Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Updated chapter based on the previous edition, written by Andrew Green and Tom R. Norris.
The shoulder has the widest range of motion (ROM) in the human body, allowing for positioning of the upper extremity in a variety of directions. This adaptation from a weight-bearing limb to working “instrument” is crucial for humans, and as a consequence, any impairments of shoulder function may reduce the quality of life and cause dramatic socioeconomic effects.
Glenohumeral dislocations and proximal humeral fractures are the most frequent traumatic injuries of the shoulder girdle and include a broad range of clinical problems. Although some injuries are recognized early and treatment options clearly defined, other injuries and conditions sometimes present significant treatment challenges. Sometimes injuries seem to be only of minor character and tend to be neglected. This leads to a significant delay until the necessary diagnostics and treatment are introduced, causing suboptimal or poor outcomes. Shoulder girdle injuries in the polytrauma setting present additional challenges because other musculoskeletal injuries often take precedence. A comprehensive multidisciplinary approach to an injured patient requires recognition of the critical importance of restoration and preservation of shoulder girdle function after traumatic injury.
The goal of this chapter is to review the relevant anatomy, biomechanics, epidemiology, classifications, evaluation, management, complications, and outcomes of treatment of acute glenohumeral dislocations and proximal humeral fractures and fracture-dislocations.
To comprehend the pathologic changes caused by proximal humeral fractures and fracture-dislocations and glenohumeral dislocations, it is important to understand the developmental and normal adult anatomy of the glenohumeral joint.
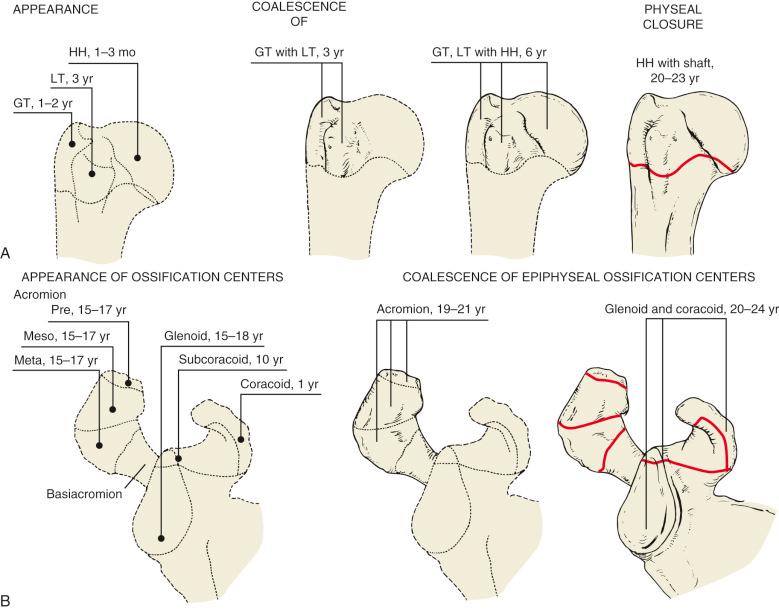
The proximal part of the humerus develops from three centers of ossification. The epiphysis of the central articular segment of the humeral head forms within 4 to 6 months after birth. The epiphysis of the greater tuberosity forms at approximately 3 years, and that of the lesser tuberosity forms by 5 years of age. The three centers of ossification coalesce between 4 and 6 years of age and fuse with the humeral metaphysis between ages 20 and 23 years ( Fig. 47.1 ). At birth, the glenoid cavity is cartilaginous, developing a center of ossification in its upper third (subcoracoid) between 10 and 11 years of age (see Fig. 47.1 ). Furthermore, an epiphyseal plate appears for the lower part of the glenoid cavity between ages 15 and 18 years. The fusion of the two centers of ossification is usually completed at 25 years of age.
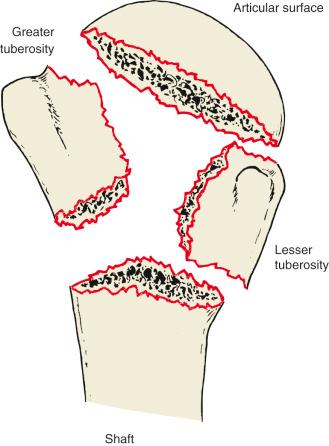
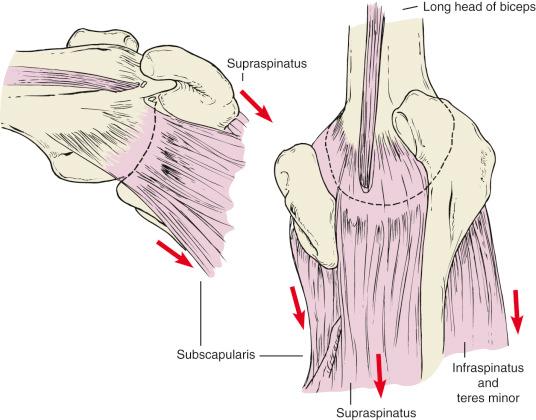
Codman recognized that proximal humeral fractures in adults occur along the lines of the old physeal scars, with injury patterns involving the four segments ( Fig. 47.2 ). These segments include the articular segment; the lesser tuberosity with the subscapularis attached; the greater tuberosity with the supraspinatus, infraspinatus, and teres minor tendons attached at their respective facets; and the shaft of the humerus.
