Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
As early detection and treatment of breast cancer have improved, survival rates have increased to the extent that 89% of individuals with breast cancer now survive 5 years beyond diagnosis, and 83% of individuals survive at least 10 years. The majority of women are diagnosed with early-stage cancer localized to the breast, and the 5-year survival rate for this group is 99%. There are over 3.5 million breast cancer survivors in the United States, two-thirds of who have been or are being treated with endocrine therapy (ET). In 2020 an estimated 276,480 new cases of invasive breast cancer were diagnosed in women in the United States. The diagnosis of breast cancer generates significant distress in the lives of patients and their families because cancer is often considered synonymous with death, pain, and suffering. The first section of this chapter provides an overview of methods to assess distress in individuals with breast disease throughout the continuum of the disease and provides an overview of options for psychosocial intervention with special attention to certain groups of patients. The second section of the chapter examines lifestyle interventions, a growing area of investigation for breast cancer patients, survivors, and women at risk for the disease. This section provides an overview of the rationale behind studying the impact of lifestyle factors on breast cancer risk and prognosis, summarizes the interventional studies in this area, and highlights future research directions.
Distress is defined as a multifactorial unpleasant emotional experience of a psychological (cognitive, behavioral, emotional), social, and/or spiritual nature that may interfere with the ability to cope effectively with cancer, its physical symptoms, and its treatment. Distress extends along a continuum, ranging from common normal feelings of vulnerability, sadness, and fears to problems that can become disabling, such as depression, anxiety, panic, social isolation, and existential and spiritual crisis. All patients experience some level of distress associated with the diagnosis and treatment of cancer at various stages of the disease. In 2004 the Canadian Strategy for Cancer Control designated emotional distress as the sixth vital sign to highlight the importance of distress as a marker of well-being and its reduction as a target outcome measure.
Research has demonstrated that, across the trajectory of the illness (from the time of diagnosis through treatment, termination of treatment, survivorship, or recurrence and palliation), the incidence of emotional distress in people diagnosed with cancer ranges from 35% to 45%. Evidence suggests that, among women undergoing breast cancer treatment, psychological distress is associated with adverse physical symptoms such as pain, fatigue, and nausea. In some studies, elevated distress has also been linked to poorer health outcomes such as higher mortality, greater morbidity, nonadherence to treatment, and poorer immune function. Furthermore, other outcomes such as medical expenditures and occupational functioning may be adversely affected in patients experiencing serious psychological distress. Addressing distress may affect outcomes; a recent Cochrane review determined that psychological interventions were effective in improving survival at 12 months in metastatic breast cancer. Additionally, there is evidence that early intervention in treating depression and anxiety can improve treatment adherence and reduce medical costs by 25%. Many other studies have been conducted to examine the efficacy of distress screening in improving patient outcomes. A recent systematic review showed that 17 of the 24 studies reviewed reported statistically significant benefits of distress screening on outcomes such as quality of life (QOL), distress, and patient-clinician communication.
In 2007 the Institute of Medicine (IOM) report Cancer Care for the Whole Patient stated that the failure to address the very real psychosocial health needs of cancer patients and their caregivers is a failure to effectively treat that patient’s cancer. The IOM report supported the National Comprehensive Cancer Network (NCCN) Distress Management guidelines first released in 1999 and most recently updated in 2022. The American College of Surgeons Commission on Cancer (CoC) echoed the importance of psychological distress screening and required cancer centers to implement screening programs for psychosocial distress by 2015 in order to acquire or maintain accreditation.
