Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Trivial or mild degrees of pulmonic regurgitation (PR) are common in structurally normal hearts, and the presence of pathologic PR is rare in adults. Some degree of PR is present in between 5% and 78% in echocardiograms of patients with normal pulmonic valves (PVs) and structurally normal hearts. Echocardiographic evaluation of the degree PR is much less well defined than for the other heart valves and is either descriptive or semiquantitative. This is primarily because of the low prevalence of clinically severe PR. In one series, only 1.6% of all severe valvular regurgitation was caused by PR.
As with other valve lesions, assessment of PR includes three basic elements: (1) establishing the mechanism of PR, (2) determining the severity of PR, and (3) assessing the impact of PR on cardiac chambers, primarily the right ventricle (RV) and the pulmonary artery (PA). Whereas the severity of PR is best assessed by Doppler echocardiography, the mechanism of PR and its impact on cardiac chambers is evaluated by two- and three-dimensional echocardiography (2DE and 3DE, respectively).
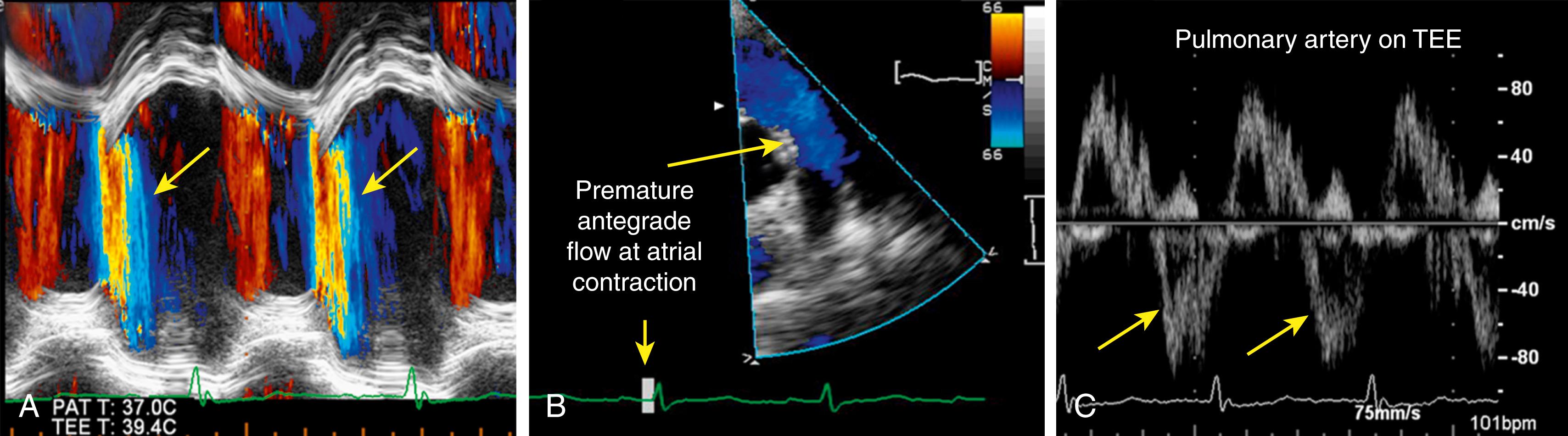
The American College of Cardiology and the American Heart Association guidelines on valvular heart disease address the issue of PR only briefly. The American Society of Echocardiography recommendations for evaluation of severity of PR include evaluation of anatomical structure of the pulmonary valve, right ventricular (RV) size, color Doppler pulmonic regurgitant jet size, spectral Doppler jet density, duration, and deceleration rate as well as a comparison echocardiography and magnetic resonance imaging in PR diagnosis. Other parameters of PR severity include timing of tricuspid valve (TV) closure and PV opening, holodiastolic flow reversal in the PA, low peak velocity of PR jet, and laminar retrograde flow. Echocardiographic markers of PR severity are summarized in Table 107.1 and shown in Figs. 107.1 and 107.2 .