The mean humeral head retrotorsion ranges from 18 to 30 degrees (total range is 10 to 55 degrees) relative to the epicondylar axis of the distal end of the humerus. The plane of the glenohumeral joint is approximately 30 degrees anterior to the coronal plane. The average adult humeral head has a radius of curvature of 22 to 25 mm. The most cephalad surface of the articular segment is on average 8 mm above the greater tuberosity. The size of the humeral head determines the lateral displacement of the greater tuberosity and the rotator cuff insertions and has an effect on the kinematics of the glenohumeral joint. These anatomic parameters have important implications for imaging, repair and reconstruction, and rehabilitation of the shoulder girdle. Anatomic alterations that accompany proximal humerus fractures can lead to major disruptions in shoulder motion and function.
The glenoid labrum surrounds the periphery of the glenoid. Histologically, the labrum is a transitional structure between the hyaline articular cartilage of the glenoid and the fibrous glenohumeral capsule. It is predominantly fibrous except at its attachment to the glenoid rim, where it is fibrocartilaginous. The labrum becomes fibrous as it blends into the capsule. The superior aspect of the labrum is intimately associated with the tendon of the long head of the biceps brachii. The glenohumeral ligaments are variably attached to the labrum. The labrum increases the depth of the glenoid fossa by about 50%.
The glenohumeral joint has the greatest ROM of any joint in the body. The loose ligaments that allow this motion also provide a passive restraint against instability. They are primarily effective at the extremes of glenohumeral motion. Unlike the discrete ligamentous structures of other joints, the glenohumeral ligaments represent thickenings within the capsular tissues. The most important of these structures is the inferior glenohumeral ligament (IGHL) complex, with anterior and posterior bands on either side of an axillary pouch. The anterior band travels from the humeral neck inferiorly up along the anterior glenoid rim. It becomes confluent with the anterior glenoid labrum in the anteroinferior quadrant of the glenoid. When taut in abduction and external rotation (ER), it is the primary shoulder stabilizer. Traumatic anteroinferior glenohumeral dislocation most commonly injures the anteroinferior labrum and anteroinferior glenohumeral ligament complex. The much less well-developed posterior band of the IGHL travels superiorly from the humeral neck to the posterior glenoid rim to join the posterior glenoid labrum ( Fig. 47.3 ).
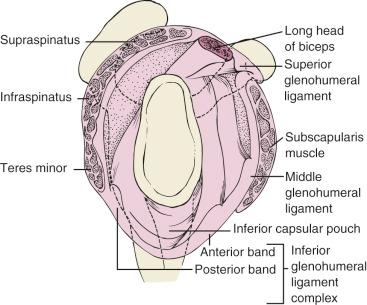
The clinical significance of the superior labrum, superior and middle glenohumeral ligaments, and coracohumeral ligaments is not as well defined. The superior glenohumeral ligament attaches at the apex of the superior labrum, along with the tendon of the long head of the biceps brachii, and at the base of the coracoid. The middle glenohumeral ligament attaches medially to the labrum along the anterior aspect of the glenoid neck. Some detachments of the superior labrum (superior labrum anterior and posterior [SLAP] lesions) and superior and middle glenohumeral ligaments are associated with instability.
The brachial plexus and peripheral nerves are intimately associated with the glenohumeral joint and shoulder girdle. Although true anatomic anomalies are uncommon, considerable variation can be seen in the exact relationship of the peripheral nerves and other shoulder girdle structures. Burkhead and colleagues have shown that the distance of the axillary nerve from the midportion of the acromion is on average 5.4 cm in females and 6.2 cm in males. The musculocutaneous nerve enters the coracobrachialis muscle on average at 5 cm from the coracoid, but a high percentage of anomalies could be found. The motor branches of the supraspinatus muscle are about 3 cm medial to the supraglenoid tubercle, and the motor branches of the infraspinatus muscle are about 2 cm from the posterior glenoid rim.
The vascular supply of the shoulder girdle is derived from the subclavian artery and the rich arborization of arteries that originate from the axillary artery ( Fig. 47.4 ). These vessels include the suprascapular, thoracoacromial, subscapular, and circumflex anterior and posterior humeral arteries. The suprascapular and posterior humeral circumflex arteries are in close proximity to the suprascapular and axillary nerves, respectively.
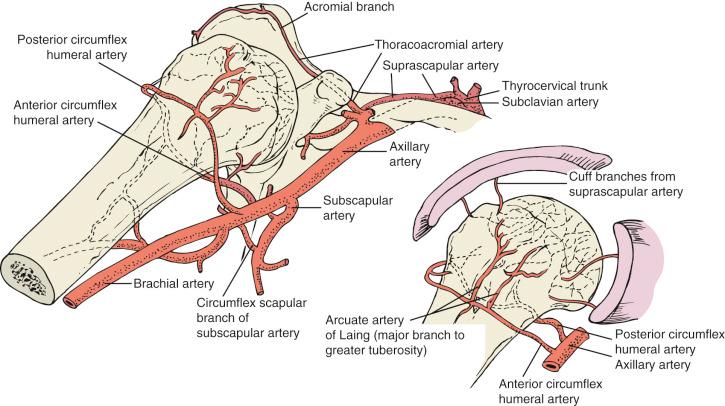
Most of the direct blood supply to the humeral head comes from the arcuate artery supplied by the anterior humeral circumflex artery, which arises from the third division of the axillary artery just above the teres major muscle. The arcuate branch ascends lateral to the biceps groove and enters the humeral head in the biceps groove to provide the major blood supply to the articular segment of the humeral head. The posterior humeral circumflex artery also sends branches to the greater tuberosity posteromedially in the area of the capsular insertion as well as supplying some of the articular segment. To a lesser extent, blood supply is provided through the rotator cuff tendon insertions on the tuberosities and through the capsule. Vessels in the medial portion of the capsule presumably maintain blood supply to the articular segment in valgus-impacted four-part fractures. Injury to the axillary artery or to the ascending branches by fracture or surgery is associated with an increased incidence of osteonecrosis. Hertel and colleagues found that the most relevant predictors of ischemia are the length of the dorsomedial metaphyseal extension of the head fragment and the integrity of the medial head/metaphysis hinge.
