Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Aortic regurgitation (AR), either acute or chronic, can be caused by valvular pathology, aortic root pathology, or a combination of the two. In developed countries, chronic isolated AR is predominantly caused by aortic root disease or congenital aortic valve disease, but rheumatic fever still remains the leading cause of chronic AR in developing countries. Surgery is frequently needed for patients with acute AR, and the timing of surgery for chronic AR depends on regurgitation severity, the patient’s symptoms, and left ventricular (LV) size and function. Therefore, accurate determination of cause and severity of AR is crucial when managing patients with AR. Semiquantitative and quantitative techniques should be used in an integrated fashion to assess the severity of AR.
Currently, Doppler color flow imaging is widely used to determine the severity of AR despite its limitations and semiquantitative nature. Parasternal long-axis, short-axis, and apical views can demonstrate the color Doppler recording of the AR well. Maximal length and area of the aortic regurgitant jet show poor correlation with aortic angiography. Short-axis jet area at the high left ventricular outflow tract (LVOT) relative to the LVOT area correlates well with angiography. The proportion of either jet area or jet width compared with LVOT area or width in excess of 65% indicates severe AR. , Although appealing, it is important to note that this method requires careful attention to gain settings and Nyquist limits to avoid over- or underestimating the severity of regurgitation. In general, this method only provides a rough estimate of the severity of AR. This method is of limited utility in patients with eccentric jets, diffuse jets, and jets originating along the entire coaptation line.
Both continuous-wave (CW) and pulsed-wave (PW) Doppler techniques are useful for the semiquantitative assessment of AR. Whereas dense CW Doppler signal implies greater quantity of regurgitation, faint signals generally represent mild regurgitation. Pressure halftime, the time for the pressure gradient to drop by half of its original value, is another measure of severity of AR obtained by CW Doppler. , It is expected that the pressure halftime is shorter (<200 msec) in patients with severe AR because of the rapid rise in LV pressure from a large amount of regurgitant volume (RV), especially in patients with acute AR. Conversely, in patients with mild AR, the pressure halftime is longer (>500 msec) because of a more gradual rise in LV pressure. Pressure halftime cannot be used alone to determine the severity of AR because it is dependent on chronicity of the regurgitation, systolic blood pressure, and LV compliance. For example, pressure halftime may be short because of underlying severe LV diastolic dysfunction. Another frequently used Doppler technique involves PW Doppler of the proximal descending thoracic aorta. Significant holodiastolic flow reversal in the descending thoracic aorta, diastolic velocity time integral similar to systolic velocity time integral, and relatively high end-diastolic velocity (>18 cm/s) are indicative of moderate to severe or severe AR ( Fig.88.1 and ![]() ). In some older patients, diastolic flow reversal is a less reliable indicator of the severity of AR because of a stiff aorta.
). In some older patients, diastolic flow reversal is a less reliable indicator of the severity of AR because of a stiff aorta.
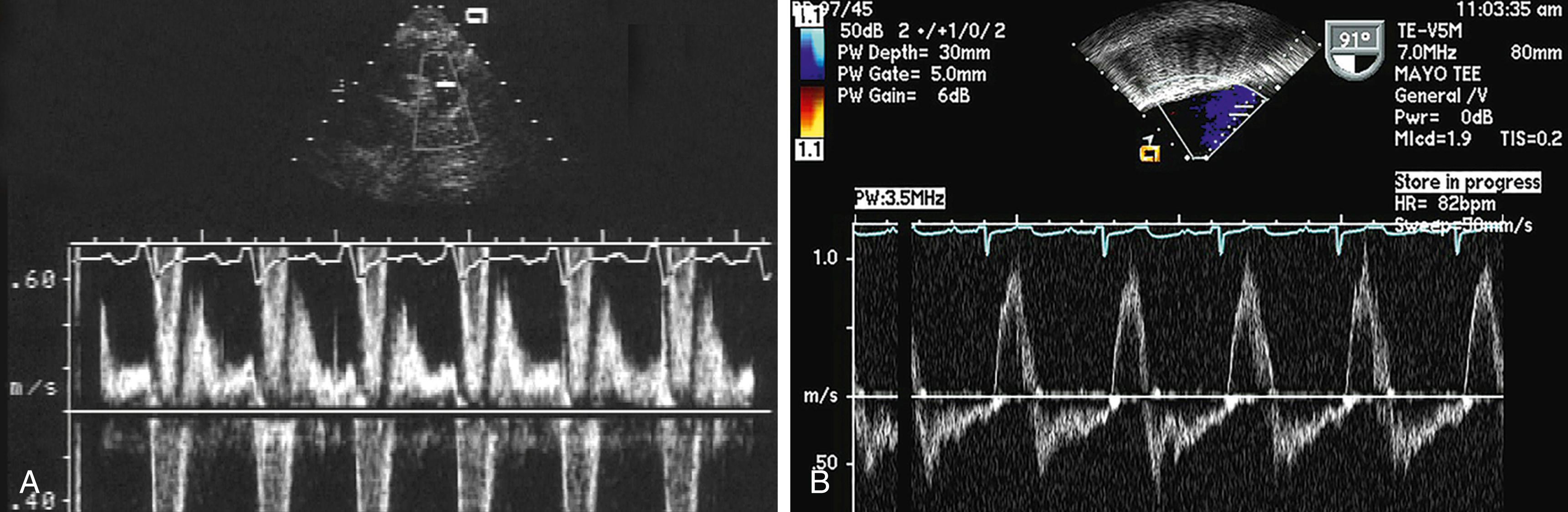
Video 88.1. Holodiastolic flow reversal in proximal descending thoracic aorta in a patient with severe aortic regurgitation.
