Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The clinical manifestations and complications of atherosclerosis are the most common therapeutic challenges encountered by vascular surgeons. The tendency for lesions to develop at specific anatomic sites and to follow recognizable patterns of progression was appreciated as long ago as the late 1700s by the extraordinary British anatomist and surgeon John Hunter. Considered one of the forefathers of vascular surgery, his dissections of atherosclerotic aortic bifurcations remain on view at the Hunterian Museum in London and presage the disease process that Leriche would give name to 150 years later.
The modern era of surgical reconstruction for complex atherosclerotic occlusive disease began in earnest in 1947, when the Portuguese surgeon J. Cid dos Santos successfully endarterectomized a heavily diseased common femoral artery. Four years later, Wylie and coworkers in San Francisco extended this new technique to the aortoiliac level. At the same time, and building on the pioneering work of Alexis Carrel, Kunlin would report the first long segment vein bypass in the lower extremity, in 1948. It would be another 10 years before synthetic grafts were being regularly used for aortic bypass grafting and the first efforts to extend vein grafting to the tibial level were described by McCaughan. Tremendous advances in both the understanding of atherosclerosis biology and the ability to treat arterial occlusive disease percutaneously have dramatically impacted the treatment algorithms for arterial insufficiency in recent years. This chapter will review the current role for the surgical management of aortoiliac and infrainguinal arterial occlusive disease.
Chronic obliterative atherosclerosis of the distal aorta and iliac arteries commonly manifests as symptomatic arterial insufficiency of the lower extremities. Disease in this location is seen often in combination with occlusive disease of the femoropopliteal arteries, producing a range of symptoms from mild claudication to more severe levels of tissue loss and critical ischemia. Patients with hemodynamic impairment limited to the aortoiliac system may have intermittent claudication of the calf muscles alone or involvement of the thigh, hip, and/or buttocks. If the disease distribution also targets the hypogastric vessels, patients may additionally suffer from difficulty in achieving and maintaining an erection, resulting from inadequate perfusion of the internal pudendal arteries. A well-characterized constellation of symptoms and signs, known as the Leriche syndrome, which is associated with aortoiliac occlusive disease in the male, includes thigh, hip, or buttock claudication, atrophy of the leg muscles, impotence, and reduced femoral pulses. While vasculogenic female sexual dysfunction has been described, the equivalent impact of impaired pelvic perfusion in women remains poorly understood and more research is needed to discern the true incidence and the appropriate treatment. A meta-analysis did demonstrate fewer complications in women compared to men when one or more hypogastric arteries was disrupted by embolization, coverage, or ligation. The authors attributed this to the fact that most of the female patients in the study had obstetric-related pathologies, while more men had trauma, vascular, or oncologic indications for treatment. The authors further speculated that the younger age and the increased levels of estrogen in the female cohort may have contributed to the gender- related differences that were seen.
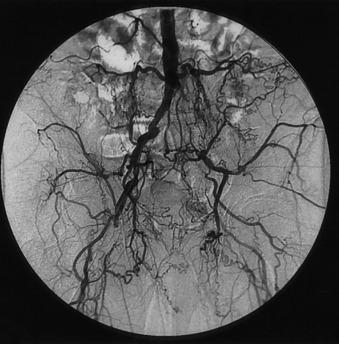
While atherosclerotic disease limited to the aortoiliac region commonly gives rise to claudication of varying degrees, it is rarely associated with lower extremity ischemic rest pain or ischemic tissue loss. This is largely the result of adequate collateralization around the point of obstruction via lumbar, sacral, and circumflex iliac vessels that serves to reconstitute the infrainguinal system with enough well-perfused arterial blood to ensure sufficient resting tissue perfusion ( Fig. 21.1 ). A well-recognized exception to this general observation arises in the situation of embolic disease. The so-called blue toe syndrome represents a situation where atherosclerotic debris breaks free from an aortic or iliac plaque and embolizes to the distal vessels (see Chapter 45 ). Wire manipulation during coronary or peripheral angiographic procedures and cross-clamping across a calcific aortic plaque during cardiac surgery are common sources of such emboli. The terminal target of the microembolic particles, be they cholesterol crystals, calcified plaque, thrombus, or platelet aggregates, is typically the small vessels of the toes.