More than two-thirds of full overhead shoulder motion occurs through the glenohumeral joint, and the rest is through the scapulothoracic articulation. Consequently, injury to the humeral head that limits the surface of the fulcrum available for motion will have a substantial influence on shoulder function.
The intact humeral head is the fulcrum through which the deltoid and rotator cuff act to provide power for the elevation of the arm while stabilizing the humeral head within the glenoid. The active power of the rotator cuff serves to protect the passive ligamentous stabilizers from overstretching or tearing. Rotation and elevation are lost if the head fulcrum is disrupted by an injury such as fracture or dislocation.
Although the glenoid is congruent with the humeral head, the surface area of the glenoid is only 25% to 30% of the humeral head and thus provides for very little skeletal stability. Consequently, glenohumeral joint stability also depends greatly on soft tissue mechanisms.
The rotator cuff interval, including the coracohumeral and superior glenohumeral ligaments, resists inferior translation of the adducted humerus and prevents posterior dislocation in the positions of flexion or abduction and ER. The coracohumeral ligament (CHL) has a role in preventing inferior instability and restraining ER. The latter effect is commonly seen in adhesive capsulitis and shoulder contractures.
For normal function, the shoulder requires power and strength, which are derived from the coordinated interaction of at least 26 muscles, including the scapulothoracic, scapulohumeral, and thoracohumeral muscles. Although the shoulder is not subjected to the same type and magnitude of loads as the hip and knee and has been described as a non–weight-bearing joint, it is load bearing. The forces generated by the muscles that cross the glenohumeral articulation are substantial. When the arm is held in 90 degrees of abduction, the joint reaction force equals 90% of the body weight. These forces understandably increase with resisted activity.
The rotator cuff and deltoid each provide approximately 50% of the power needed for overhead lifting. These structures, combined with the scapular stabilizing muscles, allow positioning of the arm in space with power and precision. Dynamic glenohumeral stability is primarily provided by the rotator cuff muscles and tendons ( Fig. 47.5 ). Lippitt and colleagues demonstrated that stability is related to the depth of the concave glenoid fossa and the magnitude of the compressive force generated by the rotator cuff, thus confirming the role of the rotator cuff as a dynamic stabilizing mechanism. They termed this concavity-compression. The scapular stabilizing muscles assist in glenohumeral stability by maintaining the glenoid as a stable fulcrum for the proximal end of the humerus. Muscular imbalance resulting in even subtle abnormal glenohumeral translation can result in shoulder dysfunction. Disruption of any of these intricate mechanisms can result in pain and shoulder dysfunction.
Even small changes between the head and the deltoid insertion can significantly alter the deltoid length–tension ratios.
The shoulder girdle muscles also influence the degree and direction of displacement of the fracture fragments. The pull of the supraspinatus, infraspinatus, and teres minor muscles results in superior and posterior displacement of the greater tuberosity. The subscapularis muscle displaces the lesser tuberosity medially. The deltoid, pectoralis major, latissimus dorsi, and teres major muscles cause displacement of the humeral shaft.
A detailed history should obtain information related to the patient's health, activity level, and the specifics of the injury. The general history includes the patient's age, sex, hand dominance, occupation, hobbies, and how the injured extremity is used in daily life. A good understanding of the patient's general health (e.g., whether osteoporosis or any condition is present that might interfere with wound or fracture healing) is of critical importance. The incidence of osteoporosis increases rapidly after middle age, especially in women. Osteoporosis has serious implications in terms of maintenance of reduction with traditional techniques of internal fixation. Expectations regarding postoperative activities should also influence the type of treatment. In some patients, there may be previous shoulder pathology and dysfunction that may affect the outcome of treatment of a new acute injury.
An assessment of the motivation and psychologic well-being of the patient and the patient's ability to understand and follow postoperative directions during a potentially long and complicated rehabilitation is necessary. Ongoing evaluation and observation of these factors during treatment are required to make appropriate modifications in the type of immobilization, supervised therapy, and progression of activity.
The mechanism of injury (i.e., whether the trauma was mild, moderate, or violent) is an important factor that should be determined in conjunction with the physiologic status of the patient. The extent of vascular and neurologic compromise and the time of onset of these potentially rapidly deteriorating symptoms must be monitored frequently. The position of the arm and the direction of force determine the direction of glenohumeral dislocation.
A complete physical examination requires visualization of all of the injured anatomic parts. On occasion, the shoulder girdle is examined rapidly and superficially in the acute setting, and the patient is then sent to the radiology department for plain radiographs. However, imaging studies do not substitute for a careful physical examination. The initial examination in the acute injury setting is usually more difficult than in a delayed or nontraumatic setting. Complicated injuries, especially in the polytrauma setting, and those involving open fractures are splinted, and much of the evaluation that does not require the patient's subjective input or attempt to demonstrate muscle function can be delayed until the patient's condition is stabilized or the patient is taken to the operating room for treatment of associated injuries.
Adequate exposure of the shoulder girdle and upper extremity is required. An examining table in the middle of the room permits evaluation of a seated patient from the front, the side, or behind. In the supine position, other muscles can be relaxed, and the patient can be made more comfortable during this portion of the evaluation.
In proximal humeral fractures, the deltoid and surrounding soft tissues may mask significant fracture displacement or dislocation. Swelling and obesity can also obscure any alteration in skeletal landmarks. The examiner must have a high index of suspicion for skeletal injury to avoid errors in diagnosis. Swelling and ecchymosis may not be present in the acute period but may develop with time. By approximately 48 hours after injury, ecchymosis can be seen to extend across the chest or down to the elbow.
