Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Access video and video lecture content for this chapter online at Elsevier eBooks+ ![]()
![]()
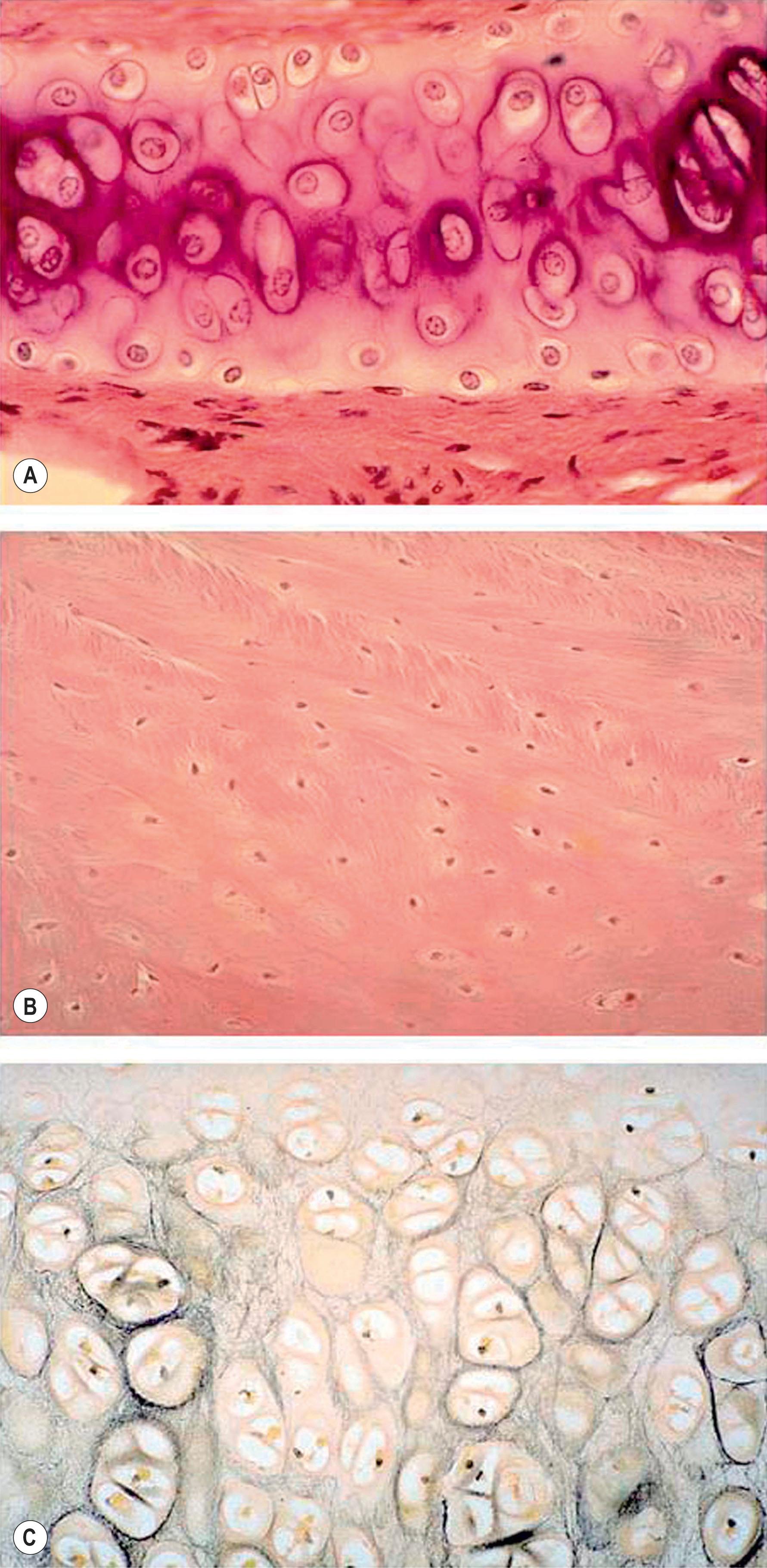
Cartilage is one kind of connective tissue, which is mainly composed of chondrocytes and their produced extracellular matrices (ECM) of type II collagen fibers, proteoglycans, and elastic fibers. According to the composition, cartilage can be classified into three types. (1) Hyaline cartilage, which is the most common type of cartilage and can be found in costal, articular, tracheal and nasal cartilages, etc. Except articular cartilage, the free surface of most hyaline cartilages is covered with perichondrium. In addition to collagen II, hyaline cartilage is rich in glycosaminoglycans and is thus characterized by its stiffness that allows for sustaining compressional loading. (2) Fibrocartilage is composed of bundles of thick collagen fibers along with intervenient unicellular islands of cartilage arranged in small chains. Because of this unique structure, fibrocartilage can provide high tensile strength and supporting function and is thus present in the areas most subject to frequent stress such as meniscus, intervertebral discs, symphyseal joints, and the joint portion of bone and tendons/ligaments. Different from other cartilage, fibrocartilage also contains type I collagen. In addition, it has a moderate amount of proteoglycans but low content of glycosaminoglycans. (3) Elastic cartilage is characterized by its extremely high elasticity because of the presence of abundant amounts of elastic fibers. It is histologically similar to hyaline cartilage but contains many elastic fibers which form an elastic fiber network along with collagen fibers. This unique feature provides elastic cartilage great flexibility so that it can withstand repeated bending. Elastic cartilage is mainly found in outer ear structures, and also found in larynx and epiglottis. It is also surrounded with perichondrium. Fig. 19.1 shows the histology of the three types of cartilage.
The perichondrium is a layer of dense irregular connective tissue that consists of two separate layers, an outer fibrous layer and an inner chondrogenic layer. Collagen fibers and fibroblasts constitute the fibrous layer. In contrast, the chondrogenic layer remains partially undifferentiated and is likely to contain mesenchymal stem cells and chondrogenic progenitor cells, which can play a role in cartilage repair and regeneration.
Cartilage is a unique tissue with low metabolic rate due to the sparsity of its cell population and its avascular structure. The glycolytic activity and oxygen consumption of cartilage approaches anaerobic condition and the tissue is nourished by tissue fluid diffusion. Because of this unique feature, cartilage graft survives relatively easily when being implanted. In terms of cartilage grafting, Sushruta Samhita in India around 600 BCE is probably the first person to perform cartilage grafting in the form of a composite graft. Cartilage graft is widely used for repairing nasal or auricular defects as well as for reconstructing other tissues either as a pure cartilage graft or as a composite graft. According to surgical procedures, cartilage can be transferred either as a free graft or as a microvascular composite graft. Generally, autologous cartilage graft will not have metaplastic changes even being transferred to a different location. In addition, grafting of free perichondrial tissue is also a common procedure for cartilage reconstruction because it has long since been observed that perichondrium possesses the ability to regenerate cartilage.
Although cartilage is considered as “immunologically privileged”, and allogeneic cartilage may serve as a potential graft, autologous cartilage grafting remains the most applicable cartilage graft. Generally, the common donor sites for harvesting autologous cartilage grafts include auricular cartilage, nasal cartilage, and rib cartilage.
As an elastic cartilage, auricular cartilage is an ideal graft for transplantation and perhaps is the most versatile of all cartilage grafts because it can be easily fashioned and contoured into different shapes for various uses. Auricular cartilage can be harvested easily under local anesthesia and a significant portion of the concha can be removed without causing donor site deformity.