If, on the other hand, aortoiliac occlusive disease is found in combination with femoropopliteal occlusive disease, ischemic rest pain, or even more severe perfusion impairment leading to ischemic tissue loss or gangrene is not uncommon. Such progressive disease, affecting multiple levels of the peripheral vasculature tree, is most frequently encountered in the elderly. Approximately one-third of patients operated on for symptomatic aortoiliac occlusive disease have orificial profunda femoris occlusive disease, and more than 40% have superficial femoral artery occlusions. Aortoiliac disease typically begins at the distal aorta and common iliac artery origins, and slowly progresses proximally and distally over time. This progression is quite variable, but may ultimately extend to the level of the renal arteries or result in total aortic occlusion.
A particularly virulent form of atherosclerotic arterial disease is often found in young women smokers. Radiographic imaging in this subset of patients typically reveals atretic, narrowed vasculature with diffusely calcific atherosclerotic changes. Frequently, a focal stenosis is found posteriorly near the aortic bifurcation. This particular distribution of disease and the characteristic patient profile have been referred to as the small aortic syndrome ( Fig. 21.2 ). Such patients invariably have an extensive smoking history, with or without other typical factors for atherosclerosis. While the diminutive size of the aorta and iliac vessels has led to compromised durability when treated endovascularly, ongoing improvements in percutaneous technology have resulted in better outcomes in this patient population in more recent years.

The diagnosis of aortoiliac occlusive disease is generally made based on patient symptomatology, physical examination, and noninvasive tests such as segmental pressure measurements and pulse volume recordings (see Chapter 18 ). Following the diagnosis of aortoiliac disease and the decision to pursue intervention, further imaging is warranted. In many centers, magnetic resonance angiography (MRA) (see Chapter 13 ) or computed tomographic angiography (CTA) (see Chapter 14 ) has supplanted catheter-based angiography (see Chapter 15 ) as the initial imaging study of choice. Should a lesion amenable to percutaneous therapy be identified, catheter-based angiography is then pursued. In cases in which a good quality roadmap is obtained with MRA or CTA and the clinical situation or anatomic pattern is unfavorable to a percutaneous approach, surgery can, in most instances, be planned directly from the MRA, obviating the need for traditional subtraction angiography.
In the minority of cases necessitating digital subtraction angiography for preoperative planning, a retrograde femoral approach is typically utilized, while the transbrachial approach serves as a useful alternative in patients with particularly challenging anatomy (see Chapter 15 ). Additional lateral and oblique views of the abdominal aorta are advised if concomitant mesenteric or renal occlusive disease is present and multiple projections of the iliac and femoral bifurcations are essential in clarifying the extent of disease in these regions (see Chapter 15 ). Finally, full runoff views of the lower extremities are needed to assess the presence or absence of femoropopliteal or crural disease. In ambiguous cases, pullback pressure measurements, both before and after the administration of a systemic vasodilator, such as papaverine or nitroglycerine, or the application of a tourniquet to induce reactive hyperemia, can be useful in documenting the hemodynamic significance of a particular stenotic zone. Finally, the use of gadolinium or carbon dioxide as contrast agents in patients with compromised renal function can minimize or eliminate the nephrotoxic effects associated with standard iodinated contrast medium.
Risk factor modification remains a cornerstone of the management of aortoiliac occlusive disease (see Chapter 19 ). Smoking cessation, blood pressure control, and aggressive efforts at cholesterol lowering should be addressed with every patient with atherosclerotic disease. Strong evidence exists supporting the benefit of a structured walking program in increasing the walking distance of patients with claudication; it is hoped that utilization of this important treatment strategy will increase now that it is a reimbursable therapeutic option. Interestingly, studies have failed to identify any exercise components; for example, intensity, duration, or content, which independently predict improvements in maximum walking distance and pain-free walking distance. The benefit of walking outside of a structured regimen with close follow-up is more debatable. Medical management with cilostazol has benefit in a subset of patients and is a reasonable first line approach to improve claudication symptoms. Recent studies have found lower rates of restenosis, amputation, and target lesion revascularization in claudicants treated with cilostazol.
There has been a considerable change in the management approach to claudication in recent years. Anyone suffering from disabling claudication, rest pain, or ischemia-related tissue loss continues to warrant serious consideration for arteriography and either percutaneous or surgical intervention. Previously, such aggressive treatment would have been considered inappropriate for claudication that was not clearly disabling. However, as percutaneous treatment has become increasingly safer and more effective, and its application has spread to increasingly more arterial beds, the indications for transluminal angioplasty have correspondingly increased (see Chapter 20 ). Such a sea change in the overall management approach to aortoiliac disease has had a dramatic impact on the numbers of patients now proceeding to open surgery. The rising popularity and success of aortic and iliac balloon angioplasty and stenting as first-line therapy has noticeably reduced the volume of aortoiliac reconstructive procedures performed in this country.