Deformity is more common with dislocations and displaced fractures. Dislocations about the shoulder are associated with visible or palpable depressions in the skin and underlying soft tissue. With an anterior dislocation, the humeral head is anterior, medial, and inferior. A sulcus is visible and palpable posteriorly and laterally beneath the acromion. With posterior dislocations, the coracoid becomes prominent, an anterior sulcus is present, posterior prominence can be noted, the arm is usually held in adduction and internal rotation, and the axis of the humerus is directed posteriorly. An inability to externally rotate the arm is the classic physical finding associated with posterior dislocation. As a result, the palm of the hand cannot be turned up even though the forearm can be supinated. In the rare inferior dislocation (luxatio erecta), the arm is held in abduction. Fracture-dislocations may be less apparent than isolated dislocations. Superior static dislocation is associated with disruption of the coracoacromial arch after a chronic massive rotator cuff tear and not the result of an acute traumatic injury.
Other areas are evaluated before addressing the proximal humeral fracture. The cervical spine is assessed for any tenderness and pain with motion. If the status of the cervical spine is uncertain, cervical spine radiographs are obtained before any movement of this area. Direct tenderness is a common clinical finding when there are fractures of the ribs, clavicle, acromion, and humerus. Pain may be elicited indirectly with motion or with longitudinal compression or distraction of the shoulder.
The early management of proximal humerus fractures is aided by clinical evaluation of the stability of the fracture. When the humerus is grasped at the elbow and the arm gently rotated, an assessment can be made regarding whether the humeral head rotates with the shaft. With careful manipulation and longitudinal traction, crepitus is a common finding with a displaced or unstable fracture unless soft tissue interposition has occurred. The lack of crepitus with a displaced fracture and an inability to obtain an accurate closed reduction suggest soft tissue interposition. If the humeral head moves with movement of the humeral shaft, then the fracture is stable either because it is impacted or there is healing.
Neurologic evaluation is carried out for all components of the upper extremity. Gentle motion and isometric contractions are generally sufficient to allow palpation of individual muscle groups as a screening test for muscle integrity and nerve supply. Radial, median, and ulnar nerve function can be assessed without disturbing the proximal humeral fracture. An attempt is made to evaluate the biceps, the triceps, the three divisions of the deltoid, the spinati, the pectoralis, the latissimus dorsi, and the trapezius muscles. Dermatomal sensory patterns are recorded, but unfortunately, sensibility in the axillary nerve distribution in the lateral aspect of the arm is not a reliable test for determining the presence of axillary motor function. It is important to remember that neurovascular injuries occur in 5% to 30% of complex fractures of the proximal end of the humerus. The axillary nerve is the most commonly injured peripheral nerve. In addition, axillary nerve injury often occurs in combination with other peripheral nerve injuries. Some of these combined injuries are infraclavicular brachial plexus injuries. Unfortunately, recovery of associated nerve injuries is often incomplete.
Early deltoid muscle atony with inferior subluxation of the humeral head can occur and must be distinguished from an axillary nerve injury. Electromyography and nerve conduction studies can be performed as soon as 3 weeks after injury and give a baseline for comparison 3 months later when the studies are repeated to assess the extent of nerve involvement. Nerve conduction studies performed before Wallerian degeneration occurs can confirm nerve continuity. A careful and detailed neurologic examination should be possible if the patient is cooperative.
In the distal part of the involved limb, the color, capillary refill, and radial pulse are examined and compared with those of the uninjured upper extremity. More detailed vascular evaluation is undertaken if arterial injury is suspected. Vascular injuries are less commonly associated with shoulder girdle trauma than neurologic injuries. Most significant vascular injuries are arterial ( Fig. 47.6 ). The collateral circulation may mask an arterial injury, and the distal pulses may be intact. Clinical ischemia may be absent initially. An expanding axillary hematoma suggests a vascular injury. Arm positioning can compromise vascularity by extrinsic compression of a major vessel. Doppler pressures should be assessed in patients with any possibility of a vascular injury, and any abnormalities should be further evaluated with arteriography. Venous injuries are less common and rarely discussed. Nonetheless, venous laceration can cause significant local bleeding. Subclavian thrombosis is associated with diffuse upper extremity swelling and edema and can be identified with duplex ultrasonography and venography.

The glenohumeral articulation lies between the sagittal and the coronal planes of the body. In the elective setting, a complete plain radiographic evaluation includes five views of the shoulder: the three right-angle views of the trauma series (true anterior-posterior [AP], axillary lateral, and Y views) and AP views in internal and ER. Computed tomography (CT), three-dimensional reconstructions, additional plain radiographic imaging, arthrography, ultrasonography, and magnetic resonance imaging (MRI) all provide further definition of shoulder injuries.
Glenohumeral congruity and reduction and the positions and relationships of the four segments of the proximal humerus can be defined in three-dimensional space with three right-angle trauma series views. These views are taken relative to the scapular plane rather than the coronal plane of the body.
The scapular AP view ( Fig. 47.7 ) centered on the glenohumeral joint is a 30-degree posterior oblique view. The glenohumeral joint space is defined clearly. In the absence of subluxation or dislocation, the humeral head should not overlap the glenoid. AP views in the sagittal plane of the body do not adequately demonstrate the posteromedial displacement of the proximal humerus that occurs with a posterior fracture-dislocation. Overlap of the head and glenoid is expected on an AP view taken in the sagittal plane of the body, but it is indicative of a posterior dislocation or fracture-dislocation in the true AP view ( Fig. 47.8 ).