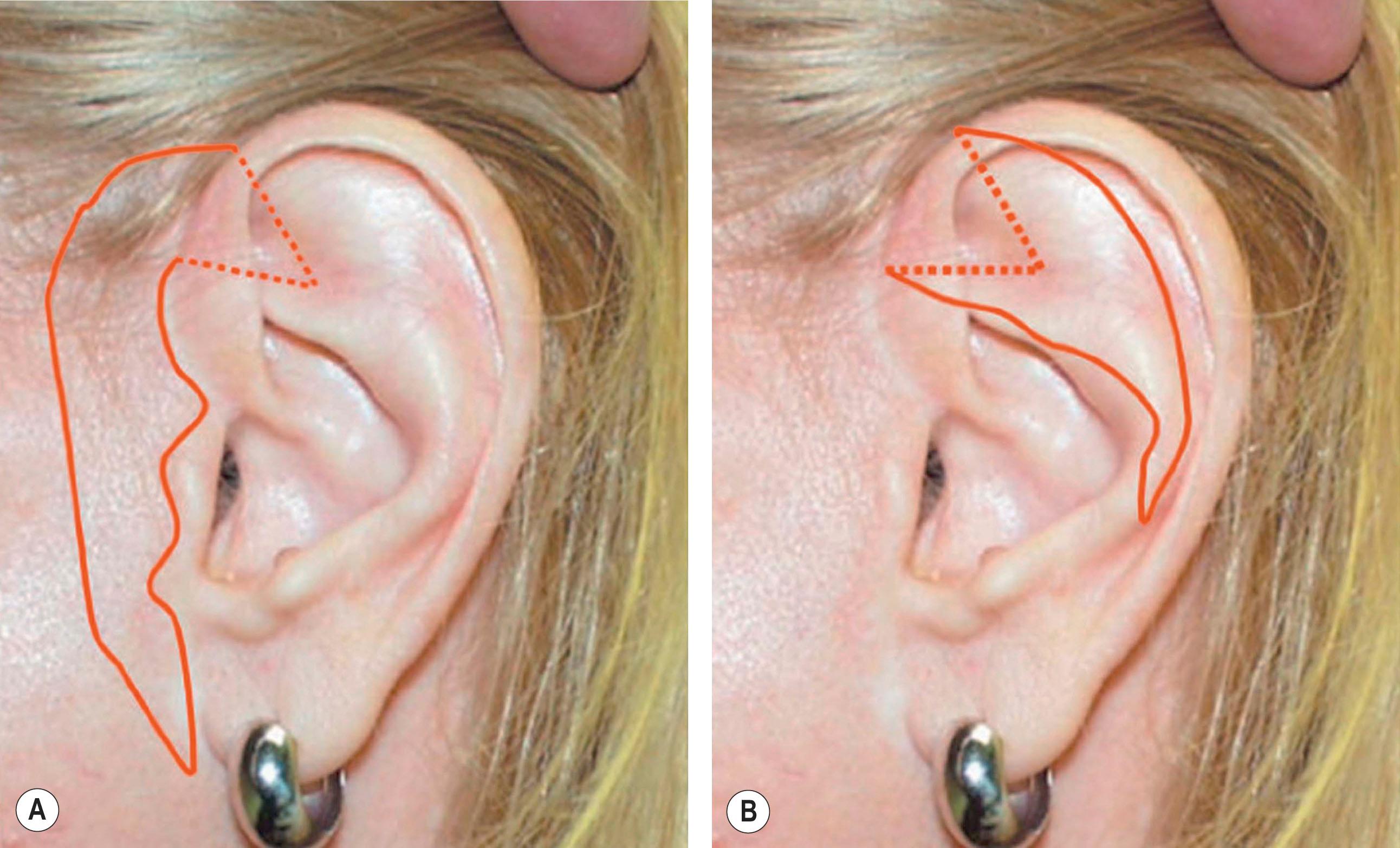
However, in practice, harvesting of entire conchal cartilage is likely to cause collapsed conchal bowl, cymba concha, and a horizontally short ear. To overcome the problem, Han et al . have proposed the surgical procedure that involves (1) using a postauricular incision to minimize visible scars, (2) harvesting the entire cymba concha and cavum concha separately, with at least 5 mm of the helical crus, leaving a lateral extension as a strut between them, as well as a 2 mm outer rim along the conchal wall, and (3) by using a tie-over bolster dressing that can serve as a mould for the conchal bowl. Fig. 19.2 presents the technique to avoid contour irregularity or deformity after harvesting maximal amount of conchal cartilage graft.
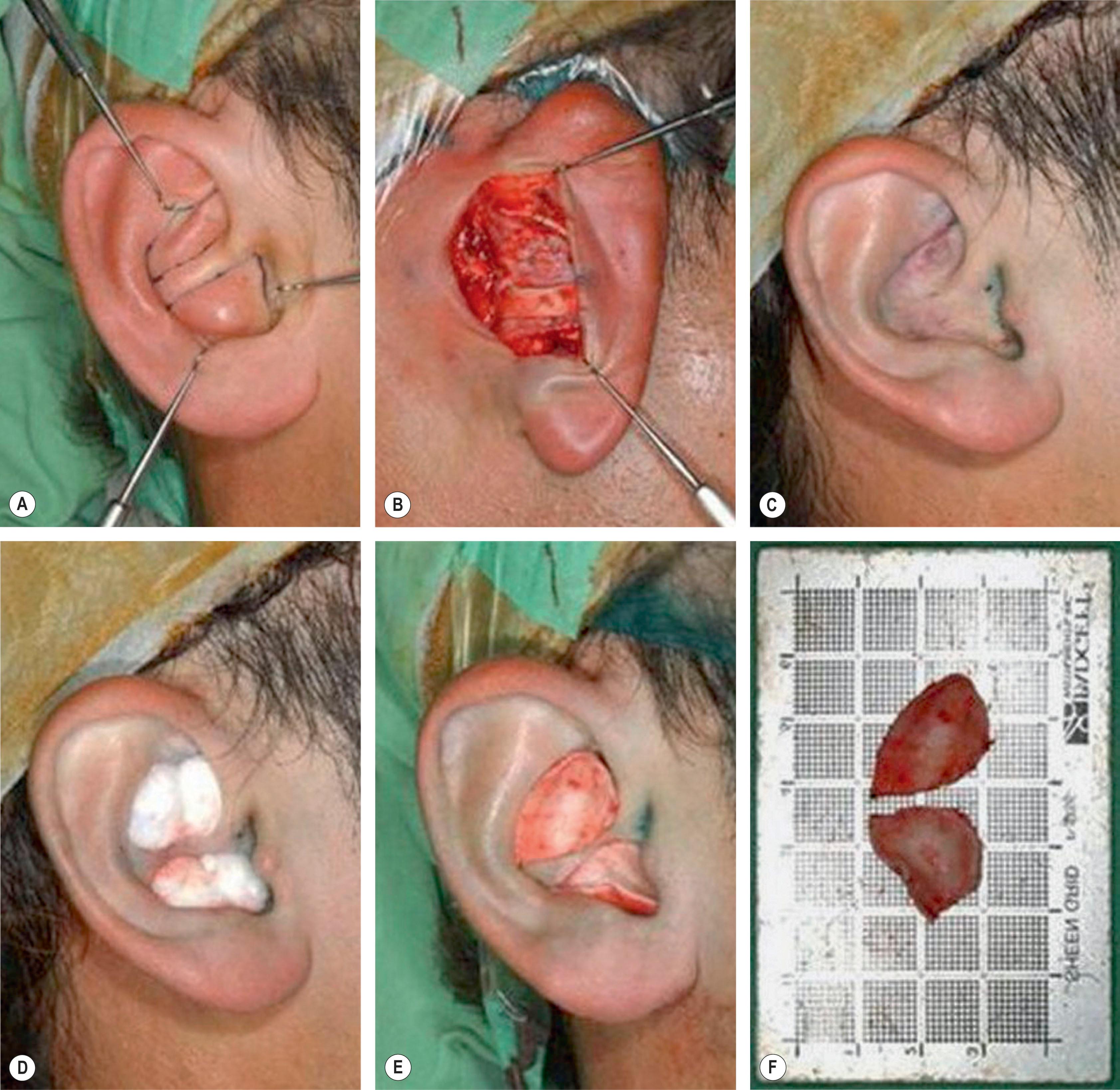
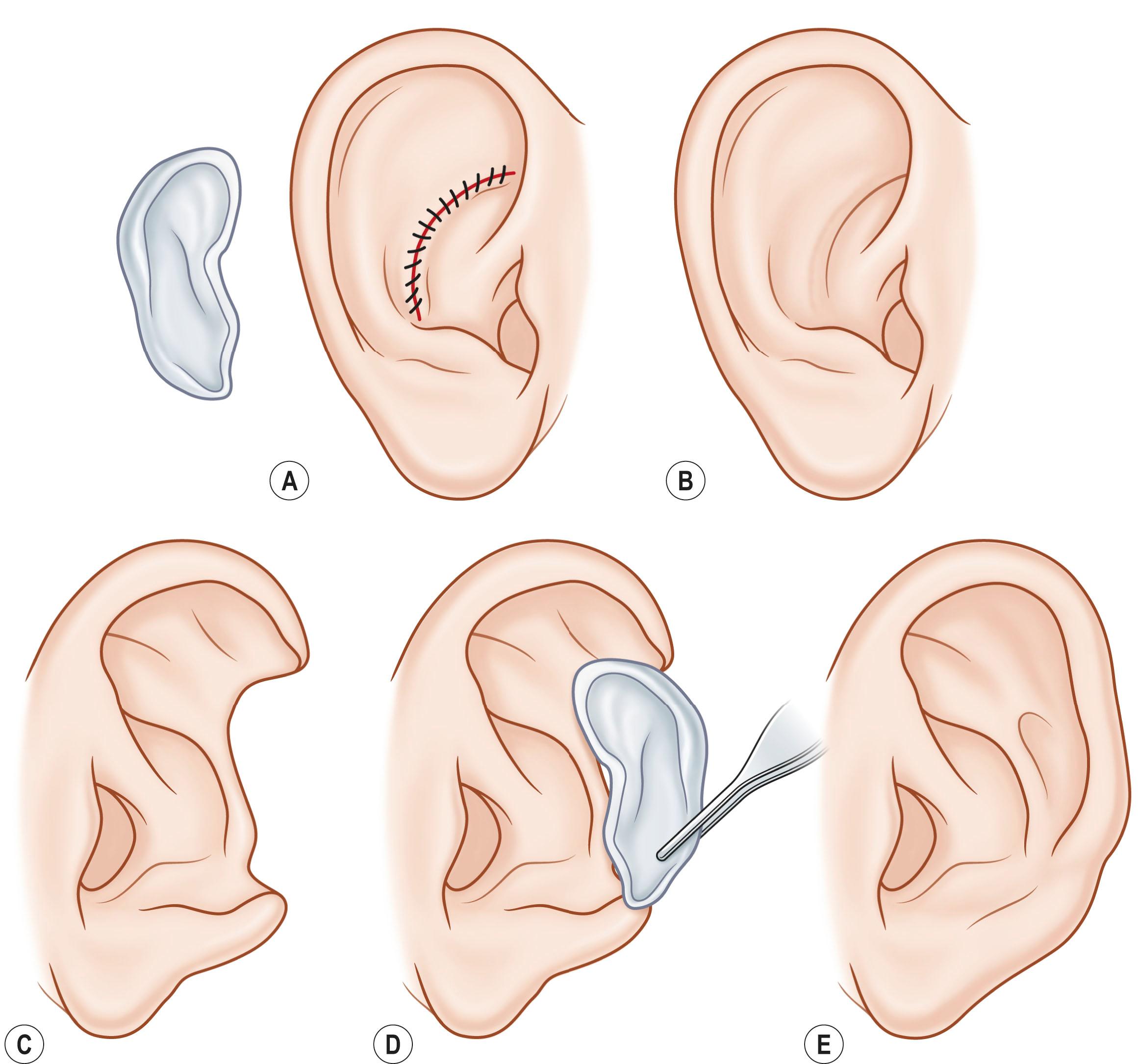
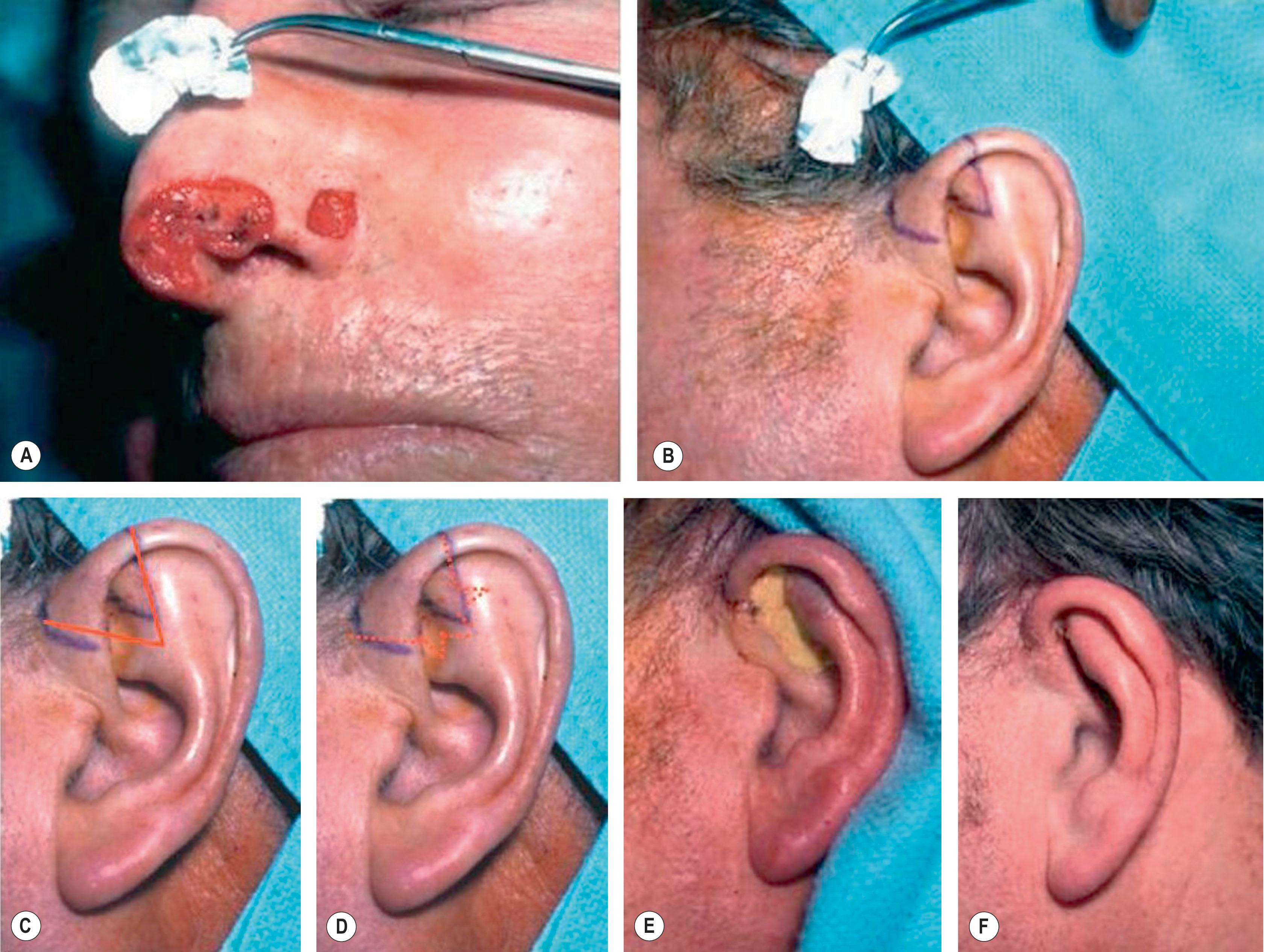
Auricular cartilage graft is often used as a framework for ear reconstruction or auricular deformity correction as reported by Brent, Ono et al ., Firmin et al ., and