Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The urinary system, volume homeostasis, osmoregulation, and composition of body fluids are all altered in normal pregnancy. There are also hemodynamic changes involving cardiac output and blood pressure. Knowledge of these changes permits earlier detection of dysfunction as well as better management of pregnant patients with kidney disease and/or hypertension. In the fourth revision of this chapter, besides an updated review of renal physiology during pregnancy, recent data on the role of relaxin in mediating renal hemodynamic changes of pregnancy as well as the role of anti-angiogenic factors in the pathogenesis of preeclampsia are discussed extensively.
The urinary system, volume homeostasis, body fluid composition, and osmoregulation are all profoundly altered in normal pregnancy. There are also marked changes in systemic hemodynamics involving cardiac output and blood pressure. Knowledge of these physiological adaptations permits earlier detection and facilitates management of renal disease and hypertension during pregnancy. In the fifth revision of this chapter, the authors revise and update the previous edition co-authored with Marshall Lindheimer, former senior and an original author of the chapter. As before, space limitations lead us to refer on occasion to previous editions of the book especially for details from the older literature.
Information about renal anatomy during normal pregnancy is limited, but it appears that the kidney becomes larger. Autopsy studies are obviously scarce, but in one unique and large series combined kidney weights of normotensive women dying during or shortly after gestation were higher than normal values for nonpregnant individuals. However, details about the cause of death, which could have affected kidney weights, were limited. Renal weight also increases during pregnancy in rats, the evidence suggesting that this is due to increased water content, as renal dry weights are similar in gravid and nonpregnant rats. In one study in which renal biopsy specimens were obtained from normal gravidas (usually during cesarean section), the light microscopic appearance was described as similar to that in nonpregnant subjects [cited in ]. But data from both autopsy material and renal biopsies performed in the last trimester on 12 normal gravidas suggested that glomerular size, but not number of cells, may be increased in pregnant women. Detailed descriptions of the kidneys of normal pregnant women or animals using electron microscopic or immunofluorescence techniques are not available.
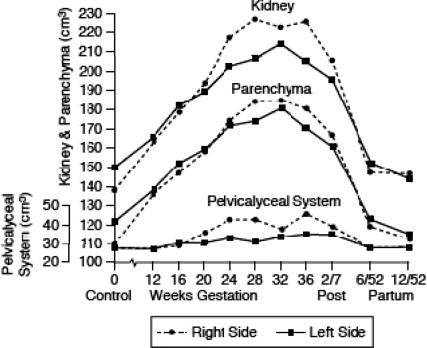
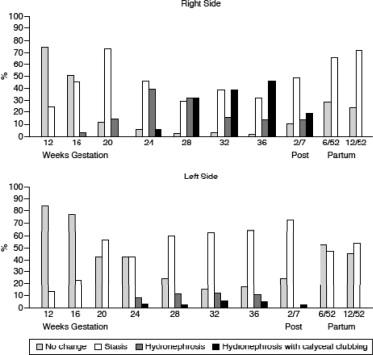
Starting in the first trimester, overall renal dimensions—length, width, and thickness—increase and peak during the third trimester at 1 cm above prepregnant values. These changes, documented by ultrasonography and pyelography, translate into an overall increase in renal volume of ~50% by the end of pregnancy ( Figure 81.1 ). Both renal parenchymal and pelvicalyceal volumes enlarge, although the latter typically begins to rise somewhat later during the second trimester. Renal parenchymal volume enlarges most likely due to increases in both vascular and interstitial fluid volume; there is little evidence for cellular hyperplasia or hypertrophy. Renal size and volume estimated by ultrasonography or pyelography in the immediate puerperium are also increased. Of interest, roentgenograms performed shortly after delivery and repeated six months later demonstrated that renal length had decreased ~1 cm between the two exams [cited in ]. The well-documented dilation of the upper ureter, renal pelvis, and major and minor calyces, which affects the vast majority of gravidas at term, is particularly prevalent on the right side. Consequently, urinary stasis and hydronephrosis (either with or without calyceal clubbing) are common physiological occurrences in human pregnancy ( Figure 81.2 ), and usually do not reflect pathologic obstruction. Although the more severe signs of this physiological obstruction resolve at least by 6 weeks after delivery, evidence for urinary stasis persists in many women at 12 weeks postpartum.
The causes of the ureteral dilation are controversial. Both humoral changes and mechanical obstruction have been implicated. Smooth muscle relaxation occurs in several organs during pregnancy, and some authors reported ureteral dilation in nonpregnant humans and animals administered estrogen–progestin derivatives. Ureteral dilation may occur in primates with placentas that secrete hormones but absent fetuses, and ultrasonography shows that the ureter dilates before the uterus has enlarged sufficiently to cause obstruction ; nor is the dilation relieved by prolonged catheterization.
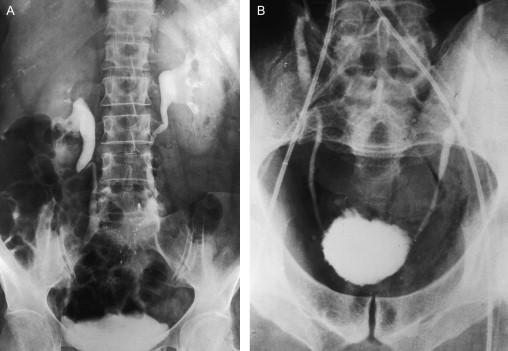
The obstructive theory is supported by the observations of marked exacerbation of intraureteral pressure when third trimester gravidas were in a supine or standing position, and significant amelioration upon removal of the obstructive influence of the gravid uterus by placing the subject in the lateral decubitus or knee–chest position, or by cesarean delivery of the fetus. Moreover, the increased pressure was noted only above the pelvic brim. These data are supported by the elegant studies of Dure-Smith, who combined in vivo and postmortem observations and concluded that ureteral dilation stops at the level of the true bony pelvic brim where the ureter crosses the iliac artery ( Figure 81.3 ). At that junction, one may see a pyelographic filling defect, called the “iliac sign” ( Figure 81.3 ). Although compelling, the data are not conclusive, because Waldeyer’s sheath, a connective tissue enveloping the ureters as they enter the true pelvis, hypertrophies during pregnancy and could restrict hormone-induced dilatation below the pelvic brim.
A related theory is that dilation of the ovarian and uterine veins (especially those on the right) during pregnancy obstructs the ureters. The “ovarian vein syndrome” (ureteral colic ascribed to obstruction secondary to enlargement of the ovarian vein) was described in a patient taking oral contraceptives, an observation that combines the humoral and obstructive theories.
Also supporting obstruction as a cause of the physiological dilation is the occurrence of an “overdistention” syndrome in late gestation. This clinical entity caused by exaggerated ureteral dilation is characterized by marked hydronephrosis, abdominal pain, increases in serum creatinine, and in some cases, hypertension. Some of these patients were successfully managed with ureteral stents, which were removed postpartum without recurrence of signs and symptoms. Perhaps the most serious consequences of physiological obstruction during pregnancy are acute urinary retention and nontraumatic rupture of the ureter, but whether these entities reflect extreme instances of physiologic ureteral dilatation or underlying pathology is not clear.
There are other clinical ramifications to the anatomical changes in the urinary tract during pregnancy. First, acceptable norms of kidney size increase by 1 cm if assessed during pregnancy or immediately postpartum, and reductions in renal length noted several months after delivery need not be ascribed to pathological decrements in renal parenchymal mass. Second, ureteral dilation and urinary stasis may contribute to the propensity of women entering pregnancy with benign asymptomatic urinary tract infection to develop frank pyelonephritis (see below). Third, ureteral dilation may result in a higher frequency of vesicoureteral reflux, further predisposing to symptomatic infection, but the presence of increased reflux in gravid women is disputed. Finally, the dilated urinary tract may contain substantial urine volumes that can introduce errors in the collection of timed urine volume. This eventuality may be minimized, however, by having the patient hydrated and positioned in lateral recumbency for 1 h prior to starting and again before completing the collection. A modest diuresis minimizes the dead-space error and concurrently ensures that any residual urine in the urinary tract or bladder is dilute and of recent origin.
Ureteral dilation mostly abates by the 12th postpartum week, and therefore imaging of the urinary tract should be deferred to this point, if possible. However, minor but significant dilation may persist in as many as 11% of parous women who have no history of urinary tract infection. This, again, suggests that obstruction may be a significant cause of changes in the ureter during pregnancy.
Several carefully conducted serial studies in pregnant women, in which glomerular filtration rate (GFR) and effective renal plasma flow (ERPF) were measured by renal clearances of inulin and p -aminohippurate, were conducted during the 1950s and early 1960s. The results convincingly showed that both GFR and ERPF increase during pregnancy, but there was considerable controversy regarding the time course of these changes [reviewed in ]. All concurred that renal hemodynamics rose during the first trimester; the discrepancies concerned late pregnancy, i.e., whether peak increments in GFR and/or ERPF were sustained until term. These divergent results most likely reflect a number of methodological pitfalls, then unappreciated, which can confound the results of renal function tests performed during pregnancy. These potential problems are reviewed in detail elsewhere, and here we highlight two of them: the need to impose a high urine flow with hydration, because the dilated ureter introduces dead-space errors, and to position the subject in lateral recumbency. The latter is particularly important in late pregnancy, because an upright or supine posture may lead to marked decrements in GFR or ERPF.
More recently, investigators reexamined the time course of renal hemodynamic changes in pregnancy, often combining serial 24-h endogenous creatinine clearances with both inulin and p -aminohippurate renal clearances and focusing on the first and last few weeks of gestation ; ( Figure 81.4 ). In some studies, nonpregnant control data were obtained prior to conception and postpartum. Although not all are methodologically flawless, they provide important information summarized as follows: GFR normally increase during the luteal phase of the menstrual cycle, continue to rise early in pregnancy, reaching peaks 40–65% above nonpregnant levels by the second trimester. These increments are maintained at least until the 36th gestational week after which a modest decrease in GFR may occur. Three months postpartum, GFR values are similar to those measured before pregnancy.

ERPF also increases in the luteal phase of the menstrual cycle and then markedly during gestation reaching values 50–85% above prepregnancy levels during the initial two trimesters ( Figure 81.4 ); Near term, however, ERPF seems to decrease ~25%, although it still remains considerably above nongravid values. In general, filtration fraction decreases early in gestation and returns to or towards nonpregnant levels in the last trimester.
Given the tremendous increase in GFR and ERPF, the question arises as to whether renal vasodilation is maximal during pregnancy, or whether gravidas possess a “renal functional reserve” similar to that observed during protein loading in nonpregnant subjects. The results of several studies are equivocal. Amino acid infusions consistently increase GFR further in pregnant women, but results of high protein meals are inconclusive. Finally, glycine infusions increase GFR in gravid rats.