Unfortunately, despite the documentation that distress occurs, and the benefit of timely psychological intervention, the initial assessment of a patient’s distress is often delayed or goes unnoticed by oncology professionals. In 2013 a study showed that less than half of the 70 CoC-accredited institutions surveyed had begun distress screening. Another study found that compliance with the Distress Screening guidelines varied across clinics, with 47% to 73% of eligible patients being screened at least once during their treatment. In response, the American College of Surgeons’ CoC, the primary accrediting body for up to 1500 cancer treatment programs serving roughly 70% of cancer patients in the United States, established new accreditation standards for patient-centered care, including Standard 3.2, which mandates that all patients be screened for distress and that an appropriate clinical response be provided when patients are identified as distressed. Barriers to screening included lack of buy-in among key cancer center staff including oncologists, lack of training on how to implement screening, discomfort with the amount of time required to address concerns, and lack of competence on how to refer patients when significant distress was identified. Other issues include budget and availability of appropriate support staff.
Although traditional psychosocial services are available on a referral basis from the health care team, these referrals are commonly made only when a patient reaches a crisis. This type of reactive approach may jeopardize the patient’s relationship with the health care team, as well as effective participation in treatment. At a minimum, psychosocial screening can provide the opportunity to identify and predict which patients are more at risk for distress and are more unlikely to adapt to the many stressors associated with a cancer diagnosis and its treatments.
The NCCN standards for managing distress suggest that all patients should be screened to ascertain their level of distress at the initial visit, at appropriate intervals, and as clinically indicated, especially when changes occur in disease status (remission, recurrence, progression, or treatment-related complications). Several identified risk factors may place an individual at increased risk for distress, and these factors should be assessed during the initial evaluation. Risk factors for distress include younger age, female gender, living alone, having young children, lower education level, severe comorbid disease, experiencing uncontrolled symptoms, having other sources of stress, history of psychiatric disorder or depression, cognitive and/or communication barriers, and a history of alcohol or substance abuse.