others. Fig. 19.3 presents an example of harvesting and the use of autogenous conchal cartilage graft for repairing partial ear defect. In addition, conchal cartilage can also be used as single-layered grafts for nasal, tarsal, and nipple reconstruction. Fig. 19.4 demonstrates the application of laminated conchal cartilage graft for correcting saddle nose deformity.
The other important application of auricular cartilage is to transfer as a composite chondrocutaneous graft for nasal reconstruction. How to aesthetically manage the donor site of auricular composite graft is important for its successful application. Singh and Bartlett have summarized several techniques to properly deal with the donor site of free auricular composite grafts according to different applications. These techniques are described as follows :
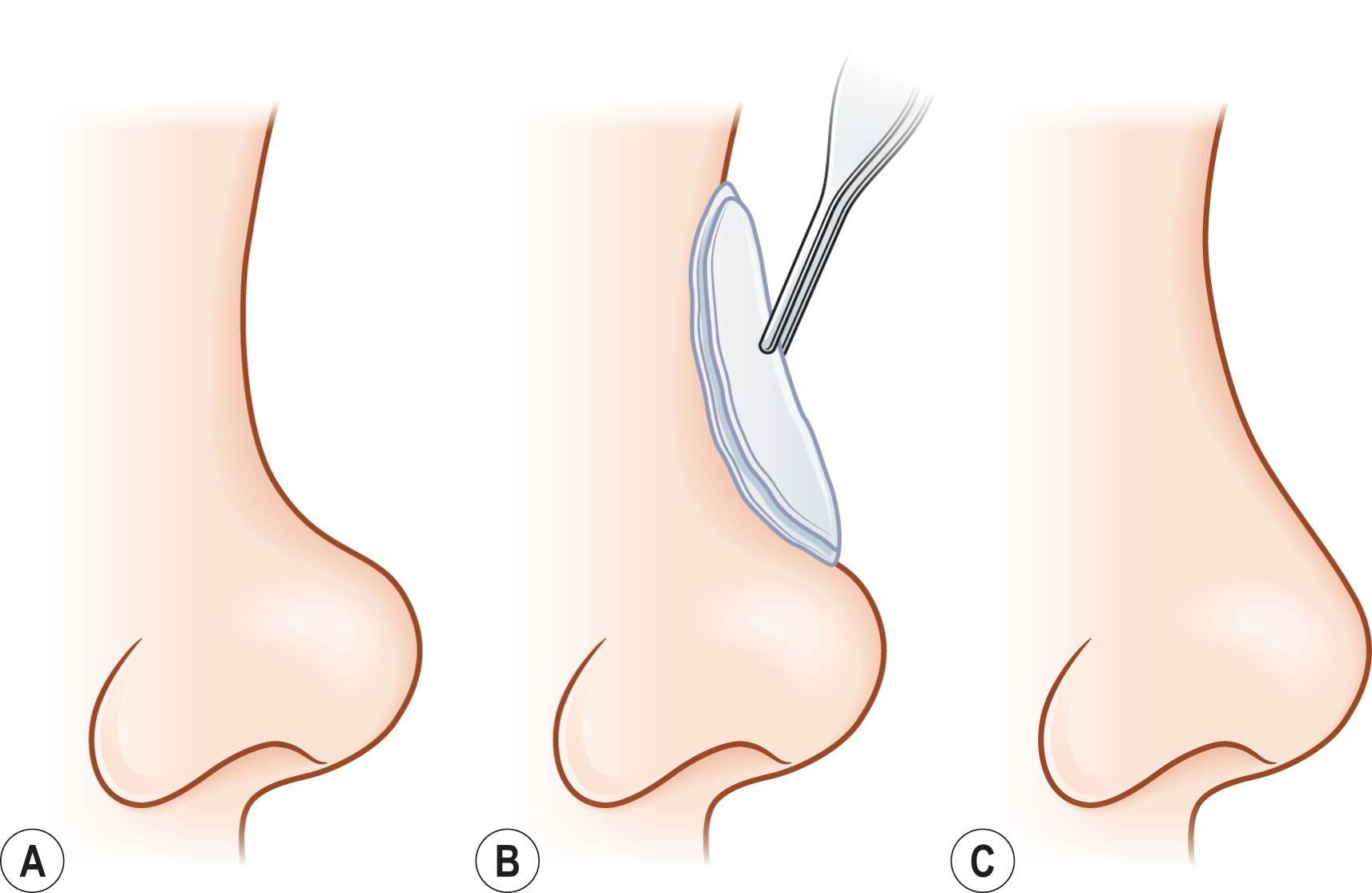
Technique 1: For less than 1 cm composite graft, it can be harvested from the root of the helix and the dog-ear is run anteriorly toward the hairline with primary closure of the defect ( Fig. 19.5 ).