Our understanding of mechanism(s) underlying the gestational rise in ERPF and GFR continues to evolve. In part due to both ethical and logistical concerns, most studies designed to determine mechanisms of gestational changes in renal function have utilized animal models as there are several species also known to manifest increases in GFR and ERPF during pregnancy [referenced in ]. Thus, by applying the renal micropuncture technique to Munich-Wistar rats during midgestation, the period when ERPF and GFR are maximally increased in this species, Baylis demonstrated the gestational rise in single nephron GFR (SNGFR) to be secondary to an increase in glomerular plasma flow, the latter due to a decline in renal vascular resistance. In her rat model, transglomerular hydrostatic pressure difference remained unchanged because there were comparable decreases in both afferent and efferent arteriolar resistances. Plasma oncotic pressure was not significantly different between nonpregnant and midterm pregnant rats and thus not involved in altering SNGFR. Because the animals were in filtration equilibrium, only a minimum value for the ultrafiltration coefficient, K f could be calculated, which was similar between nonpregnant and midterm pregnant rats; nevertheless, this determinant of glomerular ultrafiltration most likely contributed little to the gestational rise in SNGFR in the gravid rat model. To summarize, SNGFR rises mainly because glomerular plasma flow increases in the gravid rat model.
Whether similar mechanisms occur in pregnant women is unknown as glomerular dynamics cannot be directly measured. Moreover, human glomeruli may be in filtration disequilibrium, a condition in which alterations in ERPF are predicted to have less impact on GFR. Nevertheless, the parallel increases in ERPF and GFR suggest a similar mechanism governing the rise in GFR in gravid women.
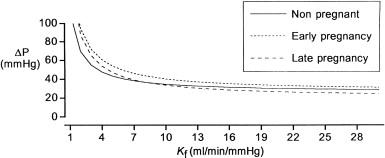
Using an indirect approach, investigators measured the fractional clearance of neutral dextrans ( C dextran / C inulin ) in normal pregnant women serially studied throughout early and late gestation followed by retesting 6 weeks postpartum. Such data can be analyzed by mathematical models, which incorporate clearance values and plasma oncotic pressures to predict glomerular capillary pressure, the ultrafiltration coefficient ( K f ) and glomerular capillary membrane porosity. Permselectivity to neutral dextrans was altered during gestation ( Figure 81.5 ), and the theoretical analysis of the sieving curves, using two different models, suggested that hyperfiltration during pregnancy was mainly due to increments in ERPF with a minor contribution from decreased glomerular oncotic pressure (the latter being greater during late gestation). Membrane porosity appeared to be altered, but comparable to micropuncture studies in rats, there was no evidence of increased glomerular capillary pressure in human pregnancy ( Figure 81.5 ). It should be emphasized, however, that this approach is theoretical in nature being dependent on several assumptions that may or may not be valid.
Further insight into the causes of the altered renal hemodynamics during pregnancy arose from studies in a rat model. Conrad adapted methodologies developed by Gellai and Valtin for measurement of renal function in chronically instrumented, conscious rats and applied them to pregnancy. Because physiology is markedly perturbed by anesthesia and surgical stress and the effects of anesthetics and surgical stress can differ in the nonpregnant and pregnant states, studies in chronically instrumented, conscious animals are an essential first step in the investigation of mechanisms underlying maternal circulatory adaptations to pregnancy. Thus, when the same chronically instrumented, conscious rats were serially studied before, during, and after pregnancy, both renal vasodilation and hyperfiltration were observed throughout most of gestation, making it an excellent model to explore the mechanisms underlying these changes.
Extracellular and plasma volumes dramatically increase during pregnancy (although most studies suggest after the peak in ERPF and GFR). Acute expansion of plasma volume by 10–15% failed to increase the GFR, SNGFR, or glomerular plasma flow in virgin female Munich-Wistar rats. Because volume expansion can suppress tubuloglomerular feedback activity, it could mediate the gestational increases in glomerular plasma flow and SNGFR. However, tubuloglomerular feedback activity was not suppressed in gravid Munich-Wistar rats, rather the mechanism was reset to the higher SNGFR of pregnancy suggesting that volume expansion of pregnancy is actually perceived as “normal.” This conclusion supports the “arteriolar underfilling” hypothesis, which states that a primary reduction in systemic vascular resistance precedes secondary vascular filling during pregnancy; however, the two events are tightly linked and virtually inseparable, although some investigators have discerned a temporal dissociation. (Also, see the section Significance of the Volume Changes During Pregnancy.)
Whether chronic volume expansion can raise ERPF and GFR to pregnancy levels is difficult to test. Most instances of chronic volume expansion that occur naturally are pathological in nature, for example, congestive heart failure or cirrhosis, and these are conditions where renal function is usually reduced rather than elevated. However, in the rare condition of primary mineralocorticoid excess, which is associated with volume expansion, GFR increases but not to the same degree as observed in pregnancy. Interestingly, chronic administration of either arginine vasopressin (AVP) or oxytocin to chronically instrumented rats permitted water ad libitum expands total body water and reduces plasma osmolality ( P osm ), as well as markedly increases ERPF and GFR. Thus, it is possible that chronic volume expansion contributes to the initiation and/or maintenance of elevated ERPF and GFR during pregnancy. Another possibility is that vascular filling consequent to primary arteriolar vasodilation in the kidneys and elsewhere may be permissive for the rise of GFR, in parallel with ERPF.
Mating female rats with vasectomized males produces pseudopregnancy—a condition physiologically mimicking the first half of rat gestation, but in the absence of fetoplacental development. This state reproduces the increases in ERPF and GFR that are observed during early pregnancy. Thus, maternal factors alone can induce changes in the renal circulation.
Davison and Noble reported that the 24-h endogenous creatinine clearance increased by 20% during the luteal phase of the menstrual cycle in women. Other investigators corroborated this finding either by using the renal clearance of creatinine, 51Cr-EDTA, or inulin. Furthermore, ERPF measured by the renal clearance of PAH or [ 125 I] hippuran was noted to be increased in two studies but not in another. Thus, increases in ERPF and GFR are observed in the luteal phase, albeit to a lesser degree compared to pregnancy. This observation may shed light upon underlying mechanisms, because several hormones that increase during the luteal phase of the menstrual cycle rise even further in early pregnancy (e.g., the ovarian hormones, progesterone, and relaxin, see below).
Neither acute nor chronic administration of estrogen(s) to humans or laboratory animals influences ERPF or GFR, although the hormone can clearly increase blood flow to other nonreproductive and reproductive organs. On the other hand, progesterone (or possibly progesterone metabolite(s) ) may contribute to renal circulatory changes in pregnancy. Chesley and Tepper administered 300 mg/d of progesterone intramuscularly to 10 nonpregnant women for 3 1/2 days and observed a 15% increase in C IN and C PAH . They speculated that longer administration of the hormone might produce larger increases in GFR and ERPF akin to normal gestation. Atallah et al. who studied nine nonpregnant women demonstrated that a rise in circulating progesterone from 7 to 30 ng/mL was associated with a significant rise in endogenous C cr (15%; 103–118 mL/min) 4 h after an i.m. injection of 200 mg of the steroid. By extrapolation, they suggested that pregnancy levels of serum progesterone, which are considerably higher, could account for the 40–65% gestational increase of GFR. Of further interest, studies in male subjects in whom renal function was measured either 3 h after i.m. administration of 310 mmol progesterone or 3 days after 155 mmol progesterone i.m. twice daily revealed significant increases in ERPF (~15% and irrespective of dietary sodium intake), but GFR was unchanged. Finally, subcutaneous injection of 2 mg/kg/d progesterone to intact female rats for 3 days produced a 26% increase in GFR; however, ERPF was not measured in this study. Thus, data from both humans and animals suggest a contribution of progesterone (or its metabolites) to the gestational rises in ERPF and GFR, although definitive evidence is lacking.
Prolactin surges in both pseudopregnant and pregnant rats during the first half of gestation coinciding with the increases in ERPF and GFR. Whether prolactin (or later in pregnancy, placental lactogen acting via the same receptor) actually contributes to the increase in renal hemodynamics and GFR during early gestation remains controversial and requires further study.
Relaxin is another hormonal candidate underlying the gestational changes in renal function. In gravid rats and women circulating relaxin arises from the corpus luteum. Human chorionic gonadotropin (hCG) is a major stimulus for relaxin secretion during pregnancy in women.
There was compelling, albeit, circumstantial evidence for considering relaxin a potential mediator of renal vasodilation and hyperfiltration during pregnancy. (i) Circulating relaxin concentrations rapidly increase after conception in women coinciding with the large increases in GFR and ERPF during the first trimester, and refs cited above). (ii) Circulating relaxin is detectable during the luteal phase of the menstrual cycle corresponding with the transient 10–20% increase in GFR and ERPF at that time, and see section Maternal Factors in Early Renal Circulatory Adaptations , above. (iii) The early gestational rise in relaxin coincides with another physiological adaptation in human pregnancy, i.e., changes in osmoregulation. These osmoregulatory changes were recapitulated by administering hCG to women in the luteal phase, but not to men suggesting the intermediary role of an ovarian hormone. Furthermore, administration of synthetic human relaxin to ovariectomized rats for 7 days produced a significant decline in P osm without changing plasma AVP concentration similar to the osmoregulatory changes noted in normal pregnancy. (iv) Chronic administration of relaxin was reported to reduce blood pressure, [ but not confirmed in ] and vasoconstrictor responses in the mesenteric circulation of spontaneously hypertensive rats, while acute administration increased coronary blood flow and reduced platelet aggregation through nitric oxide (NO) and cGMP, thereby implicating a cardiovascular role for the hormone.
Although ERPF and GFR may rise in gravid rats as early as gestational day 5, before circulating relaxin is measurable, there is a jump in renal function between gestational days 8 and 12, when circulating relaxin concentrations surge. (The modest increases in GFR and ERPF that occur during rat gestation before circulating relaxin is detectable on gestational or during pseudopregnancy when circulating relaxin is also undetectable seem to be mediated by other, as yet, undiscovered mechanisms.) Supporting the hypothesis that relaxin mediates the renal circulatory changes of pregnancy, Danielson and colleagues reported that long-term administration of porcine relaxin (pRLX) or of recombinant human relaxin (rhRLX) to chronically instrumented, conscious nonpregnant female rats increased both ERPF and GFR to midgestational levels when renal function peaks in this species. The renal circulatory response to relaxin was not contingent upon the ovaries, and intriguingly, was also noted in male rats. Short-term administration of rhRLX to conscious nonpregnant rats also increased GFR and ERPF within 1–2 h. Moreover, myogenic reactivity of small renal arteries isolated from relaxin-treated rats was significantly reduced and comparable to reductions previously reported in small renal arteries isolated from midterm pregnant rats. This phenomenon of reduced myogenic reactivity of small renal arteries has served as a faithful in vitro bioassay for the renal vasodilatory changes induced by pregnancy or relaxin treatment of nonpregnant rats. Finally, by administering relaxin-neutralizing antibodies or removing circulating relaxin by ovariectomy and maintaining pregnancy with exogenous administration of sex steroids in physiological amounts, the gestational renal hyperfiltration, vasodilation, and reduced myogenic reactivity of small renal arteries isolated from midterm pregnant rats were completely abolished. These experimental manipulations also circumvented the osmoregulatory adaptations of pregnancy. Thus, relaxin is critical to the renal circulatory and osmoregulatory changes of midterm pregnant rats. It may also contribute to these pregnancy adaptations in women.