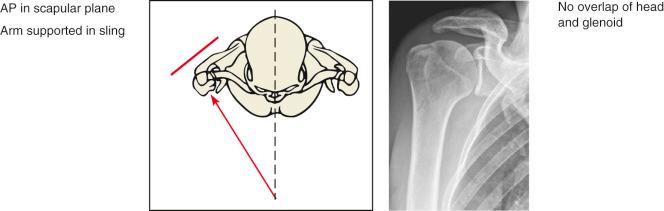
The lateral scapular view is taken at right angles to the scapular AP view; thus at a 60-degree anterior oblique angle, the beam parallels the scapular spine (see Fig. 47.7 ). The head overlaps the glenoid evenly and entirely to sit in the center of a Y formed by the scapular spine and coracoid superiorly and the scapular body inferiorly (therefore usually called the “Y view”). In this projection, an anterior dislocation is easily appreciated ( Fig. 47.9 ). More information is added regarding tuberosity and shaft displacement. It is also the best projection to assess a displaced lesser tuberosity fracture. Avulsed greater tuberosity fragments that may overlap the humeral head in the AP view can usually be seen posterior to the head on the Y view. Apex anterior angulation of a surgical neck fracture is common and can be demonstrated with a Y view. Slight scapular malpositioning leads to confusion when defining the status of the humeral head. The use of a radiograph image intensifier in positioning the patient enables an inexperienced technician to superimpose the axillary and vertebral borders of the scapula. Once superimposed, the humeral head is centered on the glenoid in a normal shoulder.

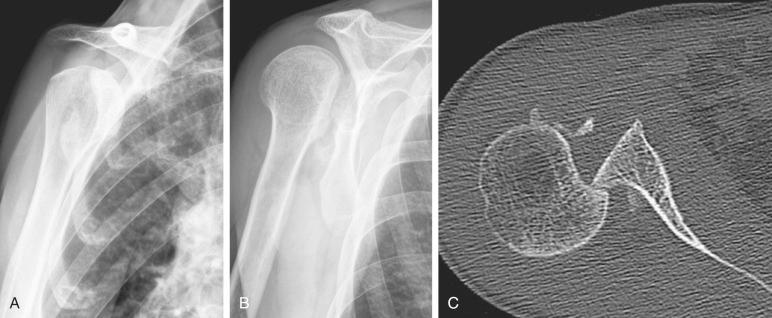
The axillary lateral view is the most useful in assessing the position of the humeral head relative to the glenoid (see Fig. 47.7 ). Although anterior dislocations can easily be distinguished on AP and lateral scapular views, subluxations, fracture-dislocations, and dislocations in the posterior direction are more difficult to diagnose and require multiplanar imaging. Head-splitting fractures are often optimally visualized on the axillary lateral radiographs. Defects in the humeral head; glenoid fractures; and fractures of the coracoid base, distal part of the clavicle, and acromion are also well visualized on axial projections.
Posterior fracture-dislocations and displaced greater tuberosity fractures are the most commonly missed fractures of the proximal end of the humerus, usually because axillary imaging is not obtained. The axial view is more difficult to perform but avoids missing these less common injuries. Although it can be difficult to position the shoulder because of pain or body habitus, many positions and projection techniques can be used to obtain a good axillary lateral image. If the AP position of the humeral head or the position of the greater tuberosity is at all uncertain, a CT scan should be obtained.
In acute trauma, an assisted axillary view is obtained with gentle longitudinal traction applied at the elbow and minimal abduction and slight shoulder flexion. This position can be maintained with a soft foam pad. The radiographic plate is placed at the top of the shoulder with the edge against the neck. The tube at the hip is directed cephalad and medial, with enough scapula visualized to adequately demonstrate humeral head articular and glenoid rim fractures and to appreciate any subluxations or dislocations. The patient can also be positioned supine holding an intravenous (IV) pole or can be positioned on the opposite, uninjured side.
When the head moves with the shaft, internal and ER views in the AP plane supplement the three-view trauma series to make up the five standard screening views recommended for routine shoulder evaluation.
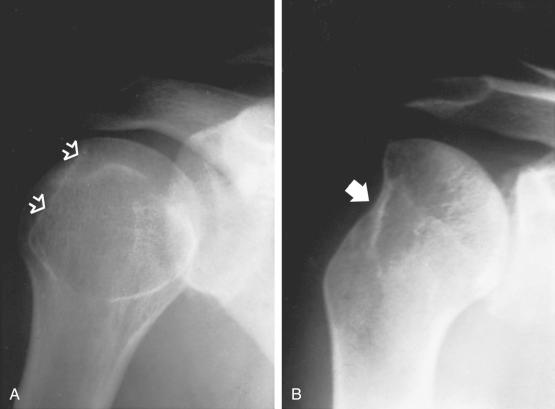
In the ER view, the greater tuberosity is normally seen. When it is absent ( Fig. 47.10 ), the axillary view is mandatory to locate any tuberosity fragment that might be retracted toward the base of the scapular spine by the spinati muscles. This fragment may be difficult to appreciate on the AP view because of superimposition with the humeral head. Occasionally, rotator cuff avulsion with a small fragment of tuberosity can be confused with a calcium deposit ( Fig. 47.11 ).

The importance of accurate classification and diagnosis of proximal humeral fractures has been emphasized. Inadequate evaluation often leads to errors in diagnosis and inappropriate treatment. A detailed history, physical examination, and plain radiographs form the basis of any shoulder evaluation. Of all the classes of shoulder disorders, fractures are perhaps the most dependent on accurate radiographic imaging technique. The three views of the shoulder trauma series (glenohumeral AP, axillary lateral, and scapular lateral) should be obtained in all cases of shoulder injury. If only two views can be obtained, the true AP and axillary lateral are the most informative.
Advances in CT imaging technology have enhanced the imaging quality, including providing routine reconstruction both in alternative imaging planes and in three-dimensional reconstruction. This imaging is useful in some cases to more precisely define the fracture and determine the treatment, especially when operative treatment is intended. Nevertheless, routine use of CT is not indicated or appropriate. Clearly, CT scanning of a nondisplaced fracture is not indicated.