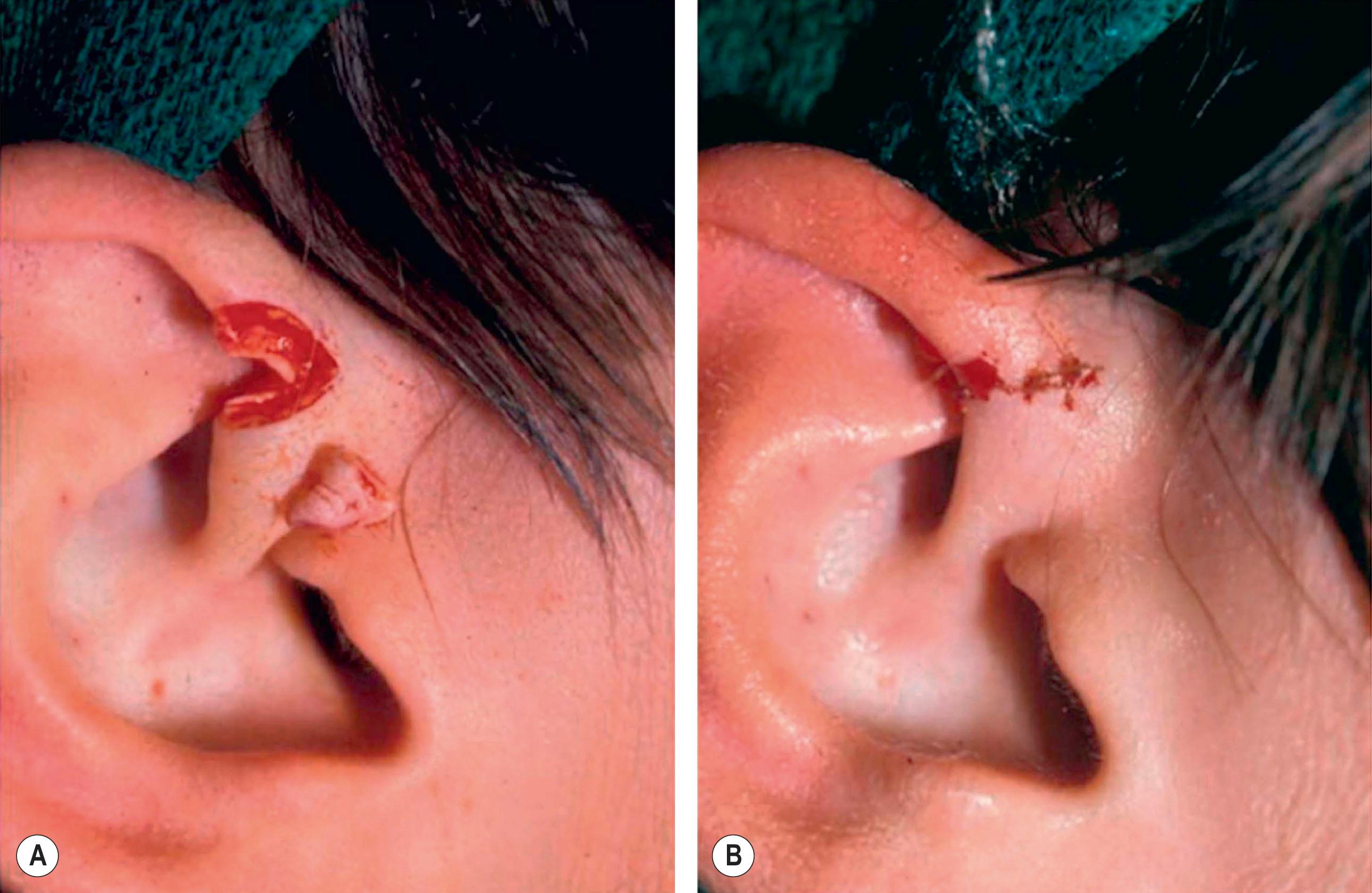
Technique 2: It is designed to close the donor site wound of the composite graft with a cartilaginous base of 1 to 1.5 cm, which is usually needed for repairing a wider defect of the alar rim. Fig. 19.6 demonstrates the surgical technique for repairing a donor site of such a defect.

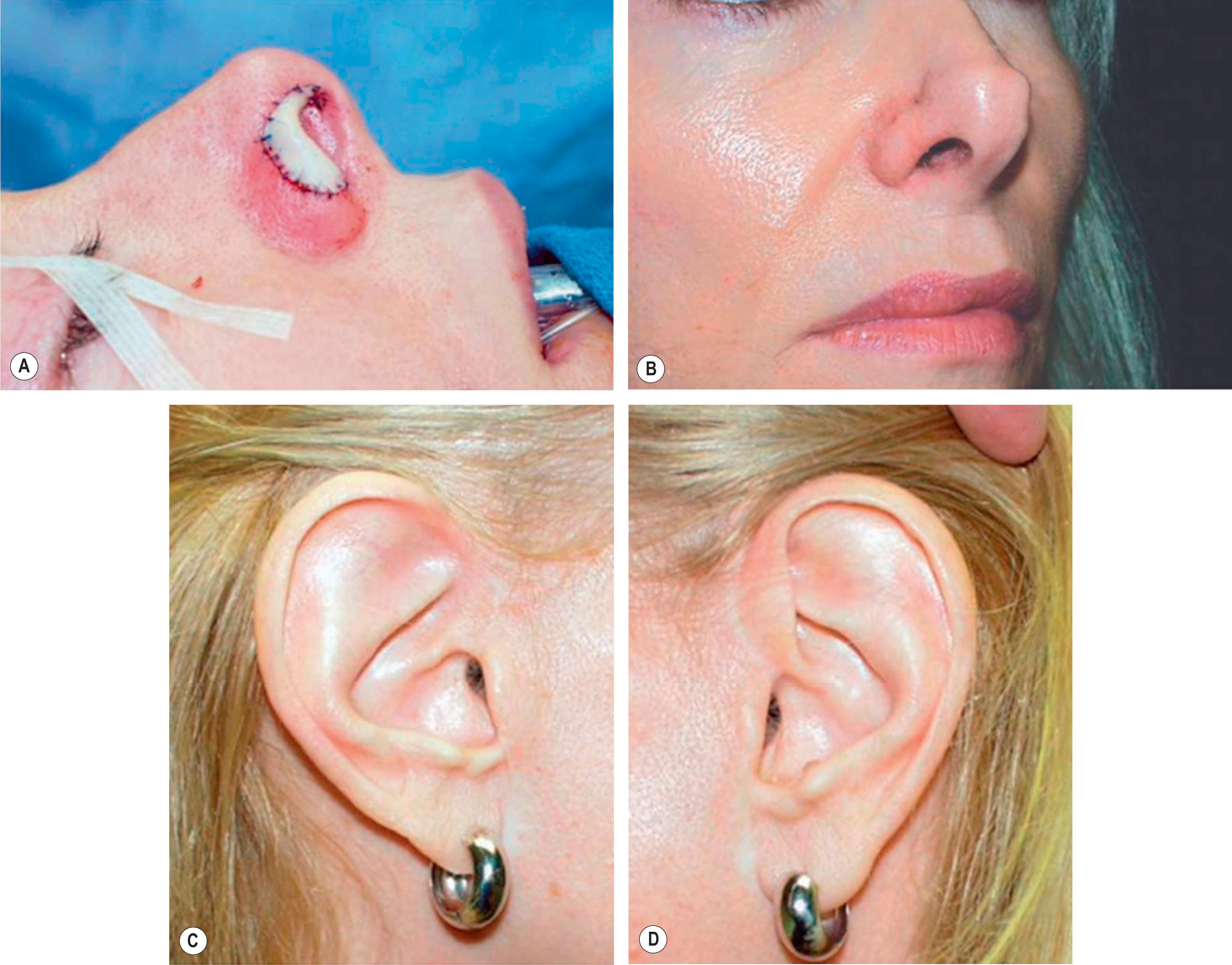
Technique 3: For repairing a nasal defect with short vertical dimension (height), the composite graft can be harvested from the anterior aspect of the helical root and the dog-ear must be run superiorly and inferiorly. As shown in Fig. 19.7 , this technique can provide adequate tissue for the nasal reconstruction and an aesthetic closure without disturbing the size of the ear.