Endothelium-derived relaxing factors including vasodilatory prostaglandins (PGs) and NO have been hypothesized to mediate the gestational increases of ERPF and GFR. The potential intermediary role of PGs has been investigated in gravid animal models and humans. Gestational rises in ERPF and/or GFR were unaffected by administration of PG synthesis inhibitors to chronically instrumented, conscious gravid rats or rabbits. Moreover, vasodilatory PG synthesis in vitro was not to increased in renal tissues from pregnant animals. Although intravenous PG infusion is not physiologically equivalent to locally produced hormone, intravenous infusion of prostacyclin to male human volunteers did not significantly change either ERPF or GFR. In related studies, the cyclooxygenase inhibitor, indomethacin, raised systemic vascular resistance by only 5% in pregnant women without significantly affecting either mean arterial pressure or cardiac output, and this increase was trivial compared to the overall decrease in systemic vascular resistance of ~40% observed during normal pregnancy. Similarly, another cyclooxygenase inhibitor, meclofenamate, did not significantly augment systemic vascular resistance in conscious, gravid guinea pigs. Taken together, the results do not support a significant role for vasodilatory PGs in the elevation of ERPF, GFR, and cardiac output, as well as the reduction in both renal and systemic vascular resistances during pregnancy.
Guanosine 3’,5’’-cyclic monophosphate (cGMP) and NO: cGMP , a second messenger of NO may participate in the renal vasodilation and hyperfiltration of pregnancy. Because extracellular levels generally reflect intracellular production, plasma levels, urinary excretion, and “metabolic production rate” of cGMP were investigated in conscious rats. All of these variables were increased throughout pregnancy and pseudopregnancy. Comparable elevations in urinary excretion and plasma concentration of cGMP were reported for human gestation. The 24-h urinary excretion of nitrate and nitrite (NO x ), the stable metabolites of NO, also increased during pregnancy and pseudopregnancy in rats consuming a low-NO x diet, paralleling the rise in urinary cGMP excretion. This gestational rise in urinary NO x excretion was prevented by chronic administration of nitro- l -arginine methyl ester ( l -NAME), an inhibitor of NO synthase, implicating NO as the source. Plasma concentrations of NO x were also higher in pregnancy, and NO-hemoglobin was detected only in the red blood cells from pregnant, but not from nonpregnant, rats by electron paramagnetic resonance spectroscopy. These results demonstrated that endogenous NO production is increased in gravid rats. Although the tissue source(s) of the gestational increase in NO production was not identified, the possibility that vascular tissues contributed was raised. Plasma levels and urinary excretion of NO x were also reported to be increased in gravid ewes. Unfortunately, the situation of NO biosynthesis during normal human pregnancy (and in women with preeclampsia) remains controversial.
The renal circulation contributes to the overall maternal vasodilatory response of pregnancy. Renal vascular resistance reaches a nadir, and ERPF and GFR peak during midgestation in rats. In chronically instrumented conscious, midterm pregnant and virgin control rats acutely administered l -arginine analogs, which inhibit NO synthase, GFR, ERPF, and effective renal vascular resistance converged in the two groups of animals. In other words, compared to virgin control rats, the gravid animals responded more robustly to short-term infusion of NO synthase inhibitors, resulting in a larger decline in GFR and ERPF, and a greater rise in effective renal vascular resistance. Consistent with these in vivo data was the inhibition of myogenic reactivity in small renal arteries ex vivo isolated from midterm pregnant compared to virgin control rats, which was restored to virgin levels by addition of NO synthase inhibitors to the bath or endothelial removal.
A critical role for NO in renal vasodilation, hyperfiltration, and reduced myogenic reactivity of small renal arteries was also established for relaxin-treated nonpregnant rats again by using l -arginine analogs. Thus, NO serves a critical role in the renal circulatory changes of both pregnant and relaxin-treated nonpregnant rats. Although pregnancy and relaxin administration to nonpregnant rats, both elicit renal vasodilation, hyperfiltration and reduced myogenic reactivity of small renal arteries that is dependent upon NO ( vide supra ), unexpectedly the urinary excretion of cGMP and NO metabolites is only increased during pregnancy. Ironically, therefore, the increased production of cGMP and NO metabolites described initially in rat pregnancy, and which stimulated further interrogation of this vasodilatory pathway, may not be either of vascular origin or of hemodynamic consequence.
Of additional interest is that in one report, but not in another, vasodilatory PGs fulfilled a compensatory role maintaining relative renal hyperfiltration and vasodilation in gravid rats compared to virgin controls during chronic NO synthase blockade. In other words, in the setting of chronic NO synthase inhibition, renal function converged in the two groups of rats after short-term infusion of PG synthesis with meclofenamate. PG blockade alone, however, did not affect renal function in conscious virgin or pregnant rats.
Paradoxically, endothelin (ET) plays a critical role in the renal vasodilation and hyperfiltration of pregnant and relaxin-treated nonpregnant rats. ET is widely recognized as a potent vasoconstrictor through interactions with ET A and ET B receptor subtypes on vascular smooth muscle. However, ET also increases intracellular calcium in endothelial cells, thereby stimulating synthesis of prostacyclin, NO, and possibly other relaxing factors through an endothelial ET B receptor subtype. Specific blockade of the ET B receptor subtype in chronically instrumented, conscious male rats with the pharmacologic antagonist, RES-701-1, induced profound renal vasoconstriction. This unexpected finding indicates a major contribution of endogenous ET in maintaining low renal vascular tone through a RES-701-1 sensitive, endothelial ET B receptor subtype and tonic stimulation of endothelium-derived relaxing factors and/or restraint of ET production. RES-701-1 appears to be relatively selective for the “vasodilator” ET B receptor subtype on the endothelium. In summary, the RES-701-1 sensitive, endothelial ET B receptor subtype maintains low renal vascular tone in normal conscious rats most likely through tonic stimulation of NO. However, with ET infusion or in pathophysiological states, ET-mediated vasoconstriction may predominate in the kidney.
A logical extension of these observations in nonpregnant rats is that the endothelial ET B receptor–NO vasodilatory mechanism is accentuated during pregnancy, thus mediating gestational renal vasodilation and hyperfiltration. Indeed, short-term infusion of RES-701-1 to conscious virgin and gravid rats completely abrogated gestational renal vasodilation and hyperfiltration, thereby producing a convergence of GFR, ERPF, and effective renal vascular resistance in the two groups of animals. As well, the inhibited myogenic reactivity of small renal arteries ex vivo isolated from gravid rats was reversed by addition of RES-701-1 or of a mixed ET B +ET A antagonist (SB209670), but not a specific ET A receptor antagonist (BQ123) to the bath. These observations were analogous to those using inhibitors of NO synthase ( vide supra ). Subsequently, the NO/cGMP pathway was suggested to transduce the vasodilatory action of endogenous ET in the renal circulation of pregnant rats.
The essential role of the endothelial ET B receptor subtype in mediating inhibited myogenic reactivity of small renal arteries isolated from pregnant rats was corroborated in the ET B receptor-deficient rat. Finally, a critical role for the endothelial ET B receptor subtype in mediating renal vasodilation, hyperfiltration, and reduced myogenic reactivity of small renal arteries was also established for relaxin-treated nonpregnant rats.
Jeyabalan and coworkers proposed that relaxin enhances vascular gelatinase activity during pregnancy that, in turn, mediates renal vasodilation, hyperfiltration, and reduced myogenic reactivity of small renal arteries ultimately through activation of the endothelial ET B receptor–NO pathway ( Figure 81.6 ). The hypothesis that vascular gelatinase activity plays a pivotal role was founded upon the confluence of several observations: first, the essential role of relaxin, the endothelial ET B receptor, and NO in pregnancy-mediated renal vasodilation as described above; second, the publications reporting stimulation of matrix metalloproteinase (MMP) expression by relaxin in fibroblasts; and third, the ability of vascular MMPs, such as MMP-2, to hydrolyze big ET at the gly–leu bond to yield ET 1–32 with activation of ET receptors.
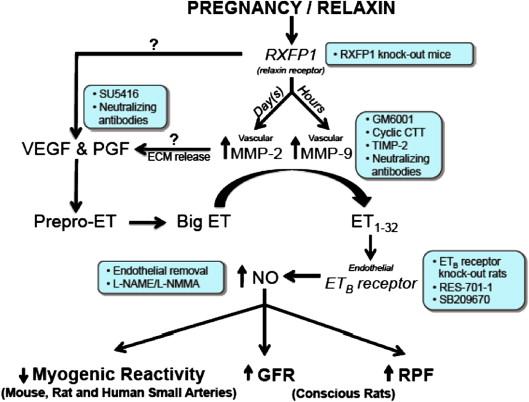
The best (if not the only) approach to testing the potential role of MMP-2 in mediating renal vasodilation, hyperfiltration, and inhibited myogenic reactivity of small renal arteries mediated by pregnancy or relaxin is to block MMP-2 production or its activity. Accordingly, short-term infusion of gelatinase inhibitors abrogated relaxin-mediated renal vasodilation and hyperfiltration in conscious rats; moreover, the inhibited myogenic reactivity of small renal arteries isolated from pregnant or relaxin-treated nonpregnant rats was reversed by gelatinase inhibitors in vitro . In contrast, there was no effect of the traditional ET-converting enzyme inhibitor, phosphoramidon, which inhibits the processing of big ET to ET 1–21 . In small renal arteries harvested from relaxin-treated nonpregnant and midterm pregnant rats, MMP-2 activity is increased by ~50% relative to nonpregnant control arteries. Thus, vascular gelatinase activity is not only part of the relaxin-endothelial ET B receptor–NO vasodilatory pathway, but it is a major locus of regulation by relaxin in this species, because neither endothelial NO synthase nor ET B receptor abundance is increased by relaxin or pregnancy, but not all investigators agree.
