Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Screen-film radiography (SFR), also known as conventional or film-based radiography, utilizes a light-sensitive silver halide–coated film placed within a cassette containing two intensifying screens, which is placed behind the patient to be imaged and exposed to an x-ray beam. Radiographic contrast is dependent on differential attenuation of x-rays as they pass through different body tissues. The exposed film is removed from the cassette and passed through a developer to produce a hardcopy radiograph.
Computed radiography (CR) involves the digital replacement of conventional x-ray film with a reusable cassette-based phosphor imaging plate, which temporarily stores an image within the phosphor layer following x-ray exposure. The CR cassette is placed into a scanner that reads the latent image from the plate by stimulating the plate with a laser beam and converting the image to a digital signal that is displayed on a computer monitor. Specialized software allows for image magnification, optimization of image contrast and brightness, and digital archiving.
Digital radiography (DR) utilizes a digital detector panel that automatically generates a digital image upon exposure to x-ray and transfers the image in real time to a computer system without the use of an intermediate cassette as used in CR.
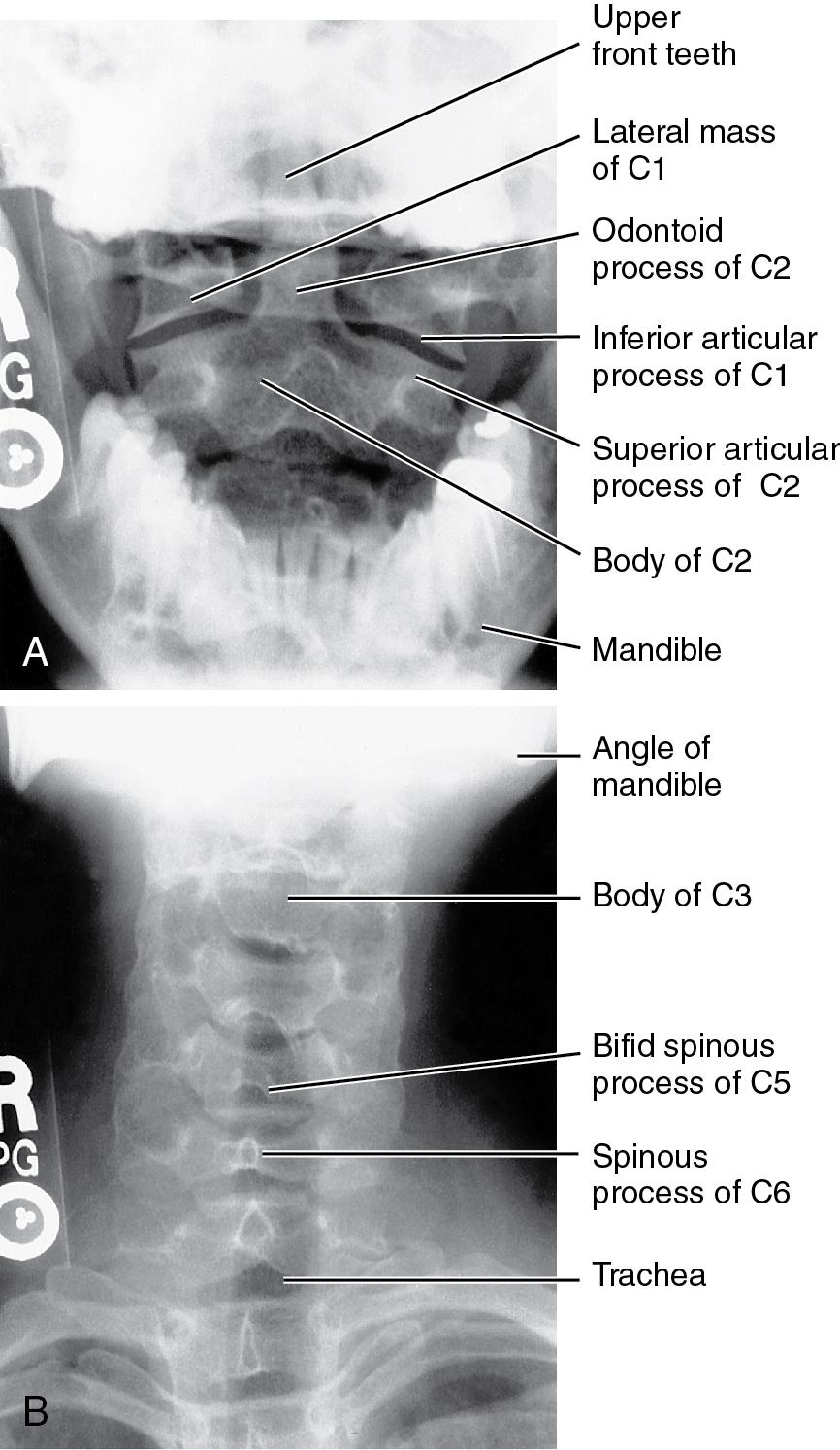
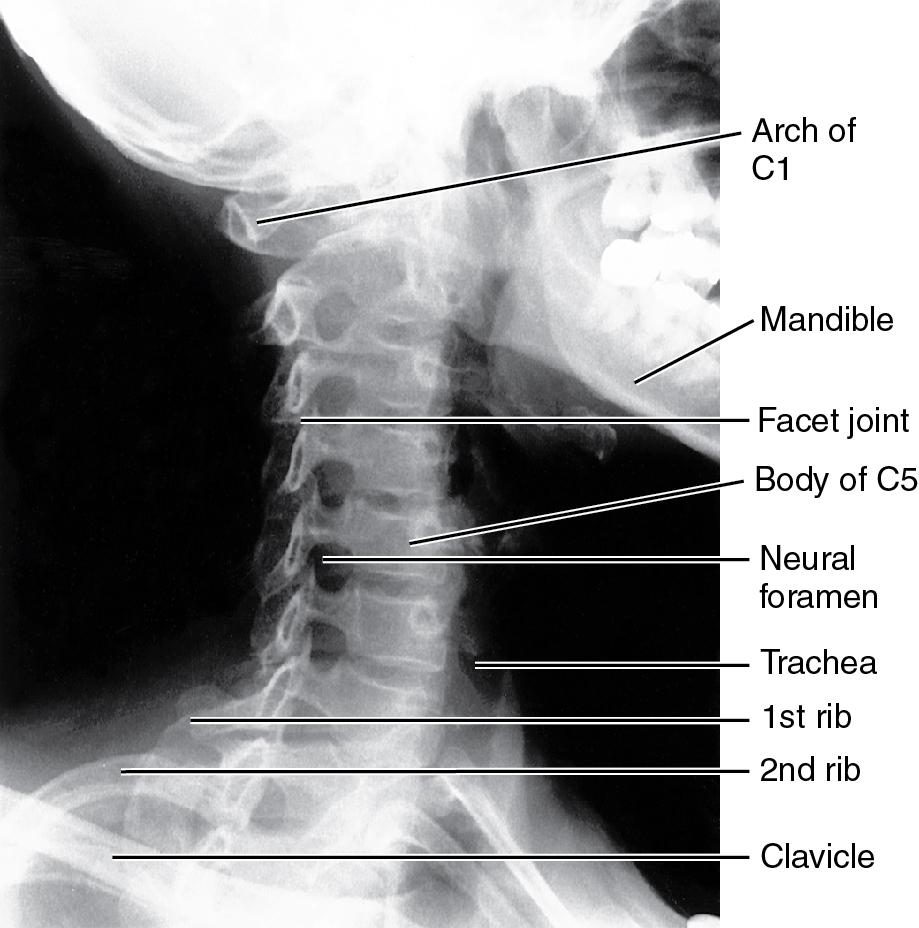
Standard cervical spine views include: lateral ( Fig. 9.1 ), anteroposterior (AP) and open-mouth AP odontoid ( Fig. 9.2 ), and right and left oblique ( Fig. 9.3 ).