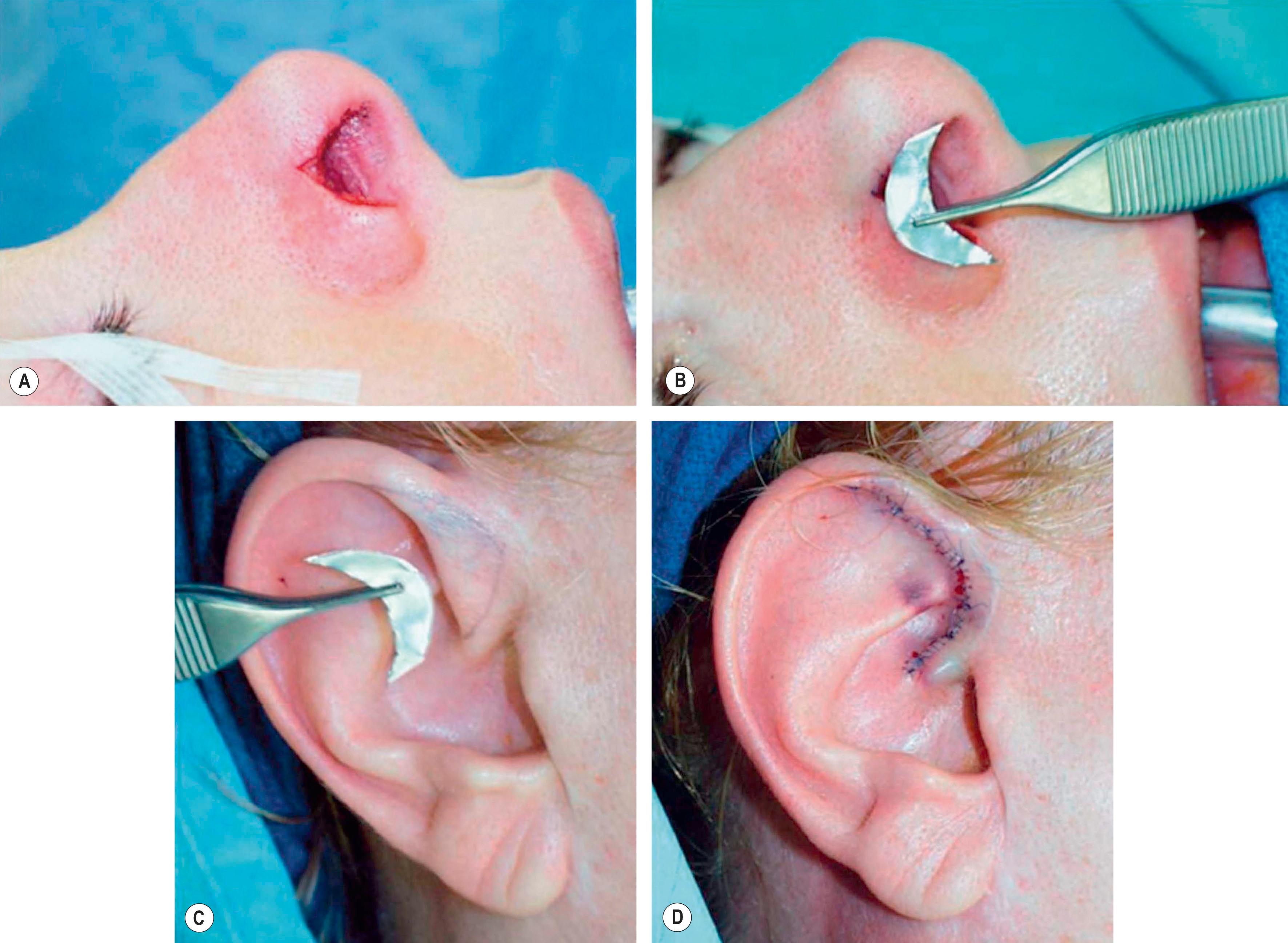
Technique 4: For harvesting grafts with width of 1 to 1.2 cm from the base of the helix, the defect may be closed primarily by advancing the helical rim forward. The possible resulting overprojection of the ear might be addressed with a postauricular incision and a scaphomastoid suture to match the prominence with the contralateral ear ( Fig. 19.8 ).
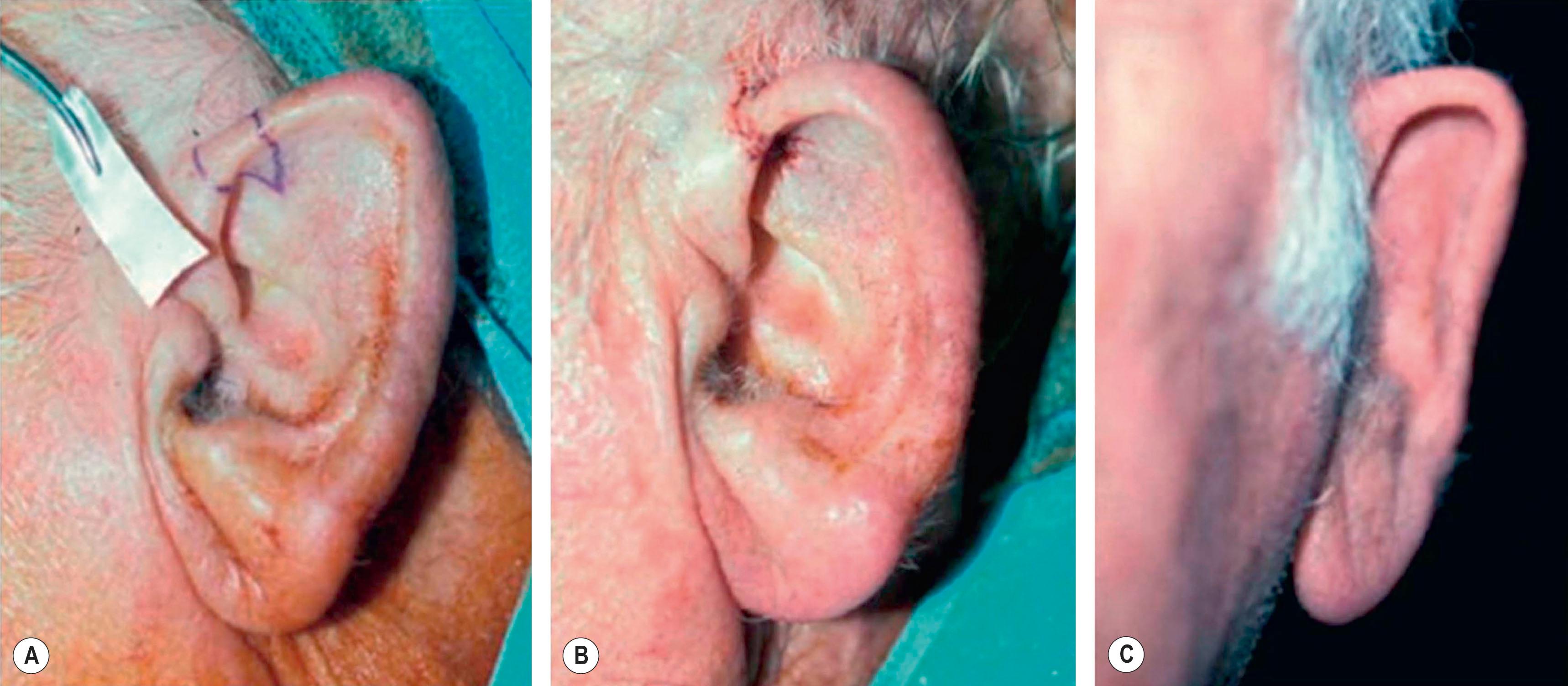
Technique 5: After harvesting composite graft wider than 1.5 cm from the base of the helix, the closure of such a wound becomes more intricate. A simple helical advancement would result in significant distortion and overprojection ( Fig. 19.9 ). To overcome this, a V-shaped wedge of skin is harvested, but a “half-star” pattern of cartilage at the apex of the V is taken ( Fig. 19.10C–E ). In addition, a postauricular incision with a scaphomastoid suture is needed. With these procedures, this technique can prevent cupping of the ear with closure ( Fig. 19.10F ).
When an extended skin graft component is needed with the composite graft, the composite tissues can be taken either preauricularly or postauricularly as demonstrated by the line drawings in Fig. 19.11 .
The above described techniques provide simple methods to primarily close the wounds of auricular chondrocutaneous composite grafts with appreciable aesthetic outcomes. Other methods of rotational flaps or skin grafts have also been described in the literatures. Importantly, functional and aesthetic aspects should be well balanced for both repair site and donor site when a physician decides to harvest an auricular composite chondrocutaneous graft with a particular size and shape.