It is unlikely that vascular MMP-2 and endothelial ET B receptor–NO are components of separate vasodilatory pathways acting in parallel. If this was the case, then one might predict that after inhibition of either vascular MMP-2 or the endothelial ET B –NO pathway, compensation of one for the other should be observed. However, no compensation or even partial compensation was noted: each and every inhibitor of the ET B receptor, NO synthase, or MMP completely abolished the renal circulatory changes during pregnancy or relaxin treatment of nonpregnant rats. Nevertheless, experimental confirmation of a common vasodilatory pathway shared by vascular gelatinase activity and the endothelial ET B receptor–NO vasodilatory pathway was obtained. That is, small renal arteries isolated from relaxin-treated, ET B receptor-deficient rats showed upregulation of vascular MMP-2 activity, but failed to show inhibition of myogenic reactivity. This dissociation of the biochemical and functional consequences of relaxin administration in small renal arteries harvested from ET B receptor-deficient rats, when taken in the context of the other results ( vide supra ), strongly suggests that vascular gelatinase is in series with, and upstream of, the endothelial ET B receptor–NO signaling pathway.
To summarize, during pregnancy relaxin accentuates the endothelial ET B receptor–NO renal vasodilatory pathway by increasing vascular MMP-2 activity (via increases in MMP-2 mRNA and protein ). A more recent study also suggests the participation of vascular endothelial growth factor (VEGF) and placental growth factors (PlGF) in the renal vasodilatory pathway of relaxin. Interestingly, higher doses of gelatinase inhibitors also decreased GFR and ERPF, and elevated arterial pressure when administered to control rats, albeit less so than in relaxin-treated rats, whereas phosphoramidon was again without effect. These results suggest that vascular gelatinase activity rather than the traditional ET-converting enzyme may be the main physiological mechanism for big ET processing (and consequent vasodilation) at least in the renal circulation of rats. Possibly, the colocalization of MMP-2 and associated proteins in the caveolae of endothelial cells with the ET B receptor and eNOS facilitates this interaction ( Figure 81.6 ).
Other factors in addition to relaxin are likely to contribute to gestational renal vasodilation and hyperfiltration especially during late pregnancy, when circulating levels of placental hormones are particularly high. For example, placental growth hormone may contribute. In addition, local factors within the kidneys themselves may participate. Mesangial cell expression of iNOS, the angiotensin (AT)-2, and relaxin receptors was reported to increase during midgestation in rats. Moreover, upregulation of the n NOSβ isoform in the renal cortex of midterm pregnancy rats was noted. Intriguingly, Morgan and colleagues observed increased histidine decarboxylase and histamine production in the superficial cortical zone of pregnant mice. Finally, increased renal production of epoxyeicosatrienoic acid may also play a role in renal vasodilation and hyperfiltration of pregnancy.
To conclude, evidence from both animal and human studies suggests that renal hyperfiltration in pregnancy is secondary to increased RPF, the latter resulting from profound decreases in renal vascular resistance. There has been considerable progress in identifying mechanisms responsible for gestational renal vasodilation, and those most promising so far were reviewed in detail above. Of importance, whatever the primary vasodilatory stimulus, it must be a powerful one, for the pregnancy-induced rise in GFR is not restricted to women with two normally functioning kidneys but occurs also in subjects with previously hypertrophied single kidneys (following uninephrectomy) and in transplant recipients.
The GFR increase during pregnancy has important clinical consequences. Production of creatinine changes little, so that increases in creatinine clearance lead to a reduction in its plasma level. This is also true of urea, which may be decreased even further by enhanced protein synthesis. Therefore, levels of creatinine and urea nitrogen decrease from a mean of 0.7 and 12 mg/dl (62 and 4.3 mmol/L), respectively, in the nonpregnant state, to 0.5 and 9 mg/dL (44 and 3.2 mmol/L). The implication of these observations is that values considered normal in nonpregnant women may reflect compromised renal function during pregnancy. Concentrations of serum creatinine and urea nitrogen exceeding 0.8 and 13 mg/dL (80 mmol/L and 5 mmol/L), respectively, should alert the clinician to evaluate renal function further.
The augmented filtered load consequent to increased GFR also contributes to the glucosuria, aminoaciduria, and enhanced urinary excretion of water-soluble vitamins that occur during normal pregnancy. Urinary protein excretion may double as well, but the greatest increments seem to occur in late gestation, long after changes in renal hemodynamics are maximal. Also, there are still discrepancies about whether there are increases in albuminuria during pregnancy, but the majority of studies suggest so. It should be borne in mind, though, that many factors affect urinary protein excretion in addition to glomerular filtration, including the pore size and number of fixed charges in the glomerular filtration barrier, and tubular reabsorption rates, a topic discussed elsewhere in this text.
There are also changes, usually increments, in the renal excretion of various low-molecular weight proteins and enzymes during pregnancy. Whether the alterations result from increased filtration and/or changes in tubular handling, or even in production is unclear (see Ref. ) for further details and citations). The increments in urinary glucose, amino acids, and proteins mentioned above also have pathophysiological consequences, i.e., the nutrient content of the urine is increased, which may predispose pregnant women to symptomatic urinary tract infection. Finally, awareness that the normal limit of urinary protein excretion is increased during gestation to 300 mg/24 h suggests that this event will also occur and may even be exaggerated in women with preexisting kidney disorders, so that increased proteinuria during pregnancy does not necessarily signify progression or exacerbation of their disease.
Glucosuria may occur normally during pregnancy. In one study, 30 women with normal glucose tolerance were evaluated serially beginning early in gestation and continuing through the sixth postpartum week (reviewed in Ref. ). Daily urinary excretion of glucose was measured by a sensitive and specific enzymatic assay, an important methodological consideration, because excretion of many other reducing substances also increases during pregnancy. All subjects excreted <100 mg/24 h when not pregnant, but during gestation this value was exceeded in 26 women (86%) ranging up to 500 mg in 12, between 0.5 and 1.0 g in 4, and exceeding 1 g/24 h in 10 others. Glucosuria was intermittent and not necessarily related to blood glucose levels or gestational stage. A comparable high incidence of glucosuria in normal pregnancy was reported by others (reviewed in Ref. ). Gestational glucosuria reverts to normal within 1 week postpartum.
Renal tubular handling of glucose, including the transport maximum ( T m ), threshold, and splay of the titration curve were evaluated during pregnancy. Many reports had weaknesses in experimental design, but there were exceptions. With exquisite attention to methodology, Welsh and Sims assessed the T m of glucose in normal nonpregnant subjects, nonglycosuric pregnant women, and normoglycemic glycosuric gravidas. The T m of glucose was lower in the latter group in comparison to the nonglycosuric pregnant subjects, and the authors proposed that gestational glucosuria resulted from increased GFR, and hence filtered load, in women with a low T m for glucose. Fifteen years later, Davison and colleagues suggested that both the T m and fractional reabsorption of glucose decrease in all pregnant women. In their study, renal glucose reabsorption was measured in subjects with normal carbohydrate metabolism during and after gestation. Care was taken to avoid extremely high plasma glucose concentrations during infusions, which can affect renal hemodynamics. All women demonstrated lower fractional reabsorption of glucose during pregnancy compared to after delivery. Those most severely glycosuric in pregnancy had the lowest fractional reabsorption rates both during and after gestation; however, they were not glycosuric postpartum because GFR and the filtered load of glucose had decreased substantially. Said otherwise, even if the splay in the glucose titration curve increases or the glucose T m decreases slightly, the striking gestational increment in GFR and consequent filtered load of glucose remains the major cause of glucosuria in pregnancy.
Gravid rats may also display glucosuria. Renal micropuncture studies in this species reveal that proximal tubular glucose reabsorption is actually enhanced, commensurate with the increment in filtered load; thus, the increased urinary glucose is due mainly to decreased distal tubular reabsorption, and perhaps to changes in epithelial permeability causing backleak in Henle’s loop.
Excretion of other sugars, including lactose, fructose, xylose, and fucose, but not arabinose, also increases during pregnancy [citations in Ref. ]; lactosuria is present in 50% of gravidas by the end of gestation, when excretion may be as much as 10-fold higher than nongravid women. During pregnancy, certain oligosaccharides are excreted in the urine not found in the urine of nonpregnant women, and thus, they are suspected to be of mammary origin. It should be emphasized, however, that the excretion of these sugars combined is minimal compared to that of glucose, and consequently, they do not amount to a significant nutrient loss to the mother.
The renal excretion of several water-soluble vitamins is also increased during pregnancy including nicotinic, ascorbic, and folic acids. Plasma folate levels actually decrease in pregnancy, and the increased urinary excretion may be largely due to reduced tubular reabsorption rather than enhanced filtered load.
Urinary excretion of many amino acids rises during pregnancy. In fact, urinary histidine concentration was once used as a method to detect pregnancy, and its disappearance from the urine was noted in preeclampsia. The most detailed studies are by Hytten and Cheyne, who conducted serial measurements in 10 women from early pregnancy through the eighth postpartum week. Renal excretion of glycine, histidine, threonine, serine, and alanine increased early in gestation and urinary losses became substantial near term. In contrast, increments in urinary excretion of lysine, cystine, taurine, tyrosine, phenylalanine, valine, and leucine occurred during the first half of pregnancy, but declined thereafter, and the urinary excretion of asparagine, glutamic acid, and arginine was unchanged during gestation. It is noteworthy that gestational aminoaciduria can reach ~2 g/day, a loss that could adversely affect fetal growth, if protein intake is suboptimal. In some subjects, urinary glycine and histidine excretion exceeded 50% of the filtered load, suggesting a role for inhibition of tubular reabsorptive process. However, these data reflect 24-h renal clearance measurements, and the little information concerning threshold or T m during short-term infusion studies is inconclusive.
Although uric acid production has been described as unchanged during pregnancy, more recent evidence disputes this conclusion. In either case, gravidas excrete considerably more urate than when they are not pregnant. The renal clearance of uric acid, typically 6–12 mL/min in nonpregnant women, rises to 12–20 mL/min during pregnancy, and consequently, plasma concentrations decline at least 25% and are only 2.5–4.0 mg/dL in many pregnant women. In most centers, 5–5.5 mg/dL is considered to be the normal upper limits for pregnancy, but the upper limit is different depending on the stage of gestation. Circulating urate tends to be higher in women with multiple gestations, displays circadian rhythm with higher and lower levels at morning and night, respectively, and the normal range may be subject to racial variations.
Whereas both the filtered load and absolute tubular reabsorption of urate increase during gestation, most investigators have documented increments in fractional excretion, i.e., the C urate / C inulin ratio is greater in pregnancy than in the nonpregnant state (reviewed in Refs and ). However, there have been only two well-monitored serial studies in which investigators determined urate concentrations with specific enzymatic assays, and the results vary. In one study, no difference in fractional clearance of urate during and after pregnancy was reported, whereas in the other, C urate / C inulin increased during the first two trimesters but returned to nonpregnant values in the third.
The peak in renal clearance of urate and the nadir in plasma concentration are observed in early gestation; subsequently, C urate declines and plasma urate levels rise near term. It is not clear whether these findings are confounded by postural artifacts, nonrenal metabolic effects in relation to the oxidant/antioxidant balance during gestation, or possibly by inadvertent inclusion of women with subclinical preeclampsia. In this regard, decrements in the C urate / C inulin or increments in P urate concentrations may precede the clinical manifestations of preeclampsia.