| Parameter | Moderate to Severe PR | Severe PR | |
|---|---|---|---|
| Color Doppler | Jet length and area | Increased | May be short |
| Jet turbulence | Turbulent jet | Laminar jet | |
| Vena contracta | Wide | Very wide | |
| CW Doppler | Jet density | Dense | Very dense |
| Deceleration slope | Short | Very short | |
| Premature cessation of retrograde flow | May be absent | Typically present | |
| To-and-fro flow | Absent | Present | |
| Peak PR velocity | Normal | Low | |
| Premature opening of the pulmonic valve | Absent | Present | |
| Premature closure of the tricuspid valve | Absent | Present | |
| PW Doppler | Regurgitant volume | <60 mL/beat | ≥60 mL/beat |
| Regurgitant fraction | <50% | (50% | |
| Holodiastolic flow reversal in PA | Absent | Present | |
| Additional Signs | RV and PA size | Progressively increases with the severity and chronicity of PR | |
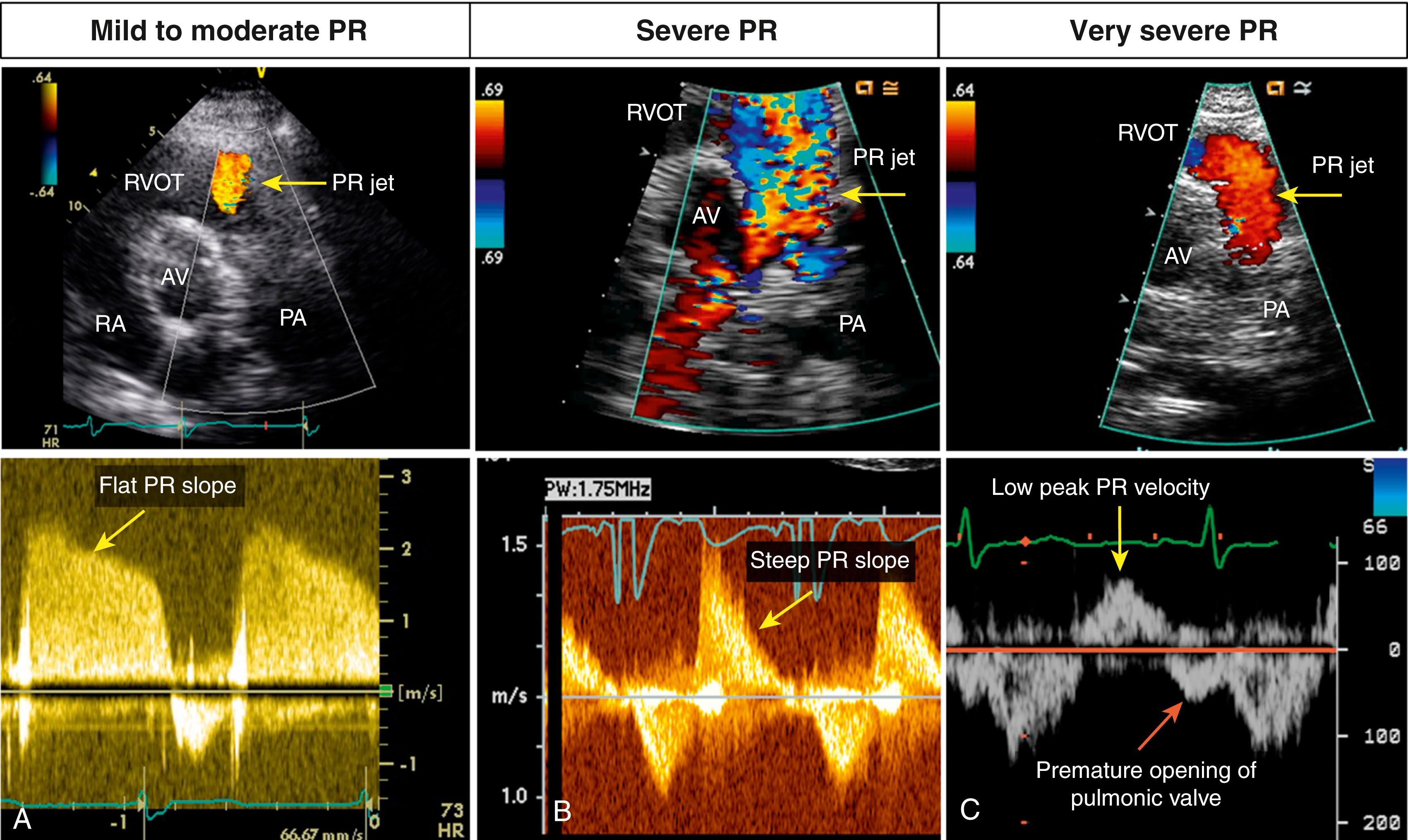
Video 107.1. Color and spectral Doppler markers of pulmonic regurgitation (PR). Transthoracic short-axis view at the level of the aortic valve demonstrate color Doppler (top) and spectral Doppler (bottom) findings in mild to moderate, severe, and very severe PR. A. Mild to moderate PR . On color Doppler, the jet is small (arrow) , and vena contracta at the jet origin is narrow. On spectral Doppler, the slope of PR jet is relatively flat (arrow) . B, Severe PR. On color Doppler, the jet is large and turbulent (arrow) , but on spectral Doppler, the PR slope is steep (arrow) . C, Very severe PR. On color Doppler, the jet is laminar (arrow) and of short duration. On spectral Doppler, there is a low peak velocity of PR jet (yellow arrow) , and there is premature opening of pulmonic valve with abnormal antegrade flow in late diastole. AV, Aortic valve; RA, right atrium; RVOT, right ventricular outflow tract.