When medical therapy or percutaneous treatment has proven inadequate or is technically inadvisable, open surgical revascularization remains indicated for those patients with aortoiliac disease and disabling claudication, ischemic rest pain, and ischemic ulceration or gangrene. Patients with nighttime foot rest pain or tissue loss usually have multisegment disease and the decision whether to perform both supra- and infra-inguinal revascularization procedures or to perform only an inflow procedure is guided by the severity of the ischemia. In general, patients presenting with significant tissue loss or gangrene are much more likely to require simultaneous or staged inflow and outflow procedures.
The numerous surgical options available to the trained vascular surgeon allow tailoring of the approach to the particular overall and anatomic situation of each patient. Historically, the reconstructive options for aortoiliac occlusive disease include aortoiliac endarterectomy, aortobifemoral bypass, and so-called extra-anatomic revascularization in the form of iliofemoral, femorofemoral, or axillofemoral grafting.
Aortic endarterectomy was commonly performed in the early era of aortoiliac reconstruction. While it is particularly suited to localized disease limited to the distal aorta or proximal iliac arteries, it has proven to be less reliable for disease involving the entire infrarenal aorta and extending into the external iliac arteries. The obvious benefit of endarterectomy is the elimination of the need for a prosthetic graft, removing the possibility of the myriad late graft-related complications. The long-term patency of limited endarterectomy is excellent and on par with bypass procedures. However, the number of patients suitable for this reconstructive approach is small and continues to diminish in the era of endoluminal reconstruction. Experience with endarterectomy during one’s training or early surgical career is another important factor influencing the choice of therapy offered, as significant technical expertise is required and many surgeons in the current era have limited familiarity with this approach.
Aortobifemoral bypass remains the mainstay of operative treatment for aortoiliac occlusive disease. During the last 20 years, the procedure has supplanted both aortic endarterectomy and aortoiliac bypass procedures. In the latter case, this change was largely driven by the recognition of subsequent graft failure due to progression of native iliac arterial disease. Early experience with aortobifemoral grafting in the 1970s was associated with a 5% to 8% 30-day operative mortality rate. Over recent decades, mortality rates of 1% have been reported, on par with that of elective abdominal aortic aneurysm repair.
Typically, half of patients proceeding to surgery for aortoiliac occlusive disease will have significant coronary artery disease, while even more will have hypertension and almost 80% will be current or prior cigarette smokers. The reduced mortality and morbidity seen in recent years is in large part due to advances in the management of concomitant coronary disease. Specifically, the importance and benefit of better preoperative identification of patients in need of initial coronary revascularization, awareness of the benefit of waiting an interval period following coronary stenting prior to proceeding with major noncoronary vascular surgery, improved perioperative pharmacologic management of patients with impaired myocardium, and more focused efforts to tailor operative and postoperative fluid administration to the individual patient’s myocardial reserve are all well-recognized. General advances in postoperative intensive care unit management, including pulmonary care, infection control, and blood product utilization, have further contributed to the progress seen.
Current early patency rates for aortobifemoral bypass grafting are excellent, approaching 100% in many reporting institutions. Five-year patency rates are greater than 80% while 10-year rates are near 75%. There are multiple reasons for the improved patency. The current graft material used by most surgeons for aortoiliac reconstruction is a knitted Dacron prosthesis, which has enhanced hemostatic properties and which tends to have a more stable pseudointima than the earlier used woven grafts. More attention is paid to avoiding graft redundancy and to ensuring a good size match between the graft and the recipient vessels. Grafts are more routinely extended beyond the iliac level to the femoral vessels, which not only improves exposure and makes for a technically easier distal anastomosis, but is also associated with less graft thrombosis from unanticipated progression of atherosclerotic disease in the external iliac vessels. With meticulous skin preparation, close attention to draping, careful surgical technique, and judicious use of a short course of intravenous antibiotic therapy, the feared higher rate of graft infection from placing the distal dissection at the groin has not materialized. However, an exception to this general practice is recommended in certain circumstances. For example, patients with hostile groin creases from prior surgery or radiation therapy, or obese, diabetic patients with an intertriginous rash at the inguinal crease will all likely be better served by performing the distal anastomosis at the external iliac level if their anatomy for such a procedure is suitable.