Oncology clinicians often fail to recognize patient distress in clinical encounters, underscoring the need for standardized screening methods. Various tools exist to screen for distress in cancer patients. These include the distress thermometer (DT), the Hospital Anxiety and Depression Scale (HADS), , and the Brief Symptom Inventory (BSI). Only a few instruments have been developed specifically for breast cancer patients. These include the Breast Cancer Chemotherapy Questionnaire (BCQ), the Functional Assessment of Cancer Therapy—Breast (FACT-B), and the European Organization for Research and Treatment of Cancer core questionnaire and breast module (EORTC QLQ-C30/+BR23). The FACT-B and the EORTC QLQ-C30/+BR23 were designed for use in breast cancer patients in a wide range of disease stages undergoing different treatments, to detect clinically meaningful changes in QOL over time. Both the FACT-B and the EORTC QLQ-C30/+BR23 combine a generic core questionnaire with site-specific modules that have been internationally validated. These instruments do take time to complete and interpret, and therefore they are not useful for screening for distress in a busy clinical setting.
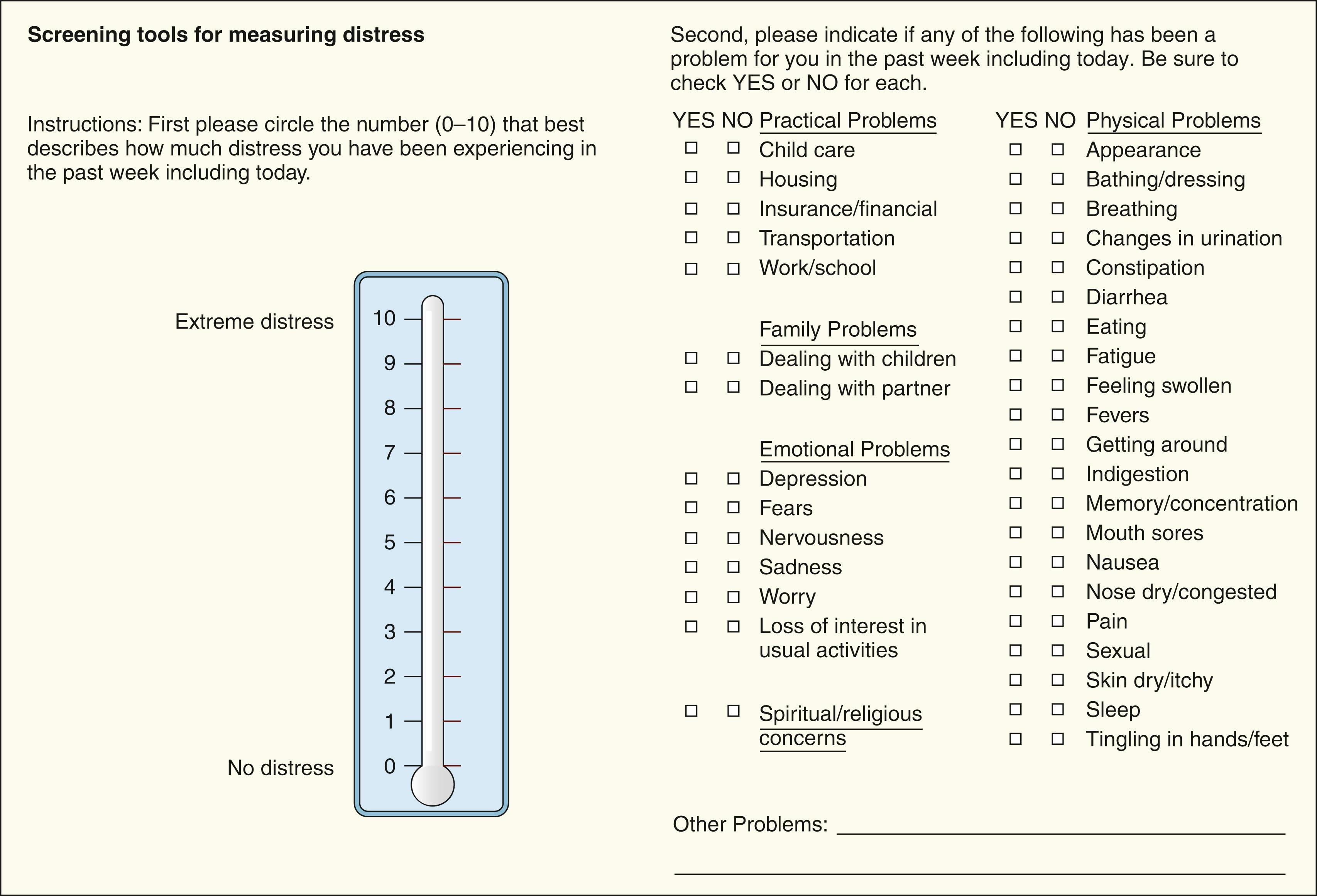
The DT ( Fig. 79.1 ) is a one-item, self-reporting, nonstigmatizing tool that is easy both to administer and to score and interpret; it is endorsed by the NCCN Distress Management guidelines for use in all oncology settings. The DT is a thermometer-like Likert scale that asks the patient to circle the number (0 = no distress and 10 = extreme distress) that best describes how much distress the patient has been experiencing in the past week, including that day. A level of 4 or higher signifies clinically significant distress and warrants a member of the oncology team performing a review of the problem list and conducting an evaluation to identify and execute appropriate referrals. Distress levels lower than 4 may be mild, and the oncology team may choose to address those through usual supportive care in the clinic.