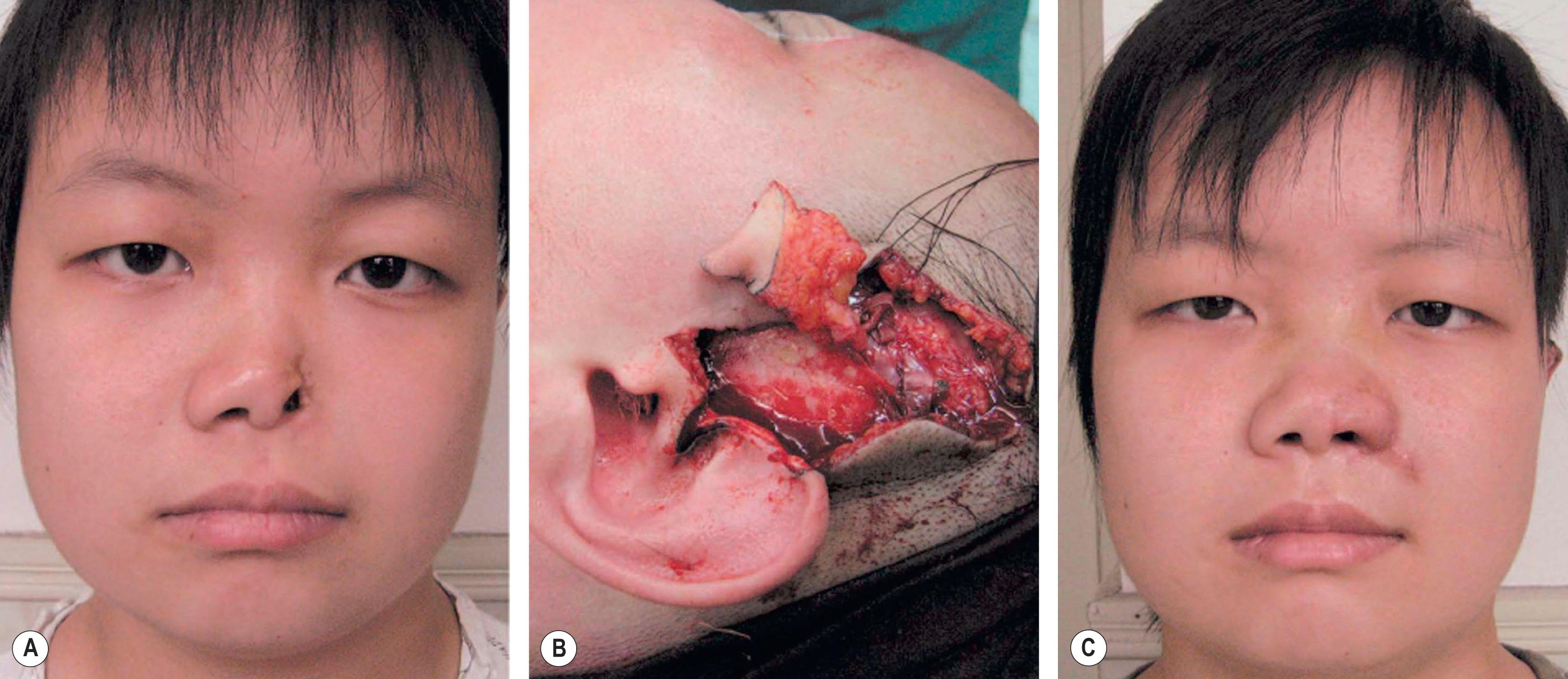
One of the concerns for clinical application of free auricular composite grafts is their limited available size due to the lack of immediate blood supply after transplantation. In contrast, microvascularly transferred auricular composite grafts can overcome this limit and is particularly useful in repairing large size nasal defect. Zhang et al . reviewed their experiences of surgical treatment of large nasal defect with vascularized preauricular and helical rim flaps that are based on the superficial temporal vessels in 63 clinical cases. The repaired deformities include unilateral alar defect, alar and sidewall defects, tip and columellar defects, entire lower third of the nose missing, and composite defects involving cheek and maxilla. The total flap survival rate reached 97%. The results demonstrate that such an approach of using vascularized preauricular and helical rim flap is a reliable method for reconstructing nasal defects. Fig. 19.12 demonstrates the surgical technique for repairing alar lobule defect with vascularized helical rim composite tissue and the preauricular skin.
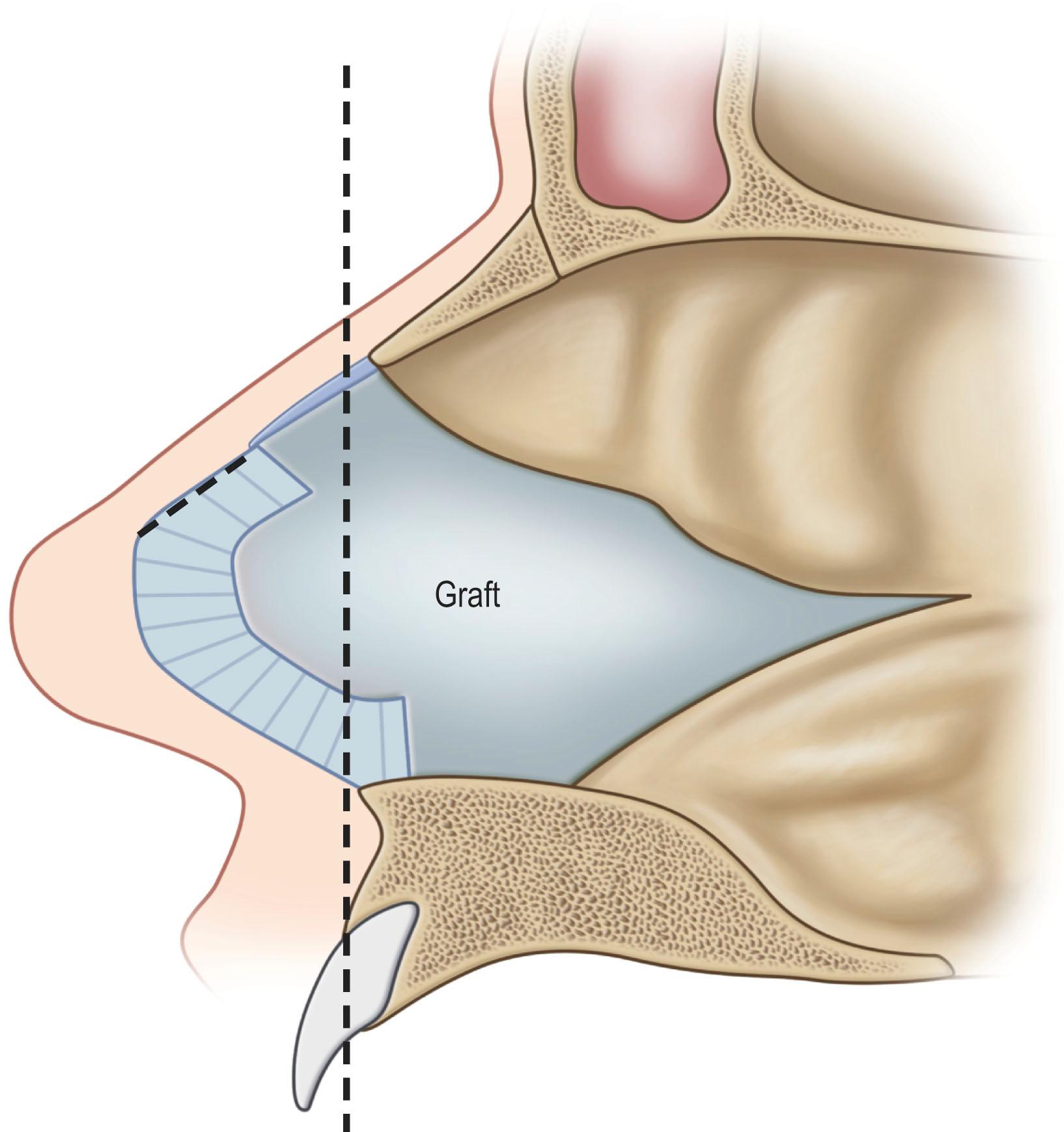
Although limited in its available amount, nasal cartilage has been employed as a composite chondromucosal graft for eyelid reconstruction. Septal cartilage is an important source of nasal cartilage graft. As reported by Murrell et al ., the septal cartilage can be accessed via a hemitransfixion incision with dissection around the caudal margin of the quadrangular cartilage. After both sides of mucoperichondrium are raised, the septal cartilage can be harvested. Importantly, as shown in Fig. 19.13 , an “L-shaped” septal strut should be preserved to give nasal support and avoid nasal collapse. Nevertheless, the amount of “L” strut cartilage necessary to provide good support can vary greatly depending on the strength, thickness, and dimensions of the nasal septum and other nasal tissues (i.e., upper lateral cartilages, lower lateral cartilages, nasal bones, etc.). As early as 1962, Millard published his work of repairing eyelid defect with a chondromucosal graft harvested from nasal septum. Later, Mustardé also described the technique in the book of Repair and Reconstruction in the Orbital Region .