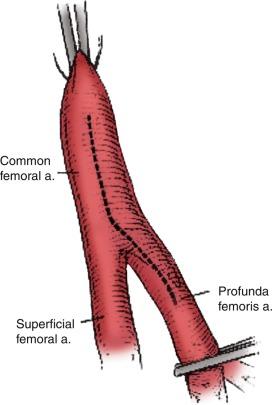
The increased awareness of the critical role played by the deep femoral artery in preserving the long-term patency of aortobifemoral grafts has also undoubtedly contributed to the better results seen. This awareness parallels a better overall appreciation for the importance of establishing adequate outflow at the femoral level in achieving higher early and late graft patency rates and sustained symptom relief. The true impact of concomitant superficial femoral artery disease is unclear from the literature. Some reports have indicated similar patency rates between those patients with and without superficial femoral artery occlusion, while others have suggested that late patency rates are reduced in this setting. What has definitely been shown is the benefit of a profundaplasty in the presence of significant superficial and profunda femoral occlusive disease. Some authors have even recommended that a profundaplasty should be carried out in every case of superficial femoral artery occlusion, even in the absence of orificial profunda disease, arguing that a “functional” obstruction on the order of 50% stenosis is present in these patients. While this position has not been universally adopted, it is now common practice to extend the hood of the distal anastomosis over the origin of the profunda femoral artery to enhance the graft outflow, especially in situations in which the superficial femoral artery is occluded or severely diseased. In the presence of significant common femoral or profunda femoral origin plaque, an extensive endarterectomy and/or profundaplasty is indicated ( Fig. 21.3 ). In these circumstances, it is preferable to close the endarterectomized recipient bed with a vein, bovine pericardial or Dacron patch, onto which the distal anastomosis can then be attached, rather than creating a long femoris patch with the graft limb.
There are several technical considerations related to aortobifemoral bypass grafting, which are the subject of considerable and passionate debate. The first involves the manner of the proximal anastomotic creation. Advocates of an end-to-end configuration claim that it facilitates a more comprehensive thromboendarterectomy of the proximal stump and allows for a direct, more in-line flow pattern, with less turbulence and more favorable flow characteristics. The obviation of competitive flow through the excluded iliac vessels with this approach is likely more of theoretical rather than real benefit. Certainly, with concomitant aneurysmal disease or complete aortic occlusion extending up to the level of the renal arteries, end-to-end grafting is indicated. Creation of an end-to-side anastomosis can, at times, be technically challenging in a heavily diseased aorta partially occluded by a side-biting clamp. A lower rate of proximal suture line pseudoaneurysms and better long-term patency rates have been found in some series. Stapling or over-sewing of the distal aorta with the end-to-end technique minimizes the immediate risk of clamp-induced emboli to the lower extremities following release of the distal clamp. Finally, those in favor of this approach claim that the ability to more effectively close the retroperitoneum, particularly after resection of a short segment of the infrarenal aorta, results in a lower rate of late graft infection and aortoenteric fistulae, although there is no direct evidence to support this assertion.
There are certain circumstances, on the other hand, when an end-to-side proximal anastomotic configuration is advantageous. The most common indication involves those patients with occluded external iliac arteries, in whom interruption of forward aortic flow may result in loss of perfusion to an important hypogastric or inferior mesenteric artery and consequent significant pelvic ischemia. Colon ischemia (1% to 2%), or even more rarely, paraplegia secondary to cauda equina syndrome (< 1%), are additional complications that can be avoided by an end-to-side configuration. Although advocated by some, routine preservation of a patent inferior mesenteric artery is not universally practiced.
The operative procedure is performed under general endotracheal anesthesia, with an epidural catheter placed for postoperative pain control. The patient is sterilely prepped and draped from the mid chest to the mid thighs. The femoral vessels are first exposed through bilateral longitudinal, oblique incisions, thereby reducing the time in which the abdomen is open and the viscera exposed. The extent of exposure of the femoral vessels necessary is dictated by the severity of disease and the level of reconstruction planned of the common femoral artery and its bifurcation. Next, the inferior aspect of the retroperitoneal tunnel through which the graft will course to reach the femoral region is begun with digital manipulation posterior to the inguinal ligament and tracking along the anterior aspect of the external iliac artery. Antibiotic-soaked sponges are then placed in the groin wounds and attention is turned to the aortic dissection.