There are few data on body potassium stores in pregnancy. One study suggests that body stores decline early in gestation and then rise to values ~100 mEq above prepregnancy levels. These findings are consistent with the theoretical considerations that pregnant women should lose potassium in their urine, because they eat and excrete normal quantities of sodium, but manifest very high levels of aldosterone and other potent mineralocorticoids (see below). Furthermore, they develop bicarbonaturia at substantially lower plasma bicarbonate levels than do nonpregnant women. Observations that plasma and serum potassium levels decrease 0.2–0.3 mEq/L between gestational weeks 10 and 28 are also consistent with this formulation.
A more traditional view, however, is that pregnant women do not waste potassium but undergo a cumulative retention of ~350 mEq of the cation, most of which is stored in the products of conception, as well as in the organs of reproduction ( Table 81.1 ). Moreover, in striking contrast to nonpregnant women, gravidas are resistant to the kaliuresis provoked by the combination of exogenous mineralocorticoids and a high-sodium diet ( Figure 81.7 ). This remarkable capacity to conserve potassium in the face of high concentrations of potent mineralocorticoids such as aldosterone and deoxycorticosterone (DOC), and the delivery of substantial quantities of sodium to distal nephron sites, may be secondary to the increased circulating levels of progesterone during pregnancy, a view supported by studies in both humans and animals but not accepted by all.
| Storage site | Sodium, mEq | Potassium, mEq | Calcium, g |
|---|---|---|---|
| Fetus | 290 | 154 | 28.00 |
| Placenta | 57 | 42 | 0.65 |
| Amniotic fluid | 100 | 3 | Negligible |
| Uterus | 80 | 50 | 0.22 |
| Breasts | 35 | 35 | 0.06 |
| Plasma | 140 | 4 | 0.12 |
| Red cells | 5 | 24 | 0.38 |
| Interstitial fluid | 240 | 8 | 0.25 |
| Total | 947 | 320 | 29.68 |
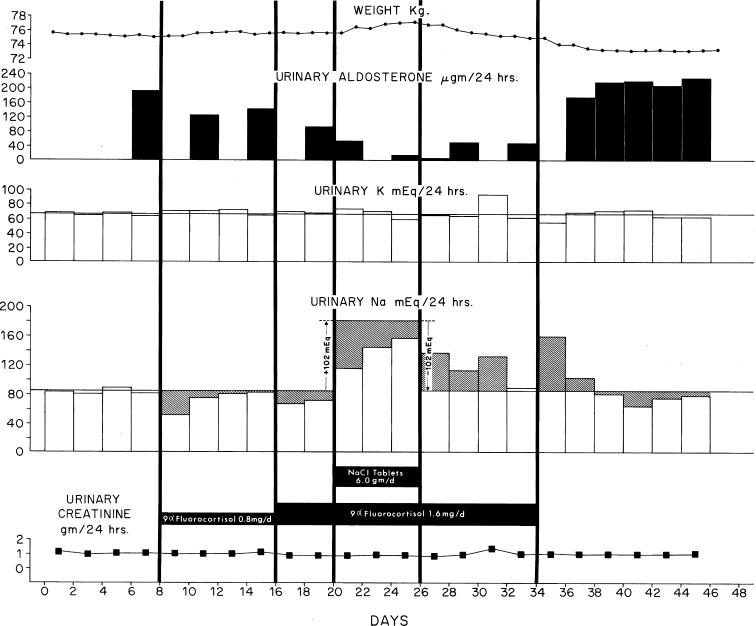
Resistance to the kaliuretic influence of mineralocorticoids may benefit gravid women with certain potassium-wasting diseases. On the one hand, excessive potassium loss of primary aldosteronism may be easier to control in gestation ( Figure 81.8 ). On the other, if the kidneys resist kaliuretic stimuli, women with underlying disorders that impair their ability to excrete potassium may be jeopardized by gestation. Finally, there is a rare disorder in which the renal mineralocorticoid receptor is genetically altered in a manner that hormones antagonizing the salt-retaining actions of corticoids become agonist in nature. During pregnancy, progesterone levels increase 100-fold, and women heterozygous for the disorder manifest severe hypertension, renal potassium wasting, and marked hypokalemia, but suppressed aldosterone levels.

Acid–base balance is affected by pregnancy. Blood levels of hydrogen ion decline 2–4 nmol early in gestation, a decrement that is maintained throughout pregnancy, and arterial (or arterialized capillary) blood pH is typically 7.42–7.44 in gravidas, as compared with 7.38–7.40 in nonpregnant women. This mild alkalemia is respiratory in origin, because pregnant women hyperventilate (believed to be a central effect of progesterone effect), and consequently, their arterial PCO 2 decreases from a nonpregnant mean of 39 to 31 torr during gestation. Supporting the causal role of progesterone are data showing that arterial PCO 2 also falls 3–4 torr during the luteal phase of the menstrual cycle. These decrements in PCO 2 are compensated by decreases in plasma bicarbonate levels of ~4 mEq/L, normal values in gestation ranging from 18 to 22 mEq/L, thereby establishing a blood pH that is only slightly alkalotic.
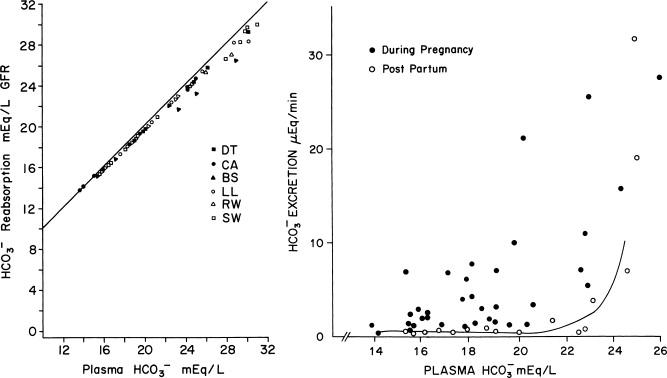
There have been few studies addressing renal bicarbonate reclamation and regeneration during pregnancy. Lim et al. infused a hypertonic bicarbonate solution in women during the third trimester. The bicarbonate titration curve from that study is shown in Figure 81.9 (left). Despite large filtered loads of bicarbonate, reabsorption continued to increase, and even when plasma levels reached 31 mEq/L, reabsorption virtually matched the filtered load. These results were unexpected, because pregnant women are hypocapnic and have increased extracellular volumes, conditions that should lead to an exaggerated “splay” in the titration curve and/or a decrease in the apparent T m for bicarbonate. However, a small but persistent bicarbonate leak was noted at lower plasma bicarbonate concentrations during pregnancy than postpartum ( Figure 81.9 , right). This modest bicarbonaturia was occasionally present at plasma bicarbonate levels as low as 15–16 mEq/L.
Urinary acidification as well as titratable acid and ammonium excretion have been measured in gravid women after being challenged with both acute and chronic administration of NH 4 Cl. The results were comparable to those of nonpregnant control subjects. It is noteworthy that the decrement in urine pH and the increases in titratable acid and ammonium excretion occurred even though blood pH decreased only slightly from 7.44 to 7.40. Thus, substantial bicarbonate regeneration can already be demonstrated at a pH higher than in nonpregnant women, and in fact it starts when values are still alkaline relative to the nonpregnant state. Distal hydrogen secretory capacity, as measured by the increment in urinary PCO 2 during the bicarbonaturia that accompanied the hypertonic bicarbonate loading, appeared to be intact during pregnancy. Finally, the decrease in blood pH during exercise is similar in the pregnant and nonpregnant states.
P osm decreases 8–10 mOsm/kg during normal gestation. This decline, which starts in the luteal phase of the menstrual cycle, continues through conception and reaches a nadir about gestational week 10, after which it is maintained until term. Only about 1.5 mOsm/kg of the fall can be accounted for by decreases in urea concentration, most of the change resulting from a decline in the concentrations of plasma sodium and its attendant anions. Thus, pregnancy is characterized by a true decrease in effective P osm .
A decrease in P osm of such magnitude in a nonpregnant subject would suppress antidiuretic hormone secretion and result in a state of massive and continuous water diuresis, which does not happen in pregnant women. Rather, gravidas are able to maintain the new, lower P osm within a narrow range, and water loading or fluid restriction, respectively, lead to appropriate dilution and concentration of their urine. These events are made possible because osmotic thresholds for both AVP secretion and thirst decrease by 8–10 mOsm/kg each during gestation, decrements which are already demonstrable during gestational weeks 5–8 and are sustained through term ( Figure 81.10 ). It should be emphasized that parallel declines in both the osmotic thresholds for AVP release and thirst are required, in order to maintain the new steady state P osm within a narrow range. That is, P osm would rise in the face of persisting circulating levels of AVP at the lower P osm of gestation, if the subject is not simultaneously stimulated to drink water; conversely, considerable polydipsia would be required to maintain a lower P osm in the absence of AVP secretion.
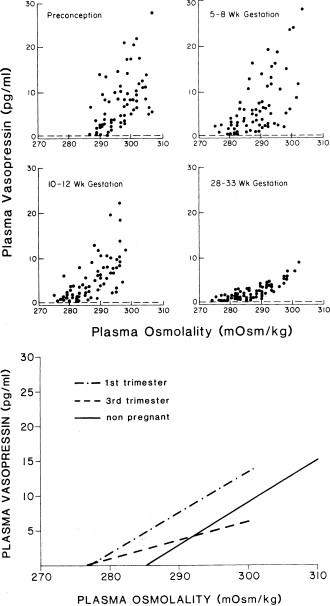
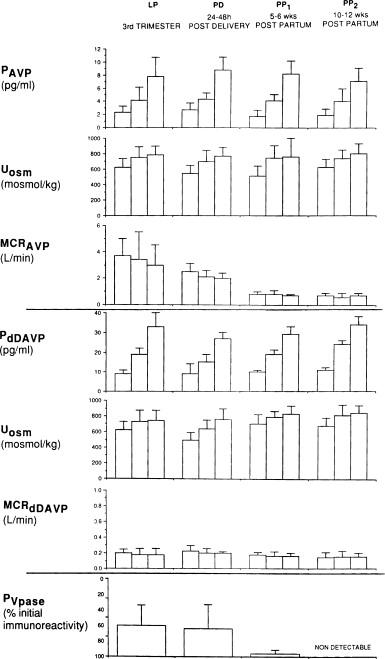
The metabolism of AVP also changes in gestation, hormonal disposal rates rising four-fold between early and midgestation. This rather striking increase in the metabolic clearance rate (MCR) of AVP parallels the marked increase in both placental trophoblastic mass and circulating levels of cystine aminopeptidase (vasopressinase). Thus, the rise in MCR of AVP is likely due to the extremely high circulating vasopressinase emanating from the placenta, a concept supported by studies showing that the metabolic clearance of 1-deamino 8-D-AVP (DDAVP, Desmopressin), the AVP analogue resistant to inactivation by vasopressinase, does not change in pregnancy ( Figure 81.11 ).
