunate fusion.
For the third issue, the appearance of the wrist without the ulnar head is somewhat unnatural. With the increased demands of some RA patients with stable disease activity, this aspect has to be taken into account when choosing a technique for DRUJ treatment in RA patients. An intervention such as the Sauvé-Kapandji procedure enables preservation of the ulna head with resection of a more proximal ulna segment.
Younger patients with higher demands are a relative contraindication for distal ulna resection; Bieber et al. reported unfavorable results in patients younger than 45 years.
The surgical principles of distal ulna excision are important and include the following aspects of (1) limited resection of the distal ulna end (2 cm or less) to minimize instability of the remaining ulna, (2) DRUJ synovectomy, (3) correction of carpal supination by suturing the remnant of the TFCC to the dorsoulnar corner of the radius, and (4) reconstruction of the dorsal capsule and extensor retinaculum with volar-to-dorsal relocation of the ECU if it is subluxated.
The wrist joint is approached through the dorsal longitudinal or “S” incision. The extensor retinaculum is opened. It is usually thin or adherent (or both) over the distal ulna capsule, which makes separation of these two layers difficult. Identification of the volar subluxated ECU may also be difficult. The tendon usually can be palpated on the ulnar aspect of the wrist. Frequently, tenosynovium is noted bulging in the region of the sixth dorsal compartment. Occasionally, the entire sixth compartment sheath is destroyed, and the tendon is frayed or ruptured. If the ECU has subluxated volarward, it is released and replaced dorsal to the axis of wrist flexion. It can be held in place with a sling of tissue fashioned from the extensor retinaculum.
A longitudinal capsular incision is made over the distal ulna. The capsule and triangular fibrocartilage are reflected from the ulna and preserved. The periosteum of the ulna is elevated, and small bone retractors are placed around the distal ulna, which can be sectioned either with a bone cutter, an osteotome, or more precisely with a power saw. A towel clip is used to apply traction to the bone fragment when the soft tissue attachments are detached. Approximately 2 cm of bone is resected. If excessive bone is removed, distal ulna stability may pose a problem. The dorsal edge of the proximal ulna should be made bevel and smooth to minimize the risk of postoperative attrition ruptures of the extensor tendons.
After the bone is removed, complete synovectomy of the DRUJ is performed. Although the triangular fibrocartilage is often destroyed, it should be protected during synovectomy when present. Reconstruction of the soft tissue support for both the DRUJ and radiocarpal joint is important to correct carpal supination and stabilize the distal ulna. If the TFCC and radioulnar ligamentous complex are present, they are sutured tightly to the dorsal and ulnar aspect of the radius.
Various methods have been used to stabilize the distal ulna after resection of the ulna head as already outlined. Linscheid and Dobyns used a different method : A distally based strip of the ECU tendon is detached, woven through the ulnar collateral ligament and any remnants of the triangular fibrocartilage, and sutured to the radius. The dorsal radioulnar capsule is closed tightly with tissue imbrication, when required. This is facilitated by supinating the wrist to relocate the DRUJ. Thereafter, the extensor retinaculum is relocated deep within the tendons, and the position of the ECU tendon is corrected if necessary.
Another method applies a distally based slip of the ECU tendon. The tendon slip is passed through the distal end of the ulna through a hole made in the dorsal cortex of the ulna and then sutured back onto itself.
An alternative is to use a Freer elevator to compress the ulna volarward and suture either the capsular tissue or ECU tendon tightly to seat the ulna stump in this volar position. This is a simple maneuver that we use most often, which serves the purpose of stabilizing the ulna stump ( Fig. 55.15 ).
Subluxation of the distal ulna causing DRUJ pain and/or extensor tendon rupture
Be sure the wrist is not subluxated over the radius, which can be accentuated if the supporting distal ulna is resected. Fusion of the DRUJ is a better option when there is impending wrist subluxation
Distal ulna excision should be cut obliquely to avoid impingement of the ulna on the radius.
The dorsal capsule over the distal ulna must be imbricated tightly to prevent recurrent dorsal subluxation.
A slip of the ECU can be used to stabilize the distal ulna. The pronator quadratus can be detached ulnarly and swung over the distal ulna for additional stability.
Always check the condition of the extensor tendons because undetected tendon fraying or rupture may be present.
For most patients who are compliant, volar splinting may suffice if the distal ulna can be reduced easily and is stabilized just with the dorsal capsular imbrication.