When CT and standard radiography are compared, CT is superior in assessing the location of fracture lines, displacement of fracture fragments relative to their normal position, rotation of the humeral articular surface, and fractures of both the glenoid and humeral heads. Bernstein and colleagues found that the addition of CT was associated with only a slight increase in intraobserver reliability and no increase in interobserver reproducibility when classifying proximal humerus fractures according to the Neer classification. The interobserver reproducibility of the senior shoulder surgeons regarding diagnosis and treatment did not change when CT was used in addition to plain film radiography. Nevertheless, CT can be especially useful in evaluating complex fractures or malunion. CT is superior to MRI in depicting bony detail.
CT has also been used to evaluate shoulders for signs of glenohumeral instability, including glenoid rim fractures, Hill-Sachs lesions, and when arthrography is added, capsulolabral pathology.
Three-dimensional reconstruction from CT scans is readily available and allows for visualization of the fracture from any direction to determine the position and displacement of the fracture fragments. This technique gives an unparalleled opportunity to make an accurate diagnosis and plan for reconstruction. We have found three-dimensional imaging to be useful occasionally in patients with especially complex fractures. Three-dimensional imaging is also very helpful in reconstructive cases with fracture nonunion, malunion, or posttraumatic glenohumeral arthritis ( Fig. 47.12 ).
Magnetic resonance imaging is rarely indicated in the acute evaluation of a shoulder fracture. However, if plain radiography fails to demonstrate a fracture and the clinical course is not progressing satisfactorily, MRI can be used to demonstrate an occult nondisplaced fracture, most commonly a greater tuberosity fracture, rotator cuff tearing, or occult articular injury. In the acute evaluation of a displaced proximal humerus fracture, MRI is not likely to provide information that would alter treatment.
After glenohumeral dislocations, MRI can provide useful information on labral tears, chondral lesions, and acute or degenerative rotator cuff tears. Recent advances in MRI technology and the proliferation of scanners have made MRI the standard test for evaluation of the shoulder for rotator cuff pathology. MRI provides the best quality imaging and has high sensitivity, specificity, and accuracy for detection of rotator cuff pathology.
Historically, arthrography was considered the gold standard for determining the presence of full-thickness rotator cuff tear. However, it is not as helpful as clinical examination or MRI in evaluating the size of the tear or demonstrating evidence of chronic pathology such as muscle atrophy on physical examination or fatty infiltration and atrophy of the rotator cuff muscles on MRI.
Shoulder ultrasonography has been used primarily for imaging of the rotator cuff. Although it is used extensively at some centers and by some individual practitioners, ultrasonography has not gained widespread acceptance. Patten and colleagues reported that ultrasonography can be used to identify occult nondisplaced greater tuberosity fractures. Ultrasonography is the least expensive, no radiation is used, and the other shoulder can easily be imaged for comparison. Experience with ultrasonography has been varied, and the results are operator dependent. A study by Teefey and colleagues reported high sensitivity and specificity for the detection of rotator cuff tears.
Although radiograph image intensifier is not used for routine shoulder imaging, it has distinct advantages in positioning the patient for radiography, in determining motion at a delayed union or nonunion site, and in evaluating stability in cases in which the degree of stability is the determining factor for open reduction and internal fixation (ORIF). A radiograph image intensifier is especially useful for intraoperative imaging.
Usually, the diagnosis of a proximal humerus fracture is straightforward. The differential diagnosis of proximal humeral fractures and glenohumeral dislocations includes muscle contusion or sprain, rotator cuff tear, brachial plexus injury, infection, disruption of the axillary artery, neuropathic arthropathy, and thrombosis of the axillary vein. Imaging studies combined with the history and physical examination enable differentiation of these injuries. When evaluating patients with proximal humerus fractures, always consider the possibility of concurrent shoulder girdle injury.
Operative treatment of an injured shoulder requires detailed and complete knowledge of the anatomy of the shoulder girdle. Shoulder anatomy is complicated and can be treacherous for inexperienced or occasional shoulder surgeons. Few shoulder injuries require immediate or emergency surgery. In most cases, surgery is performed when the patient is medically stable and the surgeon and operating room are ready and adequately equipped. All necessary fixation devices and prostheses should be in the operating room before the patient is anesthetized.
Either general anesthesia or an interscalene nerve block can be used for closed reduction or open surgical procedures on the shoulder girdle. When general anesthesia is used, it is important to be able to paralyze the patient to relax the muscles around the shoulder and facilitate retraction and exposure. Many centers specializing in shoulder surgery have extensive experience with interscalene nerve blocks ( Fig. 47.13 ). Regional anesthesia may avoid some of the risks associated with general anesthesia and paralyzing anesthetic agents, as well as the often-unpleasant side effects of general anesthesia, and has not been associated with a significant incidence of complications. Additionally, some benefit may be derived from the preemptive analgesia (before the surgical procedure) that the block provides. Importantly, the nerve block provides substantial postoperative pain relief and lessens the need for large doses of narcotics immediately after surgery. The use of ultrasonography in regional anesthesia may reduce the minimum effective volume of the anesthetic required to accomplish successful blockade. Furthermore, it can lead to a high success rate, simultaneously reducing the rate of adverse effects. Combined general anesthesia and interscalene nerve block is ideal. The regional block provides paralysis and analgesia, and the general anesthetic controls the patient's airway and avoids the problems that can be encountered with a semiconscious and uncooperative patient. One possible disadvantage of regional anesthesia is that the function of neural structures cannot be properly assessed immediately after the operation.