The cause of the osmoregulatory changes in pregnancy is obscure. hCG, constitutive NOS, and relaxin have each been suggested to play etiologic roles. Of further interest, decrements in P osm do not occur in every species ; they do so, however in rodents (along with decreases in the osmotic thresholds for AVP release and drinking), and the rat has become the model in which to explore mechanisms responsible for changes that occur in humans. In this latter model, injection of hCG yielded equivocal results (Barron and Lindheimer, unpublished observations), but relaxin lowers P osm , as well as the osmotic threshold for AVP release. These data suggest that the osmoregulatory effects of hCG in premenopausal women, ineffective in males, is through stimulation of ovarian relaxin secretion. This hypothesis remains to be explored.
Of interest is a group of investigators that ascribed the decreased P osm in pregnancy to the decreased “effective” circulating volume of pregnancy (so-called “nonosmotic” release mechanism, see below). Ohara et al. suggested that plasma AVP is detectable at low P osm during pregnancy due to nonosmotic release, and gravid rats also manifest upregulation of aquaporin-2 (AQ2) mRNA and protein in apical membranes of the collecting duct, thus abetting water retention and lower body tonicity. However, the mechanism underlying increased AQ2 expression is uncertain, because circulating AVP, although detectable despite the lower P osm , are not elevated above nonpregnant values (as in congestive heart failure). As discussed below, others have accumulated evidence against decreased or “underfill” of the arterial circulation as an explanation for the control of vasopressin secretion during pregnancy. We note here that the observations of Ohara et al may be paradoxical, insofar as an increase in AQ2 might be expected to blunt the animals ability to excrete a water load, yet gravid rats excrete water as well as or better than virgin controls.
The physiological significance of the changes in body tonicity, as well as in the osmotic threshold for AVP release and thirst is unclear. They may represent an epiphenomenon secondary to hormonal changes of pregnancy, but it is noteworthy that they may facilitate the increments in intravascular and extracellular volume that occur in pregnancy. Some believe the “physiological hypervolemia” of gestation optimizes fetal development, and in this respect, hypoosmolality results in a need for less solute per liter of extracellular water retained, certainly an advantage when sodium is scarce. Another idea is that the retention of water during pregnancy, which is distributed mainly to the intracellular space, creates a reservoir for maintaining extracellular and intravascular volume when water is scarce.
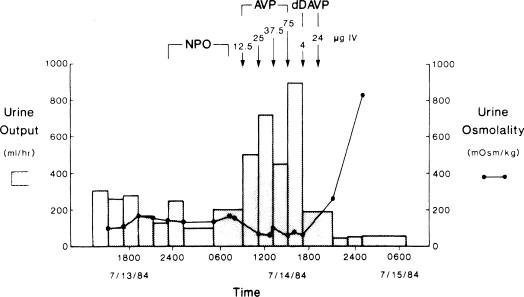
One very clinically relevant consequence of the altered osmoregulation in pregnancy is related to the striking increase in the MCR of AVP. In the past, women with central diabetes insipidus (DI) required increasing amounts of AVP administration during pregnancy. This is no longer the case since virtually all patients are currently managed with DDAVP, which escapes metabolism by circulating placental vasopressinase ( vide supra ). Still there are patients with partial central DI and sufficient hormone secretory capacity to escape detection when nonpregnant, whose disease is unmasked by the marked increase in AVP disposal rates of pregnancy. More frequent and dramatic, however, is another syndrome called “transient DI of pregnancy,” which presents during the second half of gestation and remits postpartum. It is important to recognize this entity as women may become dangerously hypernatremic especially if they undergo cesarean sections using general anesthesia or are water restricted in the delivery suite. These patients have markedly high levels of circulating vasopressinase that may still be above those of normal gestation when measured during the first week of the puerperium. Others may have subclinical central DI, their pituitary gland unable to respond to the increases in MCR of AVP during pregnancy. Polyuria in these women is usually unresponsive to large doses of AVP (pitressin), but they concentrate their urine rapidly when treated with DDAVP ( Figure 81.12 ). Some of these patients have hepatic dysfunction usually associated with preeclampsia, but in a few the DI has been associated with acute fatty liver of pregnancy. Thus, it is tempting to speculate that failure of the liver to inactivate vasopressinase, coupled with continuous placental production of large quantities of the enzyme, are causal. Consistent with this reasoning is documentation in one patient of excessive pitocin requirements during labor (vasopressinase destroys oxytocin as well as AVP).
The ability to excrete water during pregnancy can be altered in other ways as well. Changing from lateral recumbency to a supine position decreases urine flow, and quiet standing may be more antidiuretic in pregnant than nonpregnant subjects (reviewed in Refs ). The effect of supine posture is independent of circulating levels of antidiuretic hormone, since it has been noted in a pregnant patient with central DI. It should be underscored, however, that these “nonosmotic” influences on water handling are not sufficient, of themselves, to explain the gestational decline in P osm . No single body position is maintained all day, and in addition the posturally induced antidiuresis rarely retards urine flow sufficiently to account for the chronically reduced P osm (and thus the decreased plasma sodium levels ) observed in pregnancy.
The relative contribution of nonosmotic factors to the regulation of AVP secretion during pregnancy is uncertain, but in the nonpregnant human, volume is an important determinant of AVP release: hypovolemia stimulates, whereas hypervolemia blunts hormone secretion. In gestation, absolute blood volume increases markedly, but how the “effective volume” is sensed is a subject of considerable speculation, ( and discussed below). In this respect, the pregnant rat, which also undergoes a 40–50% increase in plasma volume near term, resets its volume-sensing, vasopressin secretory mechanisms such that the increased volume is sensed as normal. Hypovolemia may decrease the osmotic thresholds for hormone release and thirst (see the chapters by Robertson, MacKnight et al., and Fitzsimons, Vol. 2), and some have ascribed the osmoregulatory changes in human pregnancy to an “underfilling” of the dilated intravascular space, ( and see below). However, expansion of the central volume by head-out water immersion during the first or last trimester had no effect on either the reduced tonicity or the decreased osmotic thresholds in pregnant women, and P osm could not be restored by overexpansion of volume (produced by administration of exogenous mineralocorticoids) maintained throughout gestation in rats.
Studies of maximum urinary concentrating capacity ( U max ) during gestation are reviewed elsewhere [see also Table 81.2 of the first edition of this text, which summarizes data from 255 women in seven publications]. However, there are only three reports that include nonpregnant controls whose mean U max is sufficiently high for valid comparisons. Urine osmolality was lower in the pregnant women in each of these studies, but not significantly so (probably due to the limited number of subjects). In any case, the differences from nonpregnant controls were too small to be of biological significance.
| Increase in Weight, g | ||||
|---|---|---|---|---|
| Tissues and Fluids Accounted for | 10 weeks | 20 weeks | 30 weeks | 40 weeks |
| Fetus | 5 | 300 | 1500 | 3400 |
| Placenta | 20 | 170 | 430 | 650 |
| Amniotic fluid | 30 | 350 | 750 | 800 |
| Uterus | 140 | 320 | 600 | 970 |
| Mammary gland | 45 | 180 | 360 | 405 |
| Blood | 100 | 600 | 1300 | 1250 |
| Extracellular extravascular fluid | 0 | 30 | 80 | 1680 |
| Total | 340 | 1950 | 5020 | 9155 |
| Total weight gained | 650 | 4000 | 8500 | 12500 |
| Weight not accounted for | 310 | 2050 | 3480 | 3345 |
Urinary dilution, too, seems unchanged or only minimally affected by gestation. Pregnant women excrete water loads as well as when not pregnant, and gravid rats seem to excrete water more efficiently than virgin controls. The latter observation is of special interest because of the apparent paradoxical observation that AQ2 mRNA and protein are upregulated in the gravid rat. Immunohistochemistry of medullary tissue suggested that the increase in protein was mainly in apical membranes, which should have blunted the animal’s ability to excrete water (as would have small undetectable increases in P AVP , which the authors postulated as causing the upregulation). However, this apparent paradox may be resolved, if during the imposition of water loading, the mechanism(s) responsible for the basal increase in AQ2 expression during pregnancy are superseded.
When investigating urinary diluting capacity in humans, one should be aware that supine posture can interfere with this test. Therefore, studies aimed at detecting minimal urine osmolality or maximum free water clearance should be performed with the patient lying on her side. However, while lateral recumbency is the preferred position for prenatal measurement of most renal functional parameters, this posture interferes with tests of U max . For example, Davison et al. demonstrated that U osm actually decreased in patients dehydrated for 12 h when they assumed a lateral decubitus position for an additional 3 h, but increased when the test was repeated with the subjects sitting quietly. These observations may be explained by fluid mobilization from the extremities during bed rest, which results in either volume suppression of antidiuretic hormone release or in a mild osmotic diuresis. These results demonstrate the importance of upright posture, such as quiet sitting, when tests of maximum urine concentrating ability are performed during pregnancy.
Factors controlling volume homeostasis in pregnancy are incompletely understood and controversial. At one time, authorities believed that pregnant women retained salt excessively, thus predisposing them to develop hypertension. Sodium intake was curtailed and at times diuretics were prescribed prophylactically. More recently, the gravida was considered a subtle sodium waster, and supplemental salt was even advocated as a means of avoiding preeclampsia (reviewed in Refs. A third view, to which we subscribe, is that renal sodium handling is similar in pregnant and nonpregnant women. This section summarizes current views on sodium handling and volume homeostasis in normal pregnancy.
Healthy primigravidas gain ~12 kg during gestation, whereas multiparous women gain about 1 kg less. Most of this gain (~9.5 kg) occurs after the 20th gestational week. Not all of the increase can be accounted for by the products of conception, reproductive tissues, or total body water (discussed below), but 4–6 kg of the added weight may be accounted for by increments in maternal fat stores. The gain of 12 kg cited above was recorded in pregnant women without any edema or with only leg swelling. However, 15% of normal pregnant women may develop generalized edema (including swelling of fingers and face). Their weight gain averaged 14.5 kg, of which 4.9 kg was due to increase in the extracellular-extravascular compartments.
The value of 12 kg is well above averages reported in the older literature. Most surprising, however, is that in the past practitioners tended to regard published averages as upper limits of permissible weight gain, and many pregnant women have been admonished for excessive weight gain and their salt or calorie intake, or both, needlessly restricted. It should be emphasized that some women gain little weight while others may gain twice the average, and gestation proceeds uneventfully in both.