In cases of severe instability of the ulna stump, the forearm should be splinted in supination for 4 weeks to permit the reconstruction to stabilize.
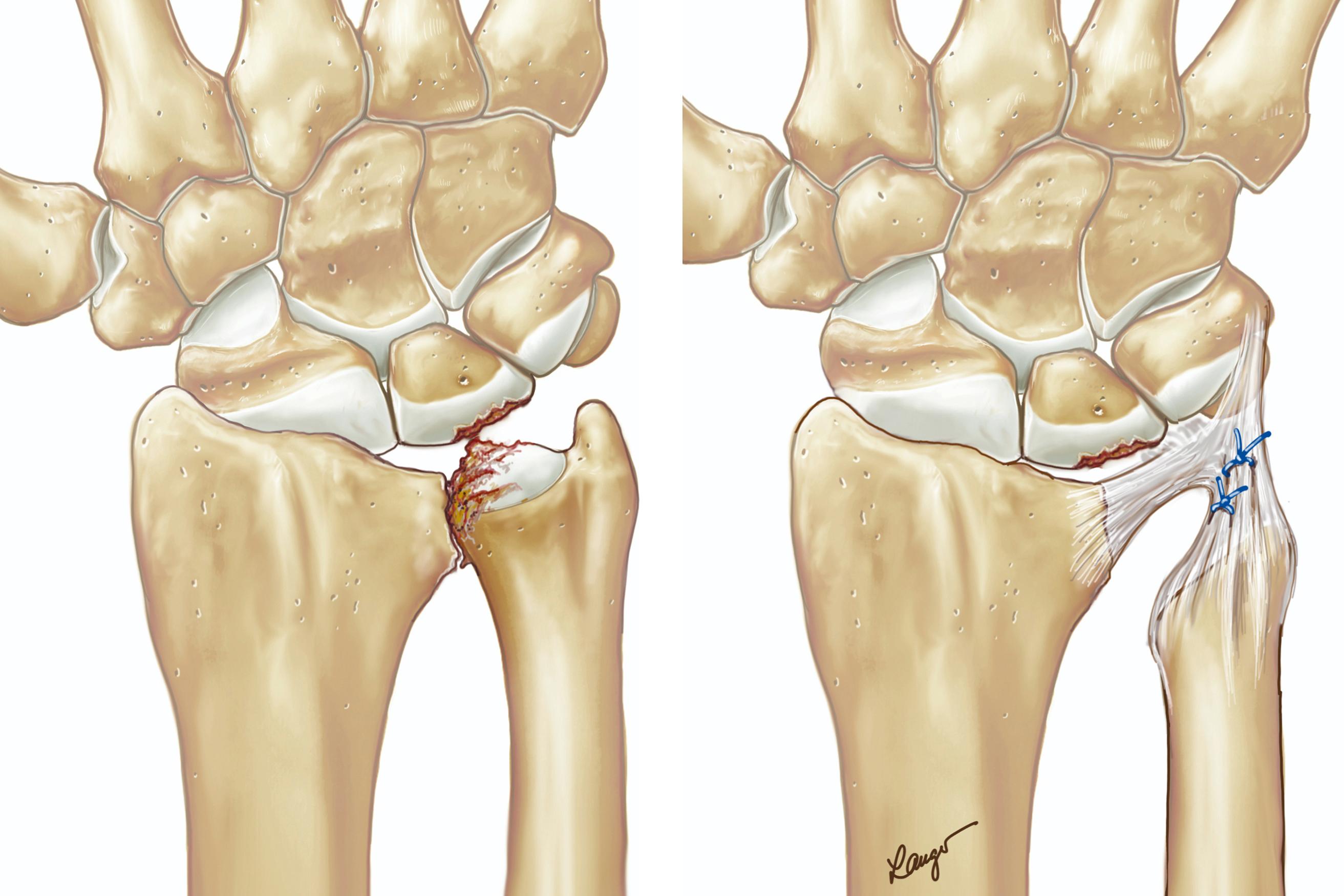
A bulky hand dressing is applied with the wrist and fingers splinted in their neutral position. There is no need to splint the forearm in supination because the patient typically will not move the wrist at all because of pain, unless directed. Finger motion is immediately started. There is no need to splint the fingers, whereas the wrist is splinted in its neutral position for 4 weeks before initiating active motion.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here