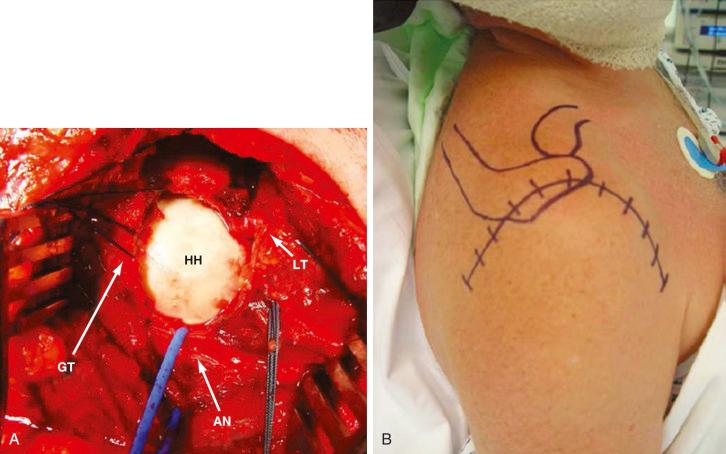
Intraoperative radiographs are required for adequate evaluation of the operative treatment of proximal humeral fractures and fracture-dislocations. Obtaining quality images is particularly challenging in these cases because the patient is often positioned in the beach-chair, or semisitting, position, and the plane of the glenohumeral joint is oblique. Image intensification is very useful because it allows greater flexibility in obtaining the correct projection, and multiple images can be obtained without having to wait for films to be developed. Biplanar radiography or image intensification is difficult but can be facilitated with proper patient positioning. If surgery is performed with the patient in the supine position, a radiolucent table can be used. In the beach-chair position, most standard operating room tables can be set up so that an image intensifier can be used. Specialized radiolucent table attachments designed for shoulder surgery can simplify intraoperative imaging.
A hemostatic gelatin (Gelfoam) mattress is placed on the operating table to provide additional padding and protection of bony prominences. The patient is positioned in the beach-chair position for anterior and superior approaches, and the lateral decubitus position is used for most posterior approaches. The upper section of a standard operating room table is replaced with a padded articulating headrest (that is adjusted to position and support the head so that the cervical spine is slightly flexed and deviated to the opposite side approximately 10 degrees). Such positioning gives more exposure superiorly in the region of the neck. The patient is positioned at the edge of the table so that the arm can be extended vertically off the edge. The scapula is padded forward with a gel bolster. A narrow gel pad can be placed over the taped eyes. A towel is wrapped around the head to exclude the hair and anesthesia tubes from the operative field. Anesthesia tubing is positioned away from the operative field. The contralateral arm and both legs and heels are positioned and padded to protect the skin and peripheral nerves.
If an autogenous bone graft (in addition to what is available in the surgical field) may be necessary, the anterior iliac crest can be positioned and prepped. A bolster under the buttock and hip makes the anterior iliac crest more prominent and facilitates exposure. Harvesting bone from the opposite anterior iliac crest permits simultaneous shoulder surgery. However, if the ipsilateral iliac crest is the donor site, the patient will be able to hold an assistive device for ambulation with the uninjured arm. The latter is preferred.
Presurgical disinfection of the patient's skin is performed according to actual standards. An adherent SteriDrape is applied high on the neck with the tails toward the axilla to isolate the surgical field.
The entire shoulder and upper extremity are prepped, and the surgical field is draped so that the arm remains free. If available, the forearm and hand are placed in a sterile articulating arm holder and positioner, which is extremely helpful during the procedure because the arm can be precisely positioned. This device facilitates exposure and positioning for imaging and frees the assistants’ hands ( Fig. 47.14 ). Prophylactic antibiotics are given before the skin is incised. The Cell Saver can be used if significant blood loss is expected, which is seldom in shoulder surgery. The skin incision is marked, and the exposed skin could be covered with an adherent iodine-impregnated drape.

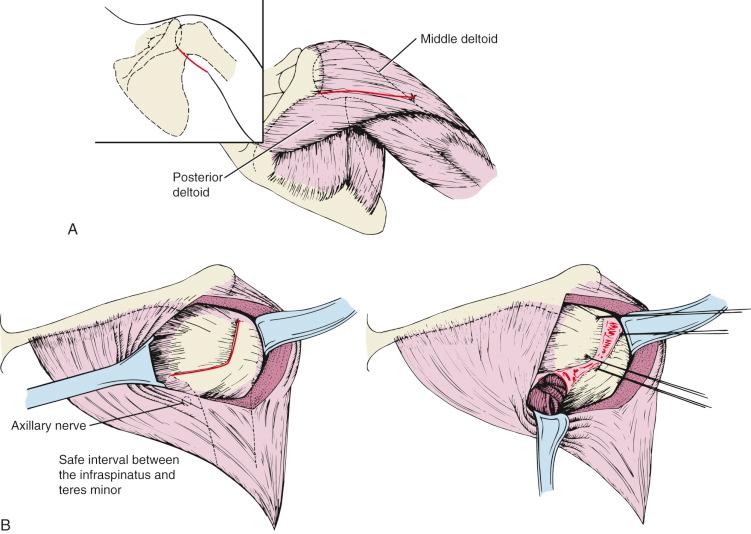
The surgeon needs to be familiar with three approaches to the shoulder. The deltopectoral approach can be used for most fractures. The superior approach gives access to the subacromial space, including the greater tuberosity and rotator cuff. The superior deltoid-splitting approach can also be extended distally after exposing the axillary nerve. Occasionally, a posterior approach is necessary for posterior and inferior glenoid fractures or a malunited greater tuberosity fracture, but this approach is seldom necessary for ORIF of acute proximal humeral fractures or for prosthetic replacement.