The proximal reconstruction is performed via a midline laparotomy. In general, the aortic dissection is limited to the region between the renal arteries and the inferior mesenteric artery. This allows avoidance of extensive dissection anterior to the aortic bifurcation, where the autonomic nerve plexus regulating erection and ejaculation in men sweeps over the aorta. It is interesting to note that several studies have found a similar rate of male sexual dysfunction with endovascular aortic aneurysm repair as with open surgical repair. This would suggest the effects of aortic dissection in this area are perhaps less important than historically believed.
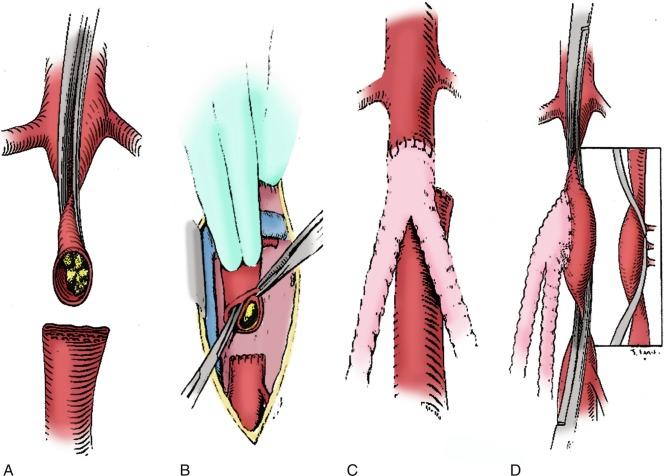
In situations where significant aortic calcification extends up to the level of the renal arteries, it may be necessary to continue the aortic dissection to the suprarenal or even the supraceliac level to allow for safe proximal clamp placement. Alternatively, proximal control may be obtained by intralumenal balloon deployment. If end-to-side repair is planned, circumferential dissection of the aortic segment to be clamped is recommended, as gaining control of any lumbar or accessory renal vessels encountered prior to performing the aortotomy helps to avoid troublesome backbleeding. The superior aspect of the graft limb tunnels is then completed, taking care to maintain a course anterior to the common iliac vessels but posterior to the ureters. Between 5000 and 7000 units of heparin are administered, with additional heparin given throughout the procedure to maintain the activated clotting time near the target range of 250 to 300 seconds. After allowing sufficient time for the heparin to circulate, atraumatic vascular clamps are placed above the inferior mesenteric artery and just below the renal arteries. The distal clamp is applied first to avoid any distal embolization of plaque dislodged with placement of the proximal clamp. If an end-to-end anastomosis is planned, the aorta is transected 1 to 2 cm below the proximal clamp and a short segment of the distal aortic cuff is excised ( Fig. 21.4 A ). This results both in better exposure of the aortic neck and a more precise proximal reconstruction and also allows the graft to lie flat against the vertebral column rather than being anteriorly oriented, facilitating later retroperitoneal coverage. If necessary, a thromboendarterectomy of the infrarenal neck is carried out at this point (see Fig. 21.4 B). The anastomosis is performed with a running suture of #3-0 polypropylene (see Fig. 21.4 C). The distal aorta is then oversewn with two layers of a running monofilament suture, or stapled with a surgical stapler. If an end-to-side anastomosis is performed, an anterior longitudinal arteriotomy is carried out after placement of proximal and distal transaortic clamps. If necessary, an endarterectomy is performed and the anastomosis carried out after the graft is beveled appropriately (see Fig. 21.4 D). If there is minimal plaque present, the distal anastomosis is performed to the common femoral artery, and individual dissection of the superficial femoral and profunda femoral arteries is not necessary.
Another point of some debate concerns the optimal management of patients with multilevel occlusive disease. The question frequently arises as to whether, or under what circumstances, a concomitant or staged outflow procedure should be performed. It is generally believed that up to 80% of patients with both inflow and outflow disease will be substantially improved following aortofemoral bypass grafting. However, other reports have suggested that between as many as one-quarter to one-third of such patients will not have significant symptomatic relief with an inflow procedure alone. While no single parameter exists to reliably guide the surgeon to know in which circumstances a combined procedure is optimal, the severity of distal ischemia is probably the most important factor to be considered. The overall medical condition of the patient and their ability to tolerate a prolonged operative procedure is also clearly important. Finally, the status of the profunda femoral artery must be taken into consideration. In the presence of superficial femoral artery occlusion, a profunda that is atretic or extensively diseased may well be unable to provide sufficient collateral runoff to the foot.