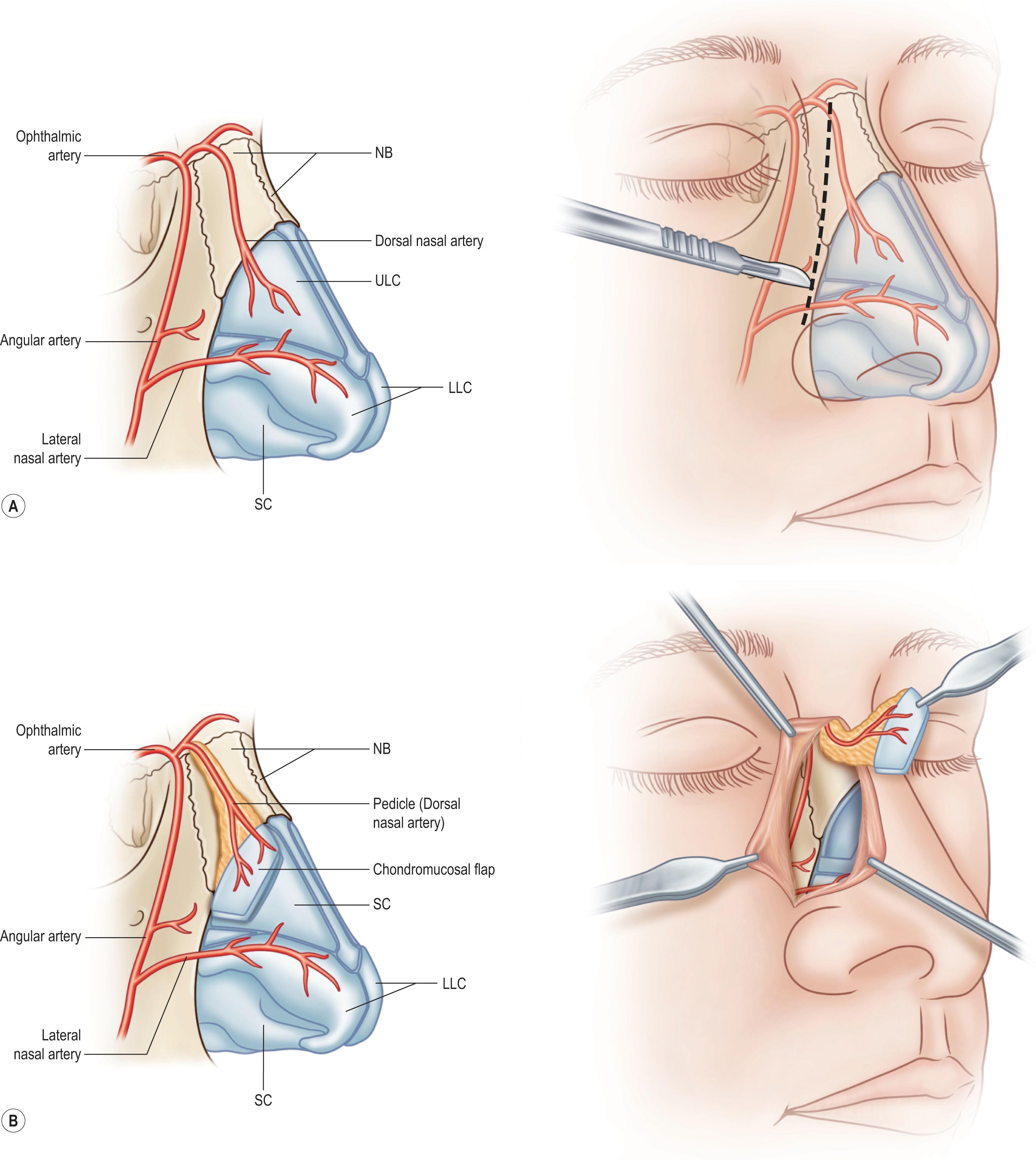
The other available region for harvesting nasal chondromucosal graft is the upper lateral nasal cartilage, as reported by Tessier in 1979. In clinical practice, repairing a large-size defect of upper eyelid is always a challenge. Scuderi and colleagues have developed a surgical technique to address such a concern. In their report, a pedicled nasal chondromucosal flap was designed along the lateral nasal wall based on the terminal branch of the dorsal nasal artery. The flap includes the subcutaneous tissues down to the periosteum and the cranial portion of the upper lateral cartilage. It can be harvested either unilaterally or contralaterally and a skin graft is applied for cutaneous coverage. In their reported 15 patients, the flap was viable in every patient and satisfactory functional recover was achieved, indicating this one-stage procedure can reconstruct a thin and mobile eyelid. Fig. 19.14 demonstrates the design and surgical procedure as well as its clinical outcome. In addition to eyelid repair, septal cartilage graft has also been used for dorsal augmentation, tracheal repair, and extended septal graft for controlling the projection shape of nose tip.
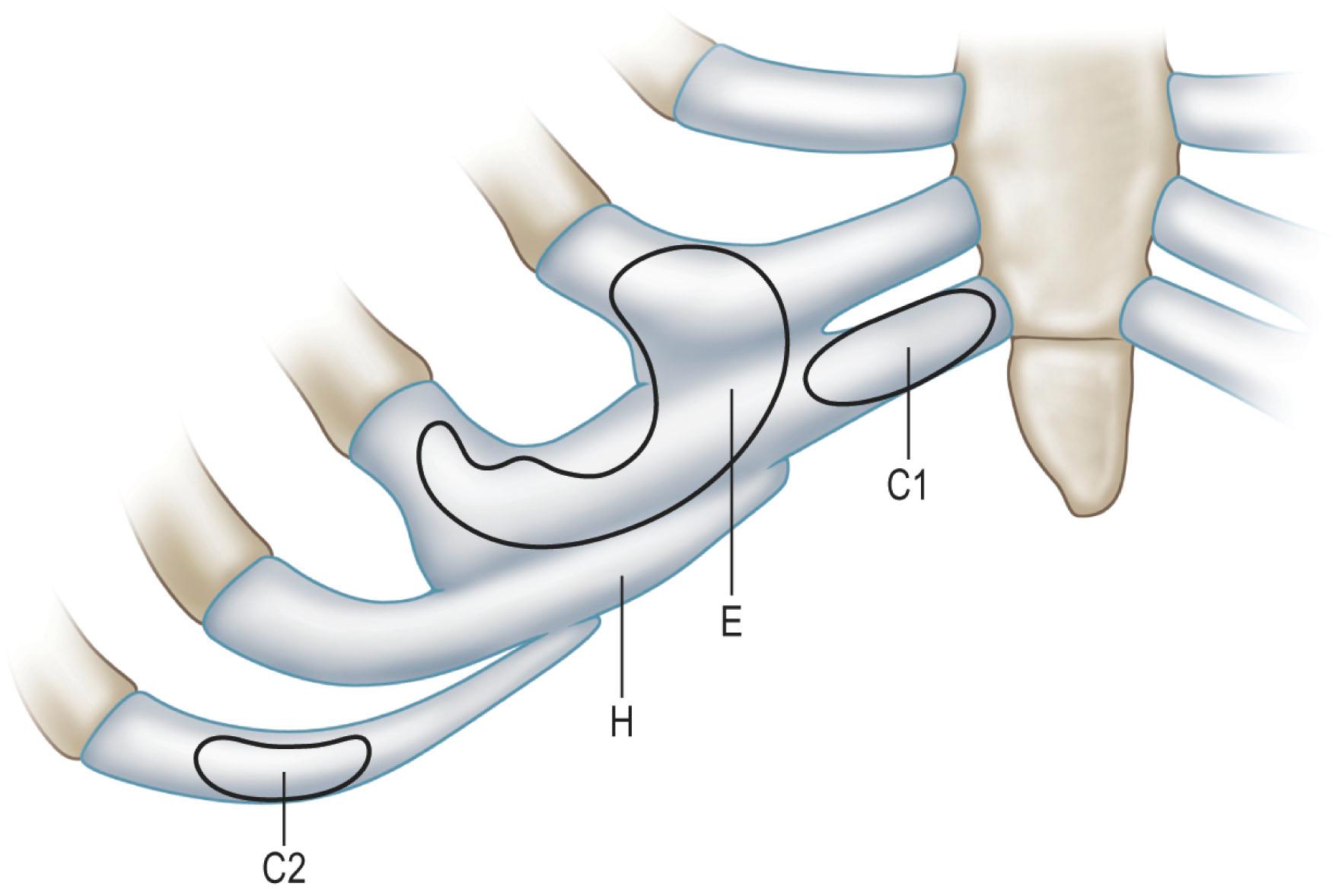
Costal cartilage may serve as the best donor site for cartilage graft in terms of available tissue amount and the mechanical strength. Autologous rib cartilage can be virtually contoured into any desired shape and it can retain the form and bulk after implantation if basic surgical principles are followed. The costal cartilage graft is often used as a cartilage framework for total ear reconstruction. Tanzer, Thomson, and Brent have respectively described the technique to harvest costal cartilage to construct auricular framework. In the procedure, the synchondrosis of the sixth and seventh cartilages as well as the eighth costal cartilage is harvested, usually along with the perichondrium. Differently, Nagata’s method for total auricular reconstruction requires the harvest of four costal cartilages in the first stage operation and one or two costal cartilages for the second stage operation. Fig. 19.15 represents a schematic illustration of the harvest of rib cartilage designed for ear reconstruction or chin contouring.
In clinical practice, harvest of costal cartilage can be associated with donor site morbidity. Uppal et al . have reported their investigation on morbidity associated with the harvest of costal cartilage in 42 patients who underwent ear reconstruction. The commonest complaints included pain and clicking of the chest wall, which usually peaked in the first week post surgery and gradually diminished over 3 months. The other problems were scar and chest wall deformity. Among them, the most challenging problems are pneumothorax during the surgical procedure and resulting abnormal chest wall contour. This is particularly true for Nagata’s method which requires more and extra cartilage grafts for auricular reconstruction.
