Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Radical prostatectomy is the “gold standard” in the surgical treatment of localized prostate cancer. Current evidence confirms a survival advantage over the absence of treatment in men with prostate cancer. Traditionally, radical prostatectomy was performed in the open retropubic or transperineal approach. The advent of minimally invasive techniques (pure and robot-assisted laparoscopy) allowing for improved visualization, has increased the understanding of prostate anatomy and surrounding structures and reduced the morbidity associated with radical prostatectomy.
In addition, over the last decade, the use of minimally invasive approaches has dramatically increased, particularly robot-assisted laparoscopic radical prostatectomy ( Fig. 66.1A ), which facilitates laparoscopic suturing.
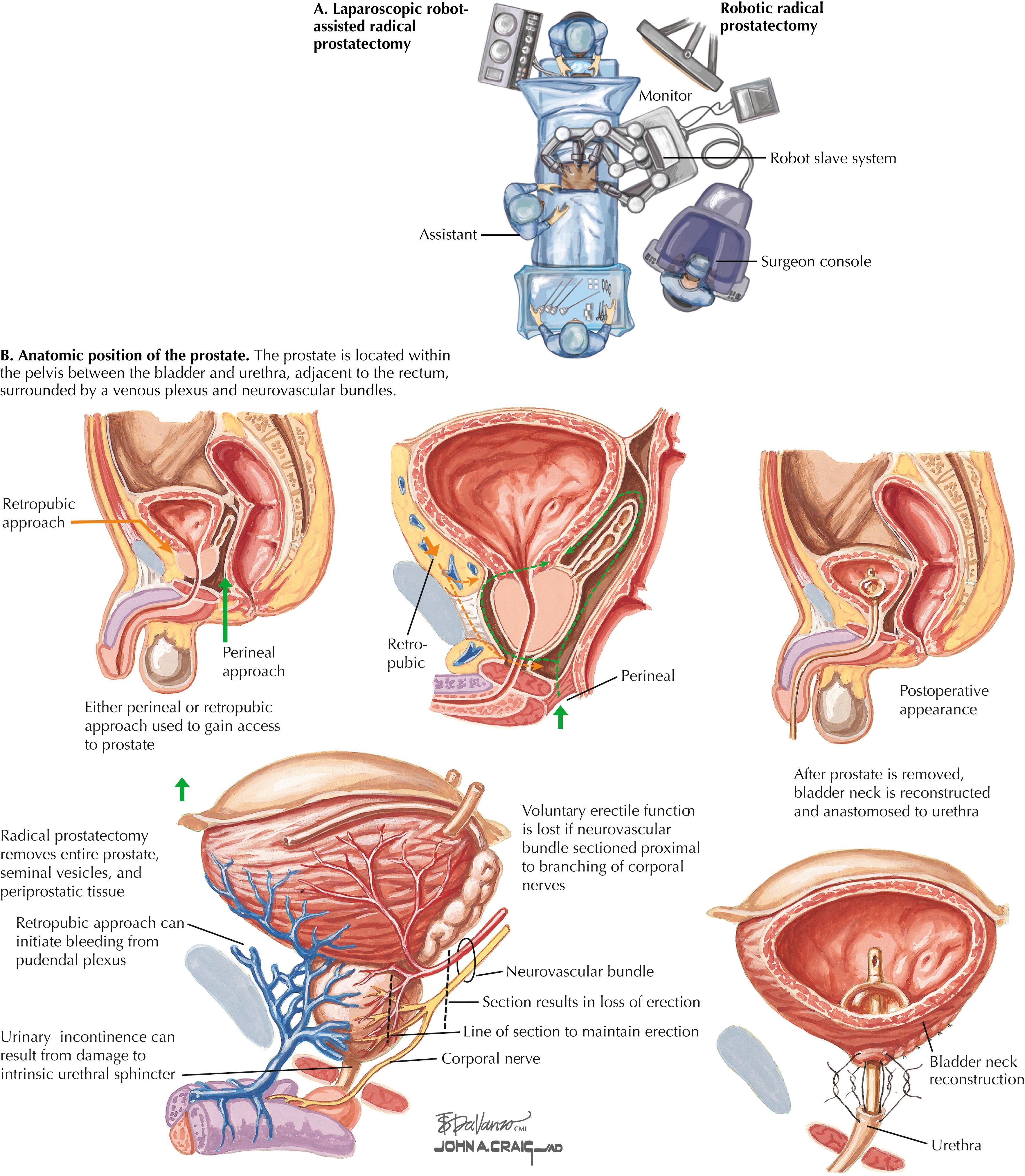
Prostatectomy can result in urinary incontinence and erectile dysfunction because of the damage to the urethral-sphincter complex and the periprostatic neurovascular bundles. Current 1-year data report that urinary continence is achieved in approximately 90% of patients, and erectile function is recovered in most men with good preoperative function.
Once the diagnosis of prostate cancer is made on biopsy, staging is obtained depending on the patient’s Gleason score, prostate-specific antigen (PSA), clinical stage, and life expectancy.
Staging can include pelvic computed tomography (CT) or, more recently, magnetic resonance imaging (MRI). A bone scan can be performed to exclude bone metastases. If the malignancy has a high probability of being localized to the prostate, treatment options are discussed with the patient, including active surveillance, radiation therapy, or surgery, depending on disease factors, life expectancy, and patient preference.
Radical prostatectomy is generally considered in men with life expectancy greater than 10 years who have prostate cancer at significant risk of progression. The variation in prostate size and shape, as well as its location deep in the pelvis between the bladder and the urethra and adjacent to the rectum, make surgical extirpation challenging ( Fig. 66.1B ). Additionally, the prostate is surrounded by a venous plexus and the neurovascular bundles responsible for erection. Therefore the surgical dissection required during radical prostatectomy should be performed meticulously by a surgeon with detailed knowledge of the anatomic relationships of the prostate.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here