If the bypass procedure is undertaken for claudication alone or mild rest pain, restoring adequate inflow may provide sufficient and relatively durable symptomatic relief. If, on the other hand, significant tissue loss is present, a combined inflow and outflow procedure is likely warranted if limb salvage is to be achieved. If several operating teams are utilized, performing both procedures at the same time can be done in an acceptably timely fashion and has been found to be safe. Indeed, several recent reports found no significant differences in operative mortality or perioperative morbidity in patients undergoing concurrent inflow and outflow procedures compared with those having major inflow reconstruction alone. While staged revascularization may be preferable in certain circumstances, both the risk of wound and graft infection resulting from re-dissection in the groin and the risk of progressive tissue loss during the initial recuperative period must be considered with this approach.
Another solution to multilevel disease has been the utilization of hybrid approaches, which combine elements of both open surgical and endovascular therapy and which have been shown to have high technical success rates and long-term patency. Many retrospective and prospective series have indicated good limb salvage, and morbidity and mortality rates equal to or better than open bypass procedures with a hybrid approach. As iliac stenting is now the first line for treatment of amenable TASC C/D iliac lesions, a combined approach using endovascular and open techniques can often fully address both inflow and outflow simultaneously. This can offer an alternative to open approaches in medically high risk patients and significantly shorten hospital and intensive care unit lengths of stay.
Aortobifemoral bypass grafting is associated with patency rates that are among the highest reported for any major arterial reconstruction. As indicated earlier, 5-year primary patency rates of 70% to 88% and 10-year rates of 66% to 79% have been described. Better rates have been realized in those patients with good infrainguinal outflow operated on for claudication compared to those with limb-threatening ischemia and associated infrainguinal occlusive disease. In general, patients with disease limited to the aortoiliac region have excellent relief of symptoms following aortobifemoral grafting, while those with multilevel disease have less complete levels of symptom diminution. Perioperative mortality rates average 4%, while 5-year survival rates between 70% and 75% have been reported. This latter rate is notably less than the 5-year survival of the age-matched control population but is on par with that typically seen for patients with claudication in general.
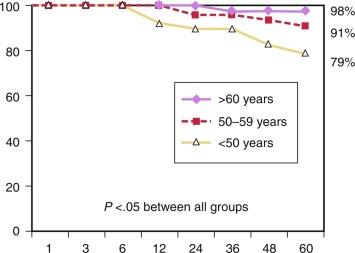
While the early and late mortality rates are similar across different age groups, the 5-year primary and secondary patency rates are significantly increased with each increase in age group. Reed and colleagues reported that primary patency rates were 66%, 87%, and 96%, and secondary patency rates were 79%, 91%, and 98% ( Fig. 21.5 ), respectively, for those < 50 years, those 50 to 59 years of age, and those > 60 years of age. Based on these findings, it seems prudent to apply caution in the application of aortobifemoral bypass grafting for younger patients with virulent aortoiliac disease. The potential impact of graft failure and the need for subsequent complex interventions should be considered, especially given the longer life expectancy of younger patients. Full utilization of all medical and endovascular options appears to be the best first-line option for younger patients with severe aortoiliac occlusive disease.
When comorbid disease renders a patient with aortoiliac occlusive disease particularly unsuitable for major vascular surgery and aortic cross clamping, or when sepsis, prior surgery or the presence of a stoma presents a hostile surgical environment for abdominal exploration, there are several alternatives available to the vascular surgeon. Such reconstructive options, in which the thoracic aorta, axillary, iliac, or femoral arteries serve as the donor vessels, are generally referred to as extra-anatomic to distinguish them from the in-line flow represented by an aortobifemoral procedure. The concept of extra- anatomic arterial reconstruction emerged in the 1950s at a time of many new developments in the field of vascular surgery. Freeman and Leeds provided one of the first descriptions in 1952 in their report of the use of the superficial femoral artery as the conduit for a crossover femorofemoral bypass graft. These approaches are also called upon in desperate situations represented by the infection of a previously placed aortic graft.