Most of the weight added in pregnancy represents fluid retention. Total body water has been measured during pregnancy using deuterium, the stable isotope of oxygen [O 18 ], and by bioelectrical impedance. The results suggest total accumulations of 6–9 L, although they vary due to methodological differences. Of interest, in a serial study starting before conception, Forsum et al. noted higher increments in body fat than other investigators.
The volume of water accumulated in the extracellular compartment remains uncertain due largely to the lack of an ideal tracer for use in pregnant women. Reported estimates vary widely, and there is poor correspondence in those subjects in whom both extracellular and total body water were measured simultaneously. Reports in which thiocyanate was used as the tracer and the gain in extracellular space calculated as 6–7 L appear the most reasonable, since when added to the estimated 1.8–2.5 L of accrued intracellular water, the total approximates that measured directly with deuterium oxide. Nonetheless, more research in this area will be needed before definitive conclusions can be reached.
Intravascular volume increases during pregnancy due mainly to increases in plasma water and a small increment in red blood cell mass ( Table 81.2 ). Plasma volume has been measured in pregnant women by several methods, but usually with Evans blue dye. In the earlier literature, values were recorded as increasing until gestational week 30 and then declining. Such studies were in error, because late in gestation the indicator may not attain complete mixing within 10 min, if the subject is positioned in a supine or sitting position. Subsequent studies were performed serially, with the gravidas positioned in lateral recumbency for each measurement, and increases in plasma volume started in the first trimester, accelerated in the second, peaked near gestational week 32, and remained elevated until term. The maximal gain averages 1,100–1,300 mL, although larger increments may occur when there are multiple fetuses.
Studies in animal models demonstrate increases in both plasma and red cell volume during pregnancy. Of interest is an observation that plasma volume increases during early rat gestation even when the animals have a “zero” sodium intake, suggesting that some of the gain can be from internal redistribution of salt and water under this dietary condition.
Since expansion of the plasma volume accounts for only 20–30% of the increase in extracellular space, increases in interstitial fluid must be substantial. In his analysis of the distribution of body water during pregnancy, Hytten suggested the following: in women with no edema or leg edema only (~80% of normal gravidas), increments in interstitial fluid average 2.5 L at term, whereas in normotensive women with generalized edema the increase in interstitial fluid reaches ~5 L at term. In normal pregnant women, both with and without edema, the greatest accrual of interstitial fluid occurs in the third trimester, thus lagging somewhat behind the increment in plasma volume.
The mechanisms explaining interstitial fluid volume increases are incompletely understood. Unfortunately, there are but sporadic and/or conflicting data from both animal models and humans. Plasma albumin decreases 0.5–1.0 g/dL during pregnancy, but its concentration in interstitial fluid may fall even further; thus, paradoxically, the oncotic pressure difference favors retention of fluid within the capillaries. However, pregnancy is a vasodilated state (see below), and precapillary resistance is decreased, capillary hydrostatic pressure elevated, and, if the capillary ultrafiltration coefficient is unaltered or higher, more fluid will enter the interstitium, especially if interstitial compliance is increased. In the steady state, there would also be enhanced return of fluid to the intravascular compartment and increased removal of protein through the lymphatics.
There is also speculation that some of the interstitial changes during gestation are due to alterations in the properties of connective tissue ground substance. Thus, although low-molecular weight substances (e.g., cellular nutrients) diffuse readily through this material, fluid is “complexed” and poorly mobilized by diuretics. Furthermore, alterations in interstitial compliance, mediated through humorally induced changes in mucopolysaccharides, could conceivably influence blood pressure. Data in favor of such a hypothesis are sparse (reviewed in Refs ) but provocative, and await further study.
On the one hand, the normal gain in interstitial volume during pregnancy may reduce the safety margin for edema formation in pathological states, thus explaining why previously healthy gravidas may develop pulmonary edema when tocolytic therapy or the development of preeclampsia provokes additional fluid retention. On the other, there is the theoretical advantage of providing a large pool of interstitial fluid, which can be mobilized into the intravascular space when sudden depletion occurs, for example, by hemorrhage. Finally, increased fluid filtration across the capillary may protect the gravida from circulatory overload whose total blood volume is already increased.
In summary, pregnancy is characterized by the accumulation of >7 L of fluid, which is stored not only in the products of conception but also in the maternal intracellular, plasma, and interstitial compartments. In essence, there is maternal “physiologic hypervolemia.” However, the volume receptors apparently reset to the hypervolemic state, thus sensing it as normal, and with imposition of salt restriction or diuretic therapy, the maternal response is similar to that observed in salt-depleted nonpregnant subjects (see below).
A pregnant woman accrues ~950 mEq of sodium ( Table 81.1 ), which is distributed between the products of conception and the maternal extracellular space (see above). This positive balance occurs gradually throughout gestation with the third trimester being the period of most rapid accumulation; however, the quantity retained is too small to be detected by conventional balance techniques. Renal sodium handling is the primary determinant of volume homeostasis, thus a brief review of the hemodynamic and humoral changes of normal gestation, which might influence urinary sodium excretion follows.
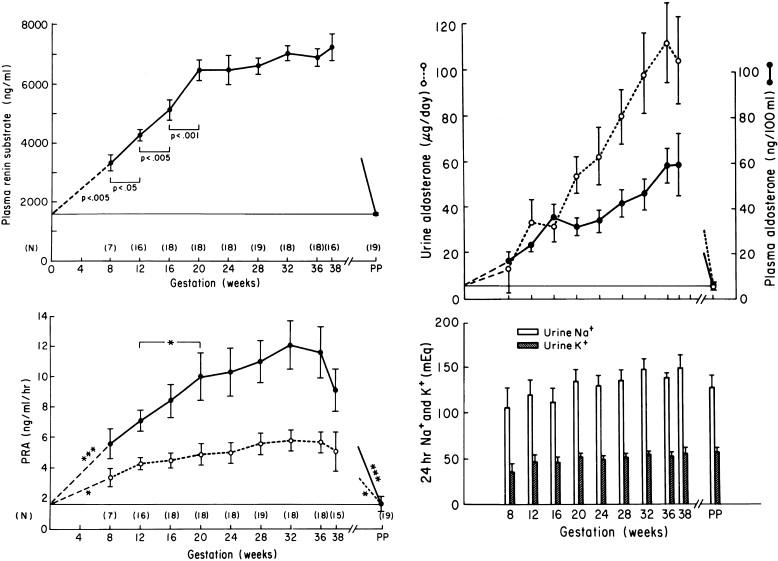
Circulating levels of many antinatriuretic hormones, mainly mineralocorticoids (e.g., aldosterone and DOC) increase during gestation, often markedly (see the previous edition, and Refs, which provide reviews and monographs with detailed bibliographies). In this regard, the renin–angiotensin system is the control mechanism most studied, and Figure 81.13 summarizes a detailed study by Wilson et al. in which plasma renin substrate, activity (Plasma renin activity), and urinary sodium and potassium excretion were measured throughout gestation. Note the sequential increases in plasma renin substrate and activity, which start early in gestation. Salt excretion (reflecting intake) was similar during gestation and in the postpartum period, suggesting that inadequate sodium intake does not account for these rises. Moreover, despite these high circulating levels of plasma renin substrate and activity, the renin–angiotensin system responds appropriately to provocative maneuvers, e.g., circulating levels decrease after saline infusion or during a high salt diet, or rise further after the administration of diuretics or when dietary sodium is restricted. Furthermore, inhibition of aldosterone biosynthesis causes a diuresis and subtle signs of volume depletion, the salt loss already apparent when aldosterone excretion, though decreasing, is still considerably above nonpregnant levels. Thus, the renin–angiotensin system does not function autonomously during pregnancy as some have presupposed. Rather, the high circulating levels of aldosterone, which often exceed those measured in nonpregnant patients with primary aldosteronism, are appropriate in pregnancy responding to homeostatic demands.
Nevertheless, physical factors do seem to have a greater influence on renal handling of salt during pregnancy then they do in the nonpregnant state including the antinatriuretic potential of the upright or supine position, and perhaps the vascular changes in the uterus especially in late gestation which has been likened to an arteriovenous shunt. In pregnancy, therefore, the supine and upright positions are markedly antinatriuretic, and quiet standing may cause greater reductions in sodium excretion in pregnant than in nonpregnant women. Thus, bed rest in the lateral recumbent position is helpful in the rare instances when a diuretic appears necessary.
Postural influences may also underlie the circadian rhythms of solute and water excretion in pregnant women. Recumbent gravidas typically display patterns of urine flow, creatinine clearance, and aldosterone and electrolyte excretion similar to those of nonpregnant subjects (i.e., daytime peaks and nighttime nadirs). However, ambulation results in more striking changes during pregnancy than in the nonpregnant state, and excretory peaks frequently occur at night (reviewed in Refs ). On the other hand, nighttime excretion of sodium and solute-free water may be greatest early in pregnancy when postural effects are minimal, suggesting that humoral, rather than mechanical factors are responsible for these changes.
Many hormones and autocoids change during pregnancy, which can theoretically enhance renal sodium excretion. These include increased circulating levels of oxytocin, melanocyte stimulating hormone, progesterone, natriuretic peptides, vasodilating PGs, and NO (for literature reviews see Chapter 100 in the first edition and Refs ). Progesterone levels increase markedly even over those observed during the luteal phase of the menstrual cycle, and binds with higher affinity than aldosterone to the mineralocorticoid receptor prompting investigators to question how aldosterone functions in face of such high circulating levels of progesterone. One possibility may be that progesterone actually contributes to antinatriuresis, as it is the major source of DOC production during pregnancy. Because renal steroid 21-hydroxylase activity (the enzyme that converts progesterone to DOC) may be particularly high in pregnancy, a considerable portion of maternal DOC may be produced in the vicinity of the renal receptors whose stimulation enhance sodium reabsorption.
There is considerable literature devoted to the various natriuretic factors and Na + –K + ATPase inhibitors in pregnancy, but their influence on renal sodium excretion during pregnancy is also obscure. In particular, the production of atrial natriuretic peptide (ANP) exceeds increases in metabolic clearance, so that circulating levels are increased. However, the increments in P ANP are quite modest in relation to the marked increases in extracellular volume that occurs in normal pregnancy. Finally, the renal resistance to the natriuretic effects of atrial peptides described in animal models does not seem to occur in human gestation.
Perhaps, the major factor of importance when considering renal salt handling during pregnancy is the profound increase in GFR. Thus, every day more than 10,000 additional milliequivalents of sodium are filtered that must be reabsorbed by the renal tubules, a quantity which greatly exceeds the salt-retaining effects of large amounts of aldosterone, DOC, or estrogens administered experimentally. Quantitatively, the increase in filtered load of sodium is so enormous that one might anticipate that it would render gravidas more vulnerable to salt and volume depletion. Thus, on the one hand, gravid rats tolerate sodium restriction and adrenalectomy more poorly than do the virgin controls but, on the other, all pregnant species including humans are in positive sodium balance, and as noted, many women exhibit edema at some point of their gestation.