DT has been tested against the Patient Health Questionnaire depression module (PHQ-9) and was found to be an effective tool for detecting depression in newly diagnosed breast cancer patients in a clinical setting. Table 79.1 includes some examples of screening instruments that have been validated and are applicable to individuals with cancer.
| Instrument Name | Dimensions Assessed | Score Range | Score Warranting Intervention | Comments |
|---|---|---|---|---|
| Distress Thermometer (DT) | Distress | 0–10 | ≥4 | Developed by the NCCN Distress Management Panel. Administered with a problem list covering various aspects of a patient’s life. |
| Patient Health Questionnaire-4 (PHQ-4) | Depression, anxiety | 0–12 (0–6 for each subscale) | ≥3 in either scale | Combination of two-item depression (PHQ-2) and two-item anxiety (GAD-2) scale. Grades symptom burden as mild (3–5), moderate (6–8), or severe (9–12). |
| General Health Questionnaire (GHQ-12) | Current mental health | 0–36 | ≥5 | Abbreviated from the original 60-question version. Focuses on two major areas: the inability to carry out normal functions and the appearance of new and distressing experiences. |
| Hospital Anxiety and Depression Scale (HADS) | Depression, anxiety | 0–42 (0–21 on each subscale—anxiety and depression) | ≥14 on total scale. ≥11 on HADS-Depression and ≥11 on HADS-Anxiety. | Widely used and validated by many studies. Total score indicates general distress. |
| Brief Symptom Inventory-18 (BSI-18) | Global Severity Index (GSI); subscales: Depression, Anxiety, Somatization | 0–72 | Total score ≥63, score ≥50 for cancer survivors | Based on Symptom Checklist-90—Revised (SCL-90-R) and BSI-53, which have additional domains. |
Although hereditary breast cancers make up only a small proportion of all breast cancer cases, those individuals who do carry the BRCA mutation often experience significant amounts of distress related to their risk of developing breast cancer. Genetic risk assessment can be a complex process for patients and their families, involving different stages, including extended counseling, specialist screening, and genetic testing for mutations. Although most people undertaking cancer genetic risk assessment do so with minimal emotional sequelae, approximately 25% report high levels of distress during the process of risk assessment and gene testing. Factors that may predict distress during this process include the anticipation of future problems after a positive test outcome such as the consideration of prophylactic surgery (mastectomy and/or salpingo-oophorectomy) and being a carrier of a mutation. Additionally, being pessimistic, being less than 50 years of age, having many relatives with breast or ovarian cancer, having a parent pass away from cancer, and having high levels of baseline anxiety are predictors of distress.
For women who test positive or negative for the BRCA1/2 mutation and who do not have a strong family history, the interpretation of the results and subsequent recommendations are well defined. Women who have a family history of breast cancer and test negative for a BRCA1/2 mutation receive an uninformative negative result because, although they know that BRCA1/2 has not caused breast cancer in their family, this does not mean that they have the same risks as the general population. Accumulated data on associations between distress and actual BRCA1/2 testing have been mixed. A recent study showed that BRCA1/2 mutation carriers with known maternal transmission and whose mothers were deceased report higher perceived stress and anxiety, lower QOL, and bereavement scores correlated with psychological measures. Conversely, a review of the literature concluded that, in individuals with no personal cancer history, BRCA1/2 carriers are not adversely affected, and noncarriers may even derive some psychological benefits from the test results.
In addition to distress concerning genetic testing, women who are found to carry BRCA1/2 mutations are also faced with decisions regarding prophylactic surgery. Because prophylactic surgery is an irreversible procedure that is performed in healthy high-risk women on parts of the body that are conceivably related to self-image and sexual attractiveness, emotional distress can be expected. Compounding this distress is the belief among some patients that prophylactic surgery must be done quickly after the presence of a BRCA1/2 mutation is discovered.
Another aspect of genetic testing is direct-to-consumer genetic testing in which patients and relatives are able to test for underlying mutations directly through the company. There is concern that, without involvement of a health care professional, positive results from these tests may cause further distress. However, a recent survey showed that, even when patients received unexpected positive results, they did not report extreme anxiety; some patients experienced moderate anxiety, but this was transient. Positive tests, however, led to these subjects seeking medical attention, undergoing prophylactic surgeries, and encouraging other family members to undergo screening.