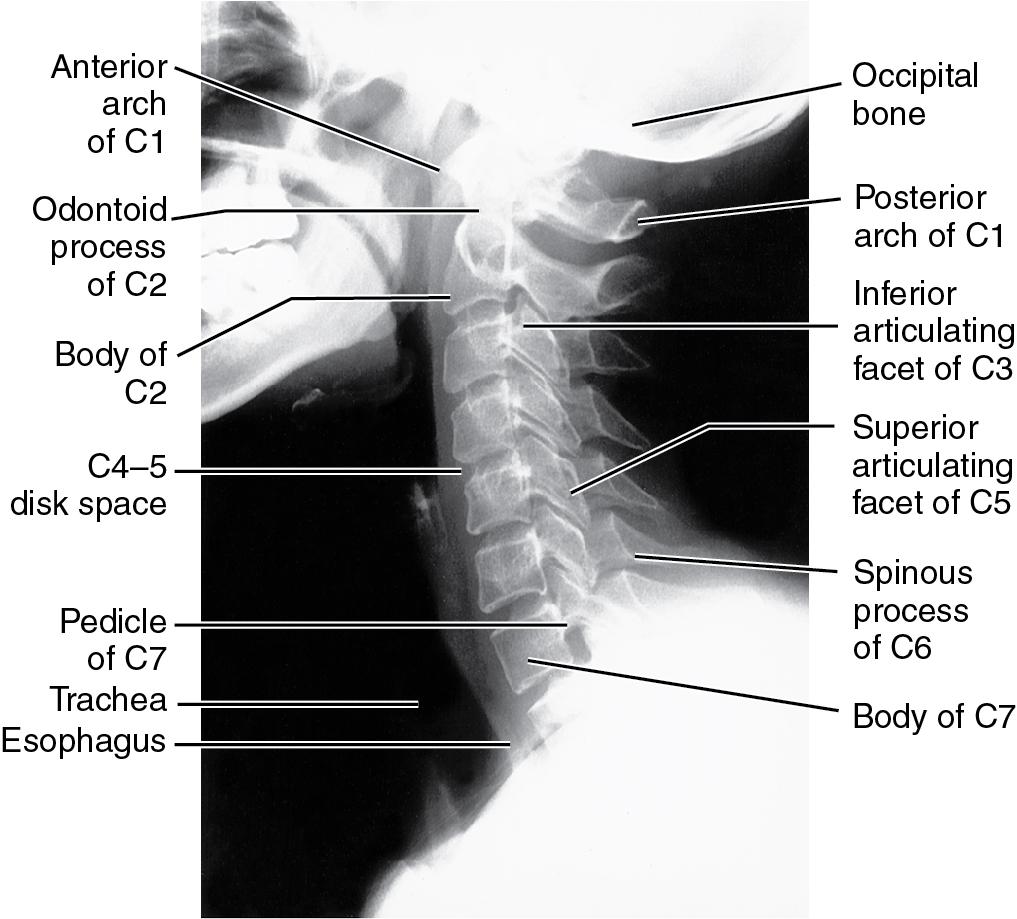
Lateral View
Assess prevertebral and retropharyngeal soft tissue shadows
Assess alignment via anatomic lines along anterior and posterior vertebral margins, spino-laminar junctions, and spinous processes
Measure the distance from the posterior margin of the anterior C1 arch to the anterior aspect of the odontoid (atlantodens interval)
Assess intervertebral disc space heights
Confirm that the superior aspect of T1 is well visualized
Open-Mouth AP Odontoid View
Check symmetry of the odontoid in relation to the lateral masses
Assess the atlantoaxial joints for symmetry
AP View
Confirm that spinous processes align with each other
Assess distance between adjacent spinous processes and vertebral endplates
Assess facet joint margins and uncinate processes
Oblique View
Assess facet joint alignment
Assess neural foramina and their bony boundaries
A swimmer’s view may be obtained when the C7–T1 level cannot be visualized on a lateral cervical spine radiograph. This view is obtained by raising the patient’s arm overhead and directing the x-ray beam obliquely cephalad through the axilla. An alternative is to obtain a cross-table radiograph with traction applied to the patient’s arms. Another option is to obtain bilateral oblique views of the C7–T1 level. Alternatively, a computed tomography (CT) scan of the cervical spine with sagittal reconstructions through the C7–T1 spinal level can be obtained.
Lateral flexion-extension cervical views should be obtained only in neurologically intact, cooperative, and alert patients. Neck motion must be voluntary and there is no role for passive or assisted range of motion during these views. Outside of the acute trauma setting, lateral flexion-extension radiographs may be used to:
Assess potential spinal instability due to soft tissue disruption when static radiographs show no significant bony injury or malalignment but clinical findings suggest a potential soft tissue injury.
Assess healing of a cervical fusion
Assess integrity of the C1–C2 articulation in patients at high risk for C1–C2 instability (e.g., rheumatoid arthritis, Down syndrome)
Lateral flexion-extension cervical radiographs are not indicated in the setting of acute trauma as they are difficult to obtain and have been shown not to provide additional clinically useful information. Because of protective muscle spasm, flexion-extension views are rarely of value in the acute postinjury period.
Increased thickness of the prevertebral soft tissue space may be a tip-off to the presence of a significant soft tissue injury involving the bony or ligamentous structures of the anterior cervical spine. This finding is less reliable in infants and children because of the wide, normal variation in the pediatric population. The normal prevertebral soft tissue shadow distance in adults is 7 mm at C2 and 22 mm at the C6 vertebral level. In general, prevertebral soft tissue thickness should not exceed 50% of the sagittal diameter of the vertebral body at the same level.