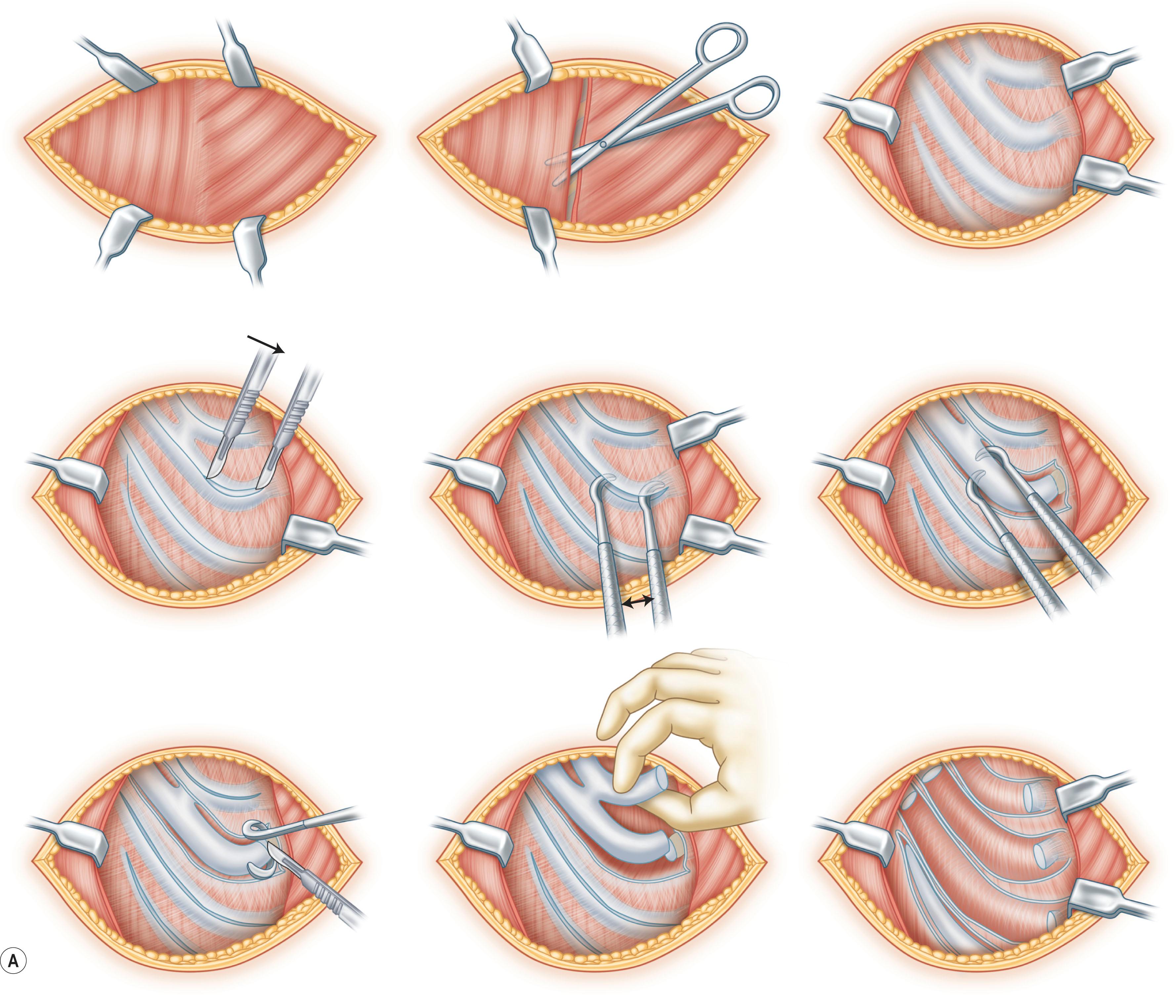
To address this concern, Kawanabe and Nagata developed a new method for harvesting rib cartilage to avoid and prevent intraoperative and postoperative complications and problems. In this modified procedure, the costal cartilages were harvested en bloc with the perichondrium left completely intact at the donor site. In addition, after the fabrication of the auricular cartilage frame, the remaining costal cartilage was cut into small blocks that acted as spacers to fill the dead space formed in the perichondrial pocket. The retained perichondrium not only helps to avoid injury of the pleura, but may also promote cartilage regeneration because of the presence of chondrogenic stem cells. In their investigation of 270 cases of total auricular reconstruction performed using Nagata’s method and the new method of rib cartilage harvesting, the incidence of infection and pneumothorax was reduced to less than 1%. More importantly, there were no postoperative chest wall deformities when costal cartilage was harvested with this new technique. Interestingly, their follow-up study revealed that returned hyaline cartilages were mixed with fibrocartilage with visible margins at 6 months post surgery. Twelve months after the first-stage operation, homogenous hyaline cartilage was observed histologically, and the regenerated cartilages were similar to native costal cartilages in their hardness, which made a second harvest possible. Fig. 19.16 illustrates the harvesting of costal cartilage using the method of retaining perichondrium and returning the remaining costal cartilage to the donor site.
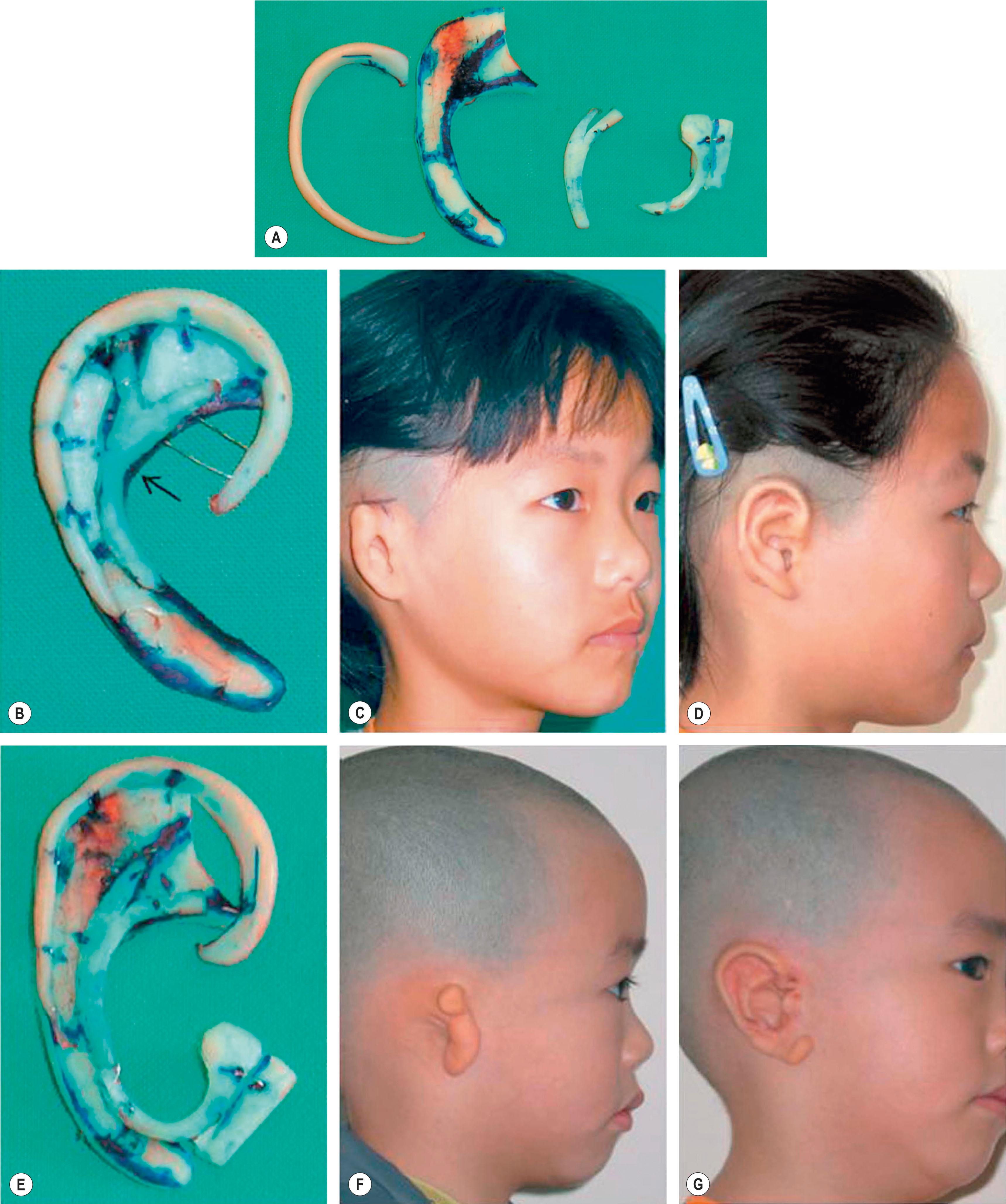
Modification of previously established methods of making auricular framework is also considered as an alternative option to avoid harvesting extra cartilage and thus help to prevent chest wall deformity. As an example, Chin et al . reported several modifications of auricular framework and these methods required less cartilage graft and meanwhile could also generate individualized and harmonious ear frameworks to meet the need for satisfactory three-dimensional (3D) outline of a reconstructed auricle. The framework may consist of the helix, the base frame, the Y-shaped antihelical complex, and the tragus attached with an additional cartilaginous cube depending on individualized need ( Fig. 19.17A–D ). In addition, bone cement is used as the support material during the ear elevation stage, and therefore extra costal cartilage harvesting is unnecessary. Fig. 19.17E–G demonstrates the clinical outcome of reconstructed ear with modified frameworks based on the individualized 3D auricle structures.
In addition to auricular reconstruction, rib cartilage graft also has other applications, including reconstruction of significant saddle nose deformity, treatment of maxillonasal dysplasia (Binder's syndrome), nipple reconstruction, for septorhinoplasty, and tracheal reconstruction.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here