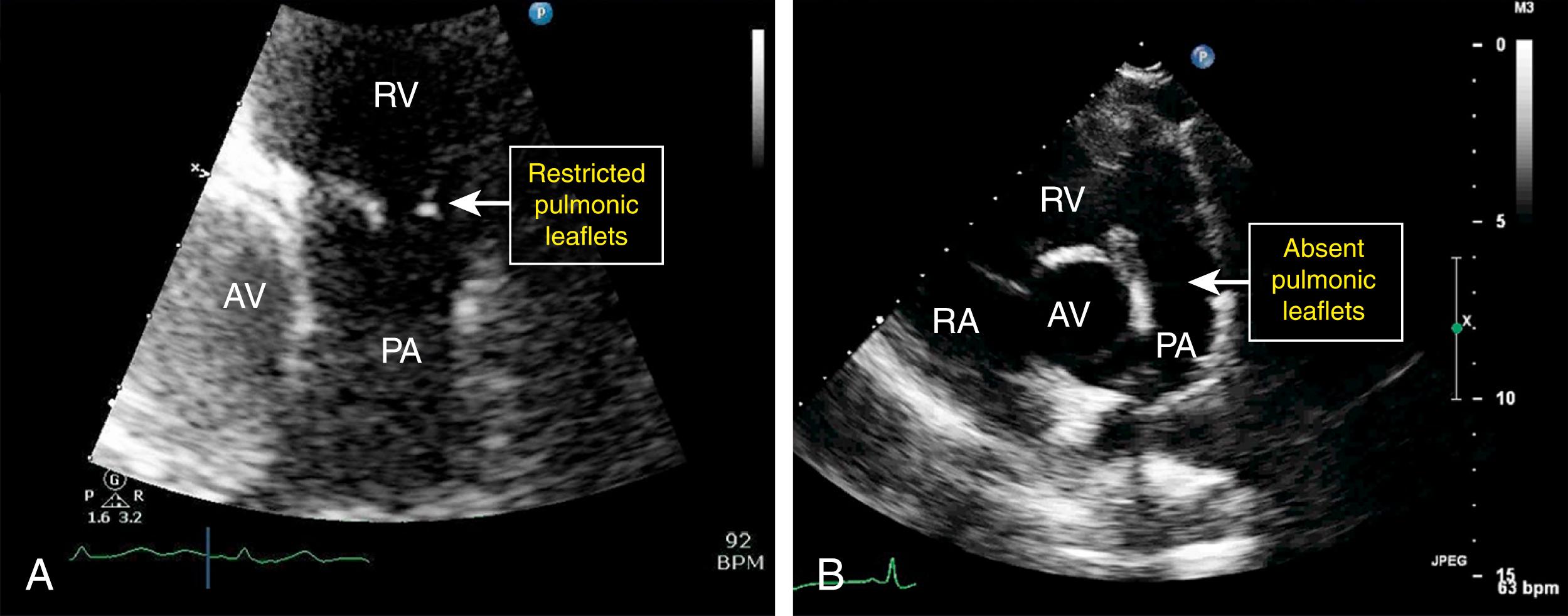
A normal pulmonary valve is semilunar, trileaflet valve located anterior, superior, and slightly to the left of the aortic valve. The valve leaflets are very thin and highly pliable, making the PV the most challenging valve to image. In addition, visualization of the PV is often limited because only one or two posterior leaflets are imageable. Moreover, because of rapid opening, the leaflets are difficult to visualize in systole. PR can be either congenital or acquired. The most common causes of severe PR included carcinoid disease and status post surgically repaired pulmonic stenosis of tetralogy of Fallot ( Fig. 107.3 ). Endocarditis rarely affects the native PV. Box 107.1 lists the majority of causes of PR.
Pulmonary hypertension (dilatation of the pulmonary artery)
Congenital (e.g., bicuspid or quadricuspid)
Status post pulmonic valvotomy (surgical or balloon)
Rheumatic heart disease
Infective endocarditis
Marfan syndrome
Carcinoid (stenosis or regurgitation)
Trauma (including injury from a pulmonary artery catheter)
Video 107.3. Causes of severe pulmonic regurgitation (PR). A, Carcinoid disease of the pulmonic valve. B, Severe PR occurring decades after surgical repair of tetralogy of Fallot. AV, Aortic valve; PA, pulmonary artery; RA, right atrium; RV, right ventricle.
The primary mechanisms of PR include distorted or absent leaflets, annular dilatation, or both. When assessing PR, it is best to evaluate the right ventricular outflow tract (RVOT), PV, and PA together. Imaging of the PV is often better by transthoracic echocardiography (TTE) than transesophageal echocardiography (TEE) given the anterior location of the valve, which is in the far field by TEE. 2D TTE and TEE imaging typically allows for visualization of only long-axis views of the PV. On TTE, PR is best visualized on the parasternal short-axis view at the level of the aortic valve and from the subxiphoid view. On TEE, the PV and PA can be imaged in the midesophageal and transgastric views using approximately the 60-degree acquisition angle. The short axis of the PV can be obtained by 3D TTE and TEE imaging.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here