It has been proposed that the smallest area of the aortic regurgitant jet hydrodynamically represents VC. From parasternal views, using the zoom function, one can visualize the proximal flow convergence zone, flow at the aortic valve, and flow below the aortic valve. In early to mid-diastole, VC is then measured, which is defined as the width of the narrowest portion of the aortic regurgitant jet that occurs immediately distal to the anatomic orifice. A VC width greater than 6 mm is indicative of severe AR with a sensitivity of 81% and specificity of 94%. In some patients, a right parasternal transthoracic window or transesophageal echocardiography (TEE) may be required to obtain adequate VC measurements ( Fig. 88.2 and ![]() ).
).
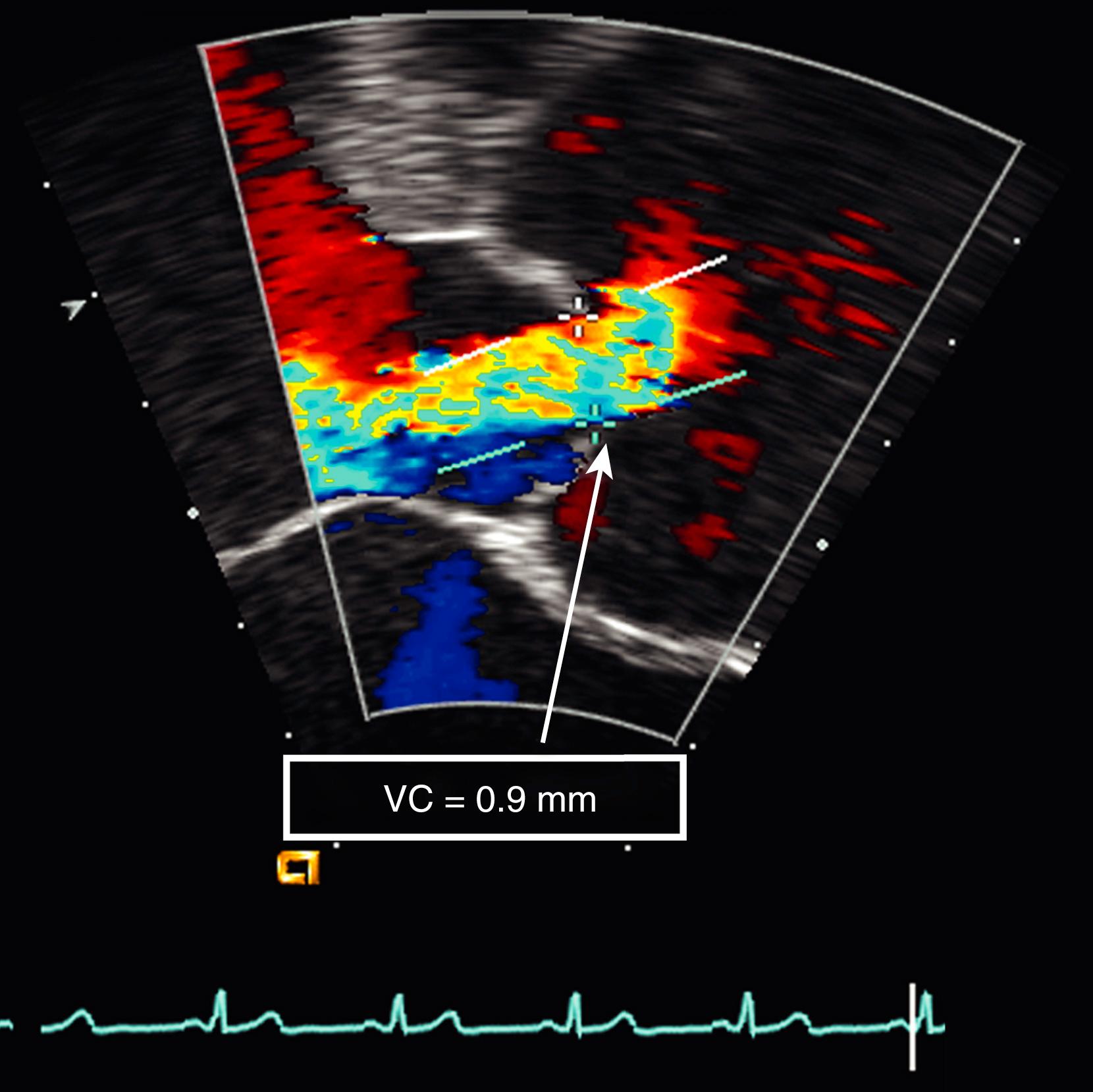
Video 88.2. Vena contracta (VC) width (9 mm) measurement in a patient with chronic severe aortic regurgitation on transesophageal study.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here