The process of detecting and diagnosing breast cancer often creates a great deal of uncertainty and anxiety among women. This distress often begins as early as an abnormal screening mammogram. Several studies have shown that an abnormal screening result causes significant increases in anxiety associated with waiting for the next test and its results. The way a patient is informed of an abnormal screening is an important factor in the patient’s emotional response. Pineault found that women who were more satisfied with the information provided to them by clinicians experienced less anxiety while waiting for their next tests and results. Providing patients with adequate information about their results is important not only to help alleviate anxiety but also to increase adherence to follow-up appointments. In a study of follow-up after abnormal screening mammograms among low-income minority women, Allen and coworkers found that many women did not even realize their results were abnormal. Some women stated that they thought a “positive finding” was good news and that they did not understand the need for a second mammogram after just having their routine one.
Breast biopsy, the next step of the diagnosis process, provides the only definitive diagnosis for breast cancer. In the United States, more than 1.6 million breast biopsies are performed annually, and approximately 80% of these findings are benign. This was much less during the COVID-19 pandemic because of the 85% reduction in screening. Uncertainty regarding the potential diagnosis results in distress that can interfere with the ability to obtain necessary health care. Patients have reported that they postponed follow-up appointments in fear of receiving a cancer diagnosis. If diagnosed with cancer, distress related to the biopsy can increase postoperative discomfort, impair decision-making ability, and lower immune function. Research has shown that the anxiety continues through the peridiagnostic period; women with a benign diagnosis reported lingering anxiety regarding continued detection practices. Unfortunately, many of these biopsies are ordered by primary care providers who do not have sufficient resources to screen women or educate them before such procedures, and distress often goes unrecognized and untreated by the health care team. Similar to the mammography process, women who are adequately informed about their cancer risk and the tests they are undergoing have been found to experience less distress, cope better with the possibility of having cancer, participate in decision-making, and have a greater trust in the health care team.
Cancer patients commonly report feeling overwhelmed at the time of diagnosis. For individuals with breast cancer, the first year after a breast cancer diagnosis is accompanied by intense challenges that cut across the physical, psychological, social, and spiritual domains of life. There are several stressors throughout the illness trajectory: awaiting diagnosis, anticipating the outcome of metastatic evaluations, surgery, adjuvant therapy, coping with side effects, and facing the risk of recurrence. The period immediately after diagnosis is usually filled with complex decision-making for primary therapy and, for many women, adjuvant therapy that will take place over the ensuing 4 to 6 months. During this time, there may be an increased sense of vulnerability, confusion, uncertainty, loss of control, and existential concerns. This is often exacerbated by inadequate information, scheduling conflicts with various providers (surgeon, medical oncologist, radiation oncologist, plastic surgeon), and the need to make decisions based on the recommendations of a new team of physicians and caregivers.
Women with early-stage breast carcinoma generally have the choice of three equally effective surgical options: breast-conserving surgery (BCS), mastectomy, or mastectomy with reconstruction. Although BCS as an alternative to mastectomy has gained popularity with time and has become the standard of care for many patients with T1 and T2 tumors, mastectomy is still a commonly used procedure. Several factors influence which procedure a woman decides to undergo, including the perceived chance of survival; concerns about breast loss, local tumor recurrence, and radiotherapy; and the patient’s perception of the surgeon’s preference. Although numerous studies have evaluated QOL among women who undergo BCS, mastectomy, or mastectomy with reconstruction, a meta-analysis of the literature revealed that no single procedure has been clearly demonstrated to provide a better QOL. Recent studies have found that patients who make informed decisions based on their personal beliefs, values, and expectation are more likely to be satisfied postsurgery. Women who were dissatisfied with the information provided in the decision-making process were more likely to experience surgery decision regret. Additionally, women who felt that their role in the decision-making process met their desired role were more likely to be satisfied with the decision, regardless of the procedure.
