Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Since being approved by the U.S. Food and Drug Administration in 2003, reverse shoulder arthroplasty (RSA) has become the standard of treatment for elderly patients with irreparable rotator cuff tears and arthritis. By 2020, it is projected that over 80,000 RSA procedures will be performed every year. A firm grasp on both patient selection and surgical technique will help guide surgeons as they treat this growing patient population. This chapter guides the surgeon in treating patients with rotator cuff tears not amenable to repair.
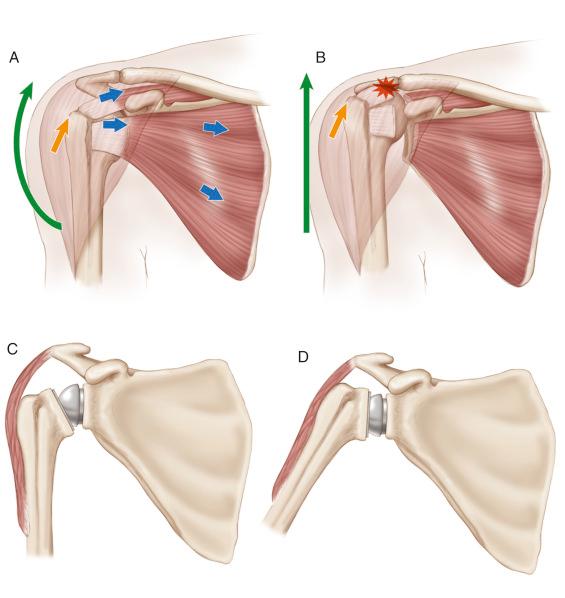
A reverse shoulder prosthesis is designed to work in the absence of a functional rotator cuff by creating a stable fulcrum about which the deltoid can elevate the shoulder in the absence of the humeral head’s centering effect on the rotator cuff. This loss of centering effect can be seen as a loss of vertical or horizontal plane stability leading clinically to loss of elevation, rotation, or a combination thereof. A cuff-deficient shoulder leads to decreased function, both by the loss of muscular forces from the missing cuff muscles and by the loss of a stable fulcrum about which the remaining muscles can rotate the shoulder. A reverse prosthesis stabilizes the shoulder joint by converting the shear forces of the deltoid and remaining cuff musculature to compressive forces that allow for improved shoulder function (see Fig. 39.1 ).
Chronic rotator cuff tears typically present with a gradual loss of function and increasing pain during attempted shoulder movement. A traumatic inciting event is rarely identified.
Acute-on-chronic tears may present with a sudden increase in pain following a specific traumatic event. Patients often report an extended period of nondebilitating shoulder pain prior to the accident.
Acute tears present with immediate onset of pain with no prior shoulder problems or dysfunction.
Patients should be asked about any cervical spine pain or discomfort.
Burning pain in the shoulder or pain radiating past the elbow warrants a detailed cervical spine examination.
Ask the patient about any functional deficits related to their shoulder pain/dysfunction. A painful functional shoulder will be treated differently from a nonfunctional shoulder.
The surgeon should focus on active and passive range of motion in forward flexion, abduction, external rotation (at side and in 90 degrees of abduction), and internal rotation. These motions should be assessed in both the standing and supine positions.
Evaluate for loss of external rotation manifested by Hornblower’s or external rotation lag sign.
Combined loss of active elevation and external rotation is an indication to perform a latissimus dorsi transfer in addition to RSA.
Test subscapularis strength/integrity via Napoleon’s/belly press test.
Note the appearance of shoulder shrug with attempted abduction, because this is a sign of pseudo paralysis (see Fig. 39.2 ).

Cervical flexion, extension, and rotation should be performed in a seated position.
Pain with any of these movements warrants further studies of the cervical spine.
Pseudoparalysis of the shoulder has no clear definition, but it can be seen as a combination of physical exam findings:
Elevation less than 90 degrees
Appearance of shoulder shrug with attempted abduction
Pain
Upper cervical radiculopathy (particularly involving C4 or C5) can mimic pseudo paralysis.
Radiculopathy may be distinguished by pain that extends beyond the elbow.
Patients may have pain with flexion/extension of the spine.
Any upper extremity neurologic deficit leading to deltoid dysfunction is an independent risk factor for poor outcome after RSA for massive cuff tear.
Previous rotator cuff surgery can result in deltoid dysfunction.
An electromyogram should be ordered when questions exist about axillary nerve activity.
X-ray
Humeral head frequently has superior migration in relation to the glenoid (see Fig. 39.3 ).

Loss of acromiohumeral distance is seen with posterosuperior cuff tears.
Anterior subluxation may be noted on the axillary view in cases of anterior cuff tear.
Evaluate for os acromiale or acromial fracture.
Computed tomographic scan
Allows for better understanding of bony anatomy.
Note the version of the glenoid, translation of the humeral head (anterior, centered, posterior), and presence of osteophytes or loose bodies.
Superior migration of humeral head is noted in association with posterosuperior cuff tears, whereas anterior subluxation is seen with anterior cuff tears.
Look for the presence of os acromiale or acromial fractures.
Evaluate for the presence of fatty atrophy in the rotator cuff musculature. This is graded according to the Goutallier classification.
Magnetic resonance imaging (MRI)
Improves understanding of rotator cuff integrity.
Also allows for grading of degree of fatty infiltration.
Can demonstrate teres minor atrophy, which may be an indication to add a latissimus dorsi transfer at the time of RSA (see Fig. 39.4 ).
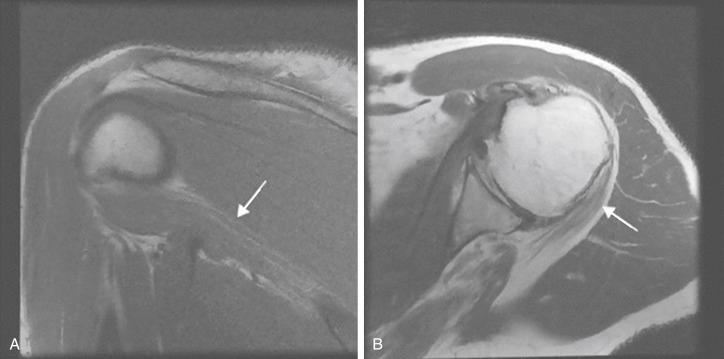
Isolated teres minor atrophy is seen on 3.3%–5.5% of shoulder MRI scans. This can be a unique pathological process or may be related to quadrilateral space syndrome.
Nonoperative treatment:
First-line treatment in nearly all patients
Consider in patients with preserved function and those unable to safely undergo surgical intervention.
Anterior deltoid reeducation physiotherapy has shown benefit in some studies.
Operative treatment:
Rotator cuff repair
Results are negatively affected by older physiologic age, anterosuperior escape, fatty infiltration of rotator cuff, failed previous cuff surgery, and smoking.
Arthroscopic superior capsular reconstruction
May be an option for younger patients with irreparable cuff tears
RSA
Produces consistent relief of pain and improvement in function in properly selected patients
Requires a functional deltoid muscle for optimal outcomes
RSA with modified L’Episcopo transfer of the latissimus dorsi and teres major is indicated in cases of combined loss of active elevation and external rotation.
Reverse prosthesis will rebalance the shoulder in the vertical plane, but the tendon transfer is necessary to rebalance the shoulder in the horizontal plane and restore active external rotation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here