Abnormal widening of the space between the posterior aspect of the anterior arch of C1 and the anterior aspect of the odontoid (dens) defines an atlantoaxial subluxation and implies laxity of the transverse ligament. This space should not be greater than 3 mm in adults or 5 mm in children. Common causes of atlantoaxial subluxation include trauma, rheumatoid arthritis, and Down syndrome.
Commonly accepted radiographic criteria for diagnosing clinical instability in the middle and lower cervical spine (C2–T1) include sagittal plane translation greater than 3.5 mm or sagittal plane angulation greater than 11° in relation to an adjacent vertebra.
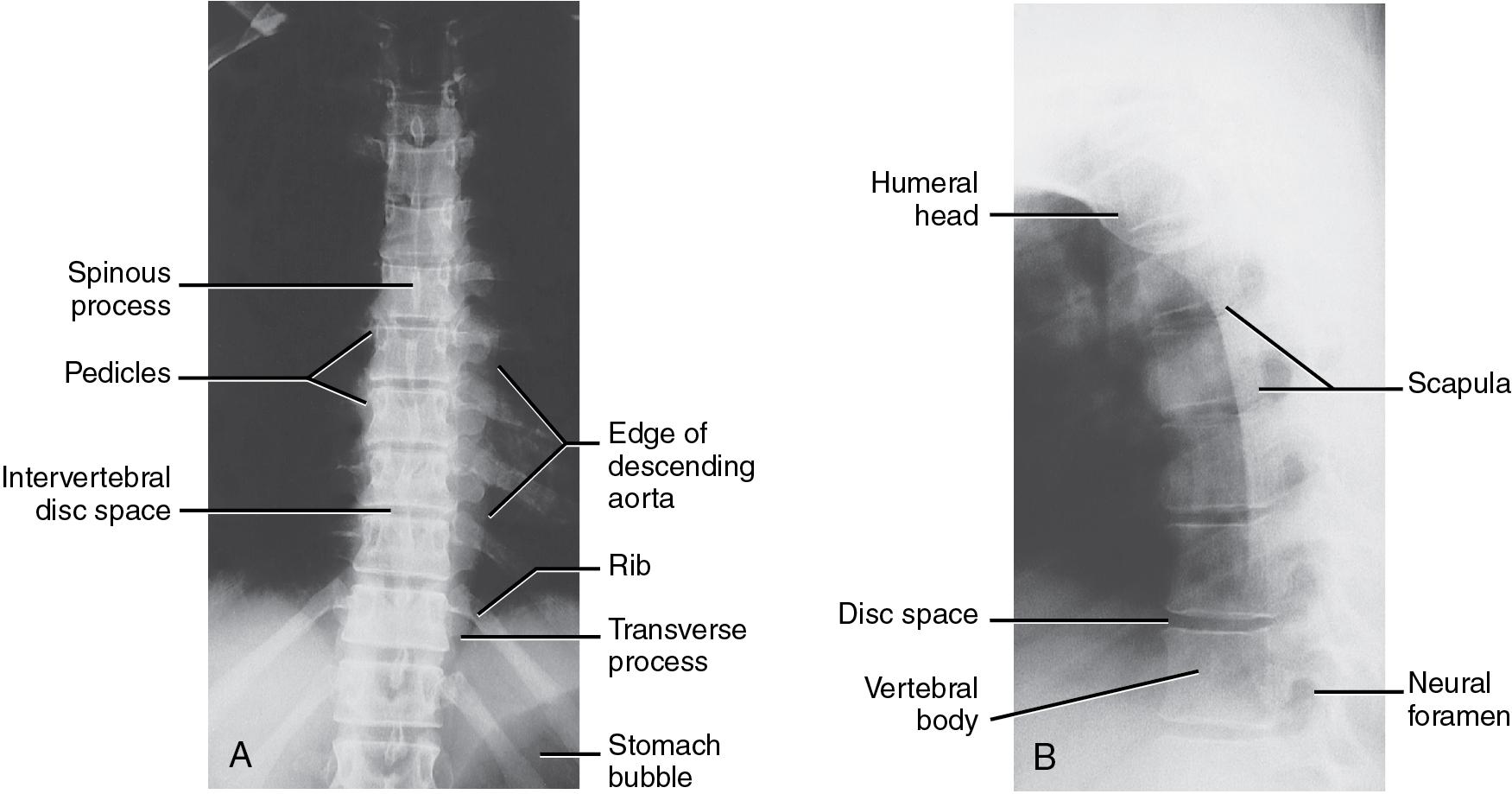
Standard thoracic spine views include an AP view and lateral view ( Fig. 9.4 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here