Whether salt-retaining or salt-losing influences predominate during gestation might be clarified by testing the capacity of pregnant and nonpregnant subjects to excrete saline loads. In the older literature, most studies lack nonpregnant controls. An exception is that of Chesley and colleagues, who infused 3% saline (410 mEq Na over 30 min) and observed that pregnant subjects excreted the administered sodium as well as the nonpregnant controls despite the fact that they were tested in the supine position and moderately sodium restricted prior to the test. These results, however, were disputed by Weinberger et al., who observed that gravid subjects given 2 L of isotonic saline over 4 h excreted significantly less sodium than comparably treated nonpregnant controls. More recently, in an extensive and meticulously conducted study in which dietary sodium intake was controlled, and the subjects were evaluated serially during the second and third trimesters and again postpartum, Brown et al. confirmed the original observations of Chesley and coworkers. A similar conclusion was reached in an animal study, in which term pregnant rats excreted acute sodium loads as well as, or better than, virgin littermate controls; however, the animals were anesthetized.
Acute imposition of sodium loads does not necessarily relate to the homeostatic processes involved in sodium balance that occur over the course of an entire gestation. Consequently, several investigators conducted metabolic balance studies in an attempt to assess salt handling over a more prolonged period during pregnancy. Some authors concluded that gravidas have an impaired ability to conserve sodium and may show signs of volume depletion when dietary salt content is too low, whereas others stated that pregnant and nonpregnant subjects withstood challenges to sodium balance in a comparable fashion (reviewed in Refs ). Bay and Ferris reported that pregnant women achieved balance as rapidly as nonpregnant controls while consuming diets containing as little as 10 mEq of sodium daily. Urinary sodium excretion decreased to similar values in pregnant and nonpregnant subjects 5–7 days after the low salt diet was instituted. These data, however, may lead to different conclusions from those reached by the authors when the following factors are considered: the small daily positive balance of 3–6 mEq in late gestation is too small to be detected by routine metabolic studies, and gravidas appear to excrete all their ingested sodium. Moreover, when gravid subjects are salt restricted, the increased sodium demands of pregnancy should make them resemble patients with cirrhosis or congestive heart failure who virtually eliminate sodium from their urine. Hence, the dietary restriction of 10 mEq daily in the report by Bay and Ferris should have revealed discernible differences in sodium balance between pregnant and control subjects. However, the gravidas in this study actually excreted 1–2 mEq more than the nonpregnant women, failed to gain the 1–2 lb of weight expected during a 7-day period in late gestation, and actually lost >2 lb. Also, plasma aldosterone increased to levels, which are considered high even for pregnant women. Thus the data of Bay and Ferris actually support conclusions contrary to the one they made, i.e., some salt-restricted pregnant women are prone to subtle sodium wasting, and others may achieve balance by invoking compensatory mechanisms such as adrenal steroid production.
In summary, there is a positive, cumulative salt balance during gestation, which amounts to a few milliequivalents of sodium daily. There are many physiological changes during pregnancy that impact sodium balance including the rise in GFR, the effects of physical factors, altered plasma levels of both antinatriuretic and natriuretic hormones, etc., but to what degree each contributes to the overall renal handling of sodium during pregnancy remains uncertain. On the one hand, the vast array and complexity of changing factors during pregnancy that affect sodium balance may render gravid women particularly susceptible to pathological outcomes should a component(s) of this intricate control system be amiss, e.g., the appearance of generalized edema and even obscure hypokalemia occasionally encountered in otherwise normal gravidas. On the other, the vast array and complexity of changing factors in pregnancy may be advantageous and evolutionarily conserved because of the inherent redundancy of mechanisms that can compensate one for the other, in the event that one or more should fail.
On the one hand, the physiological hypervolemia may be a suboptimal response to the general arterial vasodilation of pregnancy, the so-called “underfill” or “primary arterial dilation” theories. On the other, the volume changes may be a primary event arising from the marked increase in antinatriuretic factors such mineralocorticoids, the so-called “overfill” theory. However, an intermediate possibility is that volume-sensing mechanisms are continually reset as gestation progresses, and as such, the increments in absolute volume are “sensed” as normal (“normal-fill”). These contrasting hypotheses, previously mentioned in the section on osmoregulation, are clarified further below (see Ref. for extensive review).
Evidence supporting the “underfill” theory is detailed by Schrier and Duvekot and their respective colleagues, and includes the marked activation of the renin–angiotensin system, substantiated not only by an increase in all of its circulating components ( Figure 81.13 ) but also by the observation that pregnant women manifest exaggerated increases in aldosterone release in response to low-dose infusion of angiotensin II. There is also evidence that the gestational decline in systemic vascular resistance precedes intravascular volume expansion, thus supporting the “primary arterial vasodilation” theory, and administration of angiotensin-converting enzyme (ACE) inhibitors early in pregnancy evokes exaggerated decrements in blood pressure. Finally, as noted, adrenalectomy, sodium restriction, or both, are tolerated more poorly in pregnant animal models.
The “overfill” theory is supported by increases in renal hemodynamics and GFR, absolute increments in extracellular and intravascular volumes, elevation in the levels of circulating natriuretic factors and inhibitors of Na + –K + ATPase, and by a report of increased sodium excretory capacity in response to saline infusions. Gravidas also appear more susceptible to complications of volume overload, especially those with underlying cardiac or renal disorders, or those receiving tocolytic therapy with sympathomimetic agents. In addition, they seem to tolerate blood loss better than do nonpregnant women. Finally, the mean circulatory filling pressure measured in gravid rodents has been consistently described as high normal or increased as discussed further in Ref.
Evidence for “normal-fill” is supported by animal experiments demonstrating the relationship between intravascular volume depletion and AVP release (detailed in the section on osmoregulation and Refs ). Also studies in rats and humans using indices of proximal tubular function such as fractional lithium and free water clearances suggest that sodium and water reabsorption by this nephron segment are unaltered. Moreover, with water loading both species dilute their urine normally or better than nonpregnant controls. Of note here is that failure to dilute the urine normally and excrete water and sodium are major pathophysiological features of hyponatremic patients with cirrhosis or cardiac failure, the prototypic diseases in which absolute extracellular and intravascular volumes are increased while “effective circulating volume” is low. Pregnancy, however, is a physiological condition, and thus salt and water excretory responses to acute sodium and water loads are comparable in pregnant and nonpregnant populations consistent with the concept that pregnancy is a “normal-fill” state (see Refs cited above and ). Finally, as detailed elsewhere, circulatory performance during gestation (including the adequate response to exercise) is further evidence that gravidas “sense” their intravascular volume as normal.
In summary, disputes surrounding the true nature of the volume accrual in pregnancy as noted above are yet to be settled, and it may be that all views are correct with each being apropos depending on the stage of gestation, e.g., early primary vasodilation followed by rapid compensation to normal-fill, and in some cases, overfill during late gestation due to a predominance of antinatriuretic influences such as physical factors at that time. Settling these controversies should perhaps be a priority, because understanding how the pregnant woman “senses” her volume changes may have wider implications for our understanding and management of gravidas with cardiac disease and hypertensive disorders such as preeclampsia.
This section surveys renal and obstetrical outcomes in pregnancies associated with kidney disease, including acute problems (e.g., urinary tract infection and sudden renal failure), as well as the natural history of gestation in women with chronic renal parenchymal disorders. Once, women in the latter category were advised against conception, while many who had already conceived had their gestations terminated, regardless of renal functional status. Data collected during the past three decades, albeit primarily retrospective, has led to a more rational and optimistic approach to counseling these patients, as well as to guidelines for managing their gestations. Of note, most women with chronic kidney disorders but preserved, or only mildly compromised renal function, can anticipate successful pregnancy outcomes with minimal risk of accelerating their disease.
The approach to gravid women with renal problems is similar to that in nonpregnant populations, although tests which utilize ionizing radiation or radiochemicals should obviously be deferred until after pregnancy unless deemed crucial. Exposures to #5 rads do not appear to harm the fetus. The effect of the enhanced GFR, as well as alterations in acid-base parameters, and osmoregulation, on normal ranges of circulating creatinine, urea nitrogen, bicarbonate, sodium, and osmoles; blood pH and CO 2 tension were discussed in the previous section and will not be repeated here. Ammonia loading to determine the kidney’s ability to excrete protons and achieve a minimal urine pH is rarely performed in pregnancy, and gravidas may be more susceptible to NH 4 Cl-induced nausea than nonpregnant women. When assessing GFR by endogenous creatinine clearance the lower limits of normal should be increased by ~30%. Of note, other endogenous proteins easily measured in clinical labs have recently suggested as better markers of GFR than creatinine levels. One, especially, Cystatin-C has been recommended for use in pregnant women, but its validity for use in pregnancy has been recently questioned. Finally, when timed urines are neither practical (e.g., decisions during labor) nor reliable use of the Cockcroft–Gault formula based on preconception body weight can be utilized.
Most, but not all, investigators detect increases in urinary protein excretion in pregnancy. Accepting the relative imprecision and variabilities of the methods used by hospital laboratories (as well as the fact that certain proteins remain undetected by some and not by other tests), 300 mg/day should be considered the upper limit of protein excretion in pregnancy. There are limited data on normal limits and validity of protein and/or albumin creatinine ratios in gestation. As previously discussed, the fate of urinary albumin excretion is disputed. Even if it does rise, the increments are quite small, and thus use of nonpregnant upper limits of normal is probably permissible. Urine albumin excretion may have predictive value in relation to pregnancy outcome in women with diabetes, and those at high risk for preeclampsia but more research is needed here.
One should recall that as many as 5% of healthy adolescents and young adults manifest postural proteinuria, and this may become apparent or be first detected during pregnancy, especially near term when gravidas tend toward lordosis, a posture that augments urinary protein excretion. Finally, studies of tubular proteinuria, as well as enzymuria in either normal gravidas or those with renal disorders have sporadically appeared [summarized in Refs ]. These measurements are yet to be proved useful in the detection and management of renal disorders in pregnant women.
There have been few attempts to quantitate the urine sediment in pregnancy. Whether or not there is an increase in leukocyturia is unclear, but excretion of red blood cells definitely rises, so that 1–2/RBC per high-power field, considered abnormal in nonpregnant patients is probably acceptable in gravidas. One should be aware, though, that microscopic and even gross hematuria may complicate otherwise uneventful gestations. When this occurs, the differential diagnosis includes all causes of urinary tract bleeding in nonpregnant populations, but often a cause cannot be found and the bleeding subsides postpartum. In some cases, the hematuria may be due to the rupture of small veins around the dilated renal pelvis, the bleeding recurring with subsequent pregnancies. When faced with de novo hematuria in a pregnant woman, we follow up the urinalysis with ultrasonographic or magnetic resonance imaging (MRI), deferring more extensive investigations to the postpartum period.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here