Adjuvant treatments including radiation therapy, chemotherapy, and antiestrogen therapies generate additional physiologic and psychological difficulties that further affect body image, sexuality, and family. Acute adverse reactions and symptoms associated with each treatment can significantly challenge patients. Chemotherapy causes an array of symptoms including fatigue, nausea and vomiting, skin changes, and alopecia. A meta-analysis found that alopecia is often listed as one of the top three important side effects of chemotherapy among breast cancer patients and describes their hair loss as a traumatizing event. Although there have been dramatic improvements in the supportive care and management of many symptoms, alopecia and fatigue can exacerbate the negative effects that treatment has on body image and overall QOL. Women taking aromatase inhibitors (AIs) often report musculoskeletal symptoms, vaginal dryness and pain with intercourse, and increased cognitive problems ; because the duration of ET varies and can be up to 10 years in some cases, these side effects can be long-term.
Breast cancer survivors constitute 22% of the estimated 14.5 million cancer survivors in the United States. Because an increasing number of breast cancer patients are now either cured of their disease or live for many years with it, they face the complex process of adjusting to life long after cancer treatment ends. The first year after primary treatment, the “reentry” phase, is characterized by physical, emotional, and social recovery. Women report high unmet care needs and have to cope with lingering physical and emotional symptoms of treatment, fear of recurrence, decreasing social support, losing the safety net of care providers, and resuming professional and recreational activities. Cancer is a disease that can substantially affect several physical and psychological aspects of the survivor’s life years later. Many patients report heightened anxiety leading up to regular checkups or follow-up tests (e.g., mammograms, tumor markers, bone scans) that may uncover a recurrence of the cancer. Patients may also report hypervigilance to physical changes or minor aches and pains; this may be especially pronounced when medical monitoring becomes increasingly less frequent.
Zampini and Ostroff identified four critical life domains in which cancer survivors may experience challenges: physical health, psychological and social well-being, maintenance of adequate health insurance coverage, and employment. Many survivors actively strive to meet these challenges by maintaining their physical health through preventive regimens of diet, exercise, stress reduction, and smoking cessation. These activities restore some sense of control to the cancer survivor in the realm of physical health. The psychological and social well-being of survivors may be challenged on a number of fronts, including frustration with the constant intrusion that residual symptoms and follow-up visits have on their lives and their desire to move forward and return to a normal life.
The maintenance of adequate health coverage is very important, and survivors often worry about the threat of policy cancelations or reductions in coverage. Furthermore, the link between employment and insurance in the United States creates difficulties for survivors who feel compelled to retain their current employment rather than risk the possibility of losing their health care coverage. There may also be issues related to job opportunities, promotions, negative attitudes toward cancer from coworkers or supervisors, and the possibility of dismissal because of poor performance or absenteeism related to residual symptoms or ongoing surveillance appointments.
Cancer recurrence or progression presents a somewhat different set of challenges for patients and health professionals. After breast cancer therapy, QOL suffers severely, with most women having erroneous perceptions of their breast cancer risk, leading to long-term concern as a result of these perceptions. Younger age, higher level of education, and female gender have been associated with increased fear of recurrence. The fear of recurrence is common and associated not with the actual risk of recurrence but with the perception of risk.
When disease recurs, the emotional trajectory for women with recurrent disease is somewhat unclear, and there are discrepancies in the current literature regarding psychosocial outcomes. Some studies report that recurrence among survivors increases distress, and other studies report that it does not. These discrepancies may be attributed to several factors, including variance in the measures used, the control group used, the time since recurrence, and the nature of the recurrence. Patients with metastatic disease may experience more distress than those with local cancer recurrence (i.e., recurrent disease on the chest wall after mastectomy). Psychosocial responses to cancer recurrence include depressive symptoms, such as the loss of hope for recovery, anxieties and fears of death, and difficulties with disability. Specifically, Brothers and Anderson found that high levels of hopelessness after a breast cancer recurrence were predictive of increased depressive symptoms. Other issues may include uncontrolled pain, appetitive difficulties, and poor body image.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here