Axillobifemoral bypass grafting was introduced by Blaisdell and Hall in the early 1960s and has since enjoyed increasing popularity as an alternative to aortobifemoral bypass. This is largely due to the reliability of the axillary artery as a donor vessel and the minimal morbidity incurred, making it a particularly appealing option for patients with significant operative risk from comorbid disease. It is also appropriate in patients with significant aortoiliac occlusive disease of the distal aorta and the iliac arteries in the setting of intraabdominal sepsis, a history of multiple prior abdominal operations, intraabdominal adhesions or prior pelvic irradiation. Of note, LoGerfo and colleagues have shown that axillobifemoral grafting has improved long-term patency compared with axillounifemoral grafting, presumably due to the increased flow afforded by the second outflow limb.
Although usually performed under general anesthesia, it is possible to carry out the procedure using a combination of local anesthesia and intravenous conscious sedation. In the event that one arm has a higher blood pressure or a stronger pulse, that side should be selected as the donor site. If both sides are equal, the right axillary artery is chosen as evidence suggests there is a lower risk of arterial occlusive disease developing in the right subclavian artery compared with the left. The right side is also preferable in cases of aortic infection, as subsequent operations may require a left flank incision or left thoracotomy. In cases of groin infection, bilateral axillounifemoral artery bypass may be necessary to avoid infected wounds.
The axillary artery is exposed through a short infraclavicular incision parallel to the clavicle in the deltopectoral groove. The pectoralis major muscle is then bluntly separated between the clavicular and sternal heads, and the pectoralis minor muscle is identified and typically divided, enhancing exposure and allowing more space for the graft as it courses from the axilla to the subcutaneous space. The axillary artery medial to the pectoralis minor is then isolated as the proximal anastomosis is optimally placed as close to the chest as possible to minimize the risk of kinking or graft avulsion during rotational shoulder movement. Avoiding more lateral dissection further reduces the risk of injuring the medial and lateral cords of the brachial plexus as they emerge anteriorly to form the median nerve. A tunnel is created between the axillary and femoral arteries in the subcutaneous space, tracking deep to the pectoralis major muscle and inferiorly along the mid-axillary line before coursing medial to the anterior superior iliac spine; this latter orientation is important to avoid kinking of the conduit in the sitting position. Long, rigid tunneling devices with a removable central obturator are specifically designed for this step and have helped to lower the incidence of graft infection by obviating the need for counter incisions.
The common femoral arteries are then dissected through standard bilateral short groin incisions and a second subcutaneous tunnel is fashioned between them in an extrafascial, suprapubic plane. A Dacron or polytetrafluoroethylene graft, typically 8 mm in diameter, is then drawn through the tunnel. While there is no convincing evidence that one graft material is superior to the other, several reports support the common practice of using an externally reinforced graft. Newer grafts are available that are prefigured in an axillobifemoral configuration, thereby reducing from four to three the number of anastomoses needed. As in aortobifemoral bypass grafting, unrestricted outflow should be ensured by carrying the hood of the femoral grafts down over the profunda orifice and performing an endarterectomy or profundaplasty when necessary. If a prefigured graft is unavailable, the origin of the cross-femoral graft can be tailored to the body habitus of the patient. In most cases, the graft is taken off the distal hood of the descending axillofemoral graft. However, in particularly obese individuals, it may be preferable to move the takeoff more proximally to prevent kinking at the level of the inguinal ligament. Orienting the takeoff of the crossover graft at an acute angle to give an “S-shaped” final configuration has been associated with higher patency rates in some studies.
Many of the complications following axillofemoral grafting are directly related to the graft and are potentially avoidable. Disruption of the proximal anastomosis can be minimized by proper orientation of the proximal hood and ensuring that the descending limb of the graft is free from undue tension. Kinking and subsequent thrombosis of the graft can be reduced by strict attention to tunnel position and use of a reinforced conduit.
Given the minimal physiologic insult, most patients undergoing axillofemoral grafting are ambulatory and able to tolerate a regular diet on the first postoperative day.
The reported long-term patency rates of axillofemoral grafts have varied significantly, ranging from as low as 29% to as high as 85%. Favorable results were reported by Passman and colleagues, who achieved 5-year patency rates of 74% and a long-term limb salvage rate of 89% and who are advocates of a wider use for this approach. More recently, Liedenbaum et al. reported 3-year primary and secondary patency rates of 49% and 86%, respectively. In general, axillobifemoral grafting should be reserved for high-risk patients with significant tissue loss in danger of limb loss, and not be used for the treatment of claudication.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here