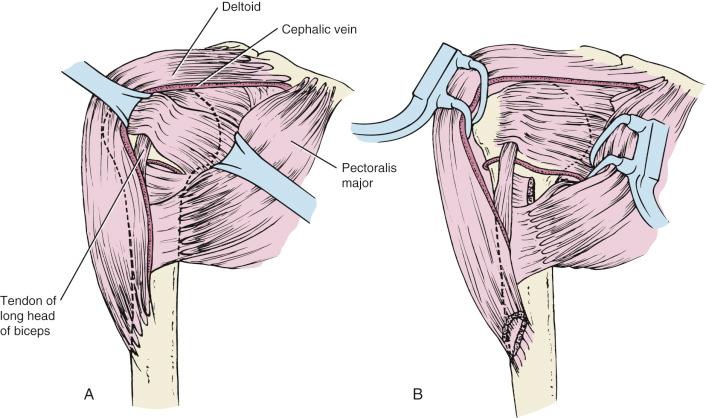
The incision for the deltopectoral approach begins at the distal third of the clavicle, passes just lateral to the coracoid, and extends to the deltoid insertion ( Fig. 47.15 ). The length of this incision is primarily dependent on the size of the patient and the extent of humeral exposure required. Recent interest in shorter incisions and minimally invasive surgery should not lead a surgeon to compromise the exposure of the fracture. Inadequate superficial exposure around the proximal humerus is more likely to lead to overly forceful retraction of the deeper muscles, potentially resulting in increased scarring and neurologic injury. Occasionally, a more cosmetically acceptable incision can be made in Langer's lines from the coracoid process to the axilla. The cephalic vein is preserved and retracted laterally with the deltoid muscle. Care is taken at the upper end of the deltopectoral interval to avoid disrupting crossing branches of the cephalic vein. The clavipectoral fascia is incised lateral to the conjoined tendon to expose the subscapularis tendon and lesser tuberosity. Careful blunt dissection under the deltoid and in the subacromial space improves exposure. Self-retaining retractors are used to retract the deltoid laterally and cephalad and the pectoralis major and intact coracoid muscles medially. Self-retaining retractors should be used with caution to avoid iatrogenic nerve injury. Abduction of the arm provides better wound exposure if necessary. However, we prefer not to affect the insertions of deltoid or pectoralis major muscles. The coracoid muscles are left intact, and the coracoid is not osteotomized to protect the brachial plexus. Although the coracoacromial ligament can be incised to improve exposure, we preserve it whenever possible. The axillary nerve is exposed only if necessary, but it has to be carefully protected throughout the procedure. The tendon of the long head of the biceps is the key landmark in the approach to the proximal part of the humerus.
In many cases, a fracture can be reduced and fixed without opening or exposing the glenohumeral joint. For a two-part surgical neck fracture, the glenohumeral joint rarely needs to be opened. For a posterior dislocation in which the articular deficit in the head is less than 20%, an opening through the subscapularis is used; however, if the deficit is between 20% and 40%, osteotomy of the lesser tuberosity enables transfer of the lesser tuberosity into the humeral head deficit. In three-part fractures, the joint is occasionally already exposed by avulsion of one of the tuberosities. The rotator cuff interval between the subscapularis and the supraspinatus can be extended medially to improve access to the glenohumeral joint. In four-part fractures, both tuberosities are usually separated, but in the rare instance in which they are still intact at the biceps groove, the groove is osteotomized, and the glenohumeral joint is exposed through the rotator interval.
The superior approach incorporates a split in the deltoid muscle ( Fig. 47.16 ). The skin incision can be made either following Langer's lines over the lateral border of the acromion or longitudinally in line with the deltoid muscle fibers. The former incision extends from the mid-acromion to 2 or 3 cm beyond the anterior acromion. The skin and subcutaneous tissue are elevated medially and laterally in full thickness to give wide exposure. The deltoid is split laterally from a point just posterior to the anterolateral corner of the acromion and posterior to the tendinous raphe between the anterior and the middle deltoid. The acromial branch of the thoracoacromial artery is coagulated. Small retractors are placed to retract the deltoid. Care is taken to avoid splitting the deltoid any more than 4 or 5 cm lateral to the acromion to prevent injury to the axillary nerve. Any portion of the underlying hemorrhagic bursa that obscures the needed exposure is excised. A stay suture can be placed at the distal portion of the deltoid split, 5 cm below the acromion, to prevent injury to the axillary nerve. This operative approach is commonly used for greater tuberosity fractures and can be used for valgus impacted fractures. More distal exposure of the surgical neck and proximal humerus is limited with this approach unless the deltoid split is extended.
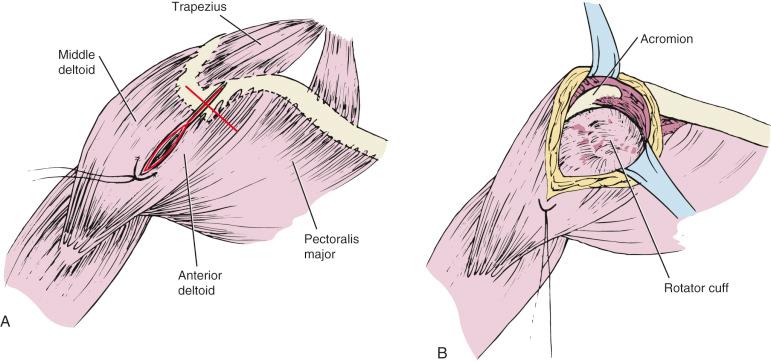
An extended modification of the superior deltoid-splitting approach was recently described. The dissection is continued distally after the axillary nerve has been located and identified ( Fig. 47.17 ). The deltoid is split distal to the crossing axillary nerve to provide more distal exposure of the proximal humerus. This facilitates the more distal exposure that is required for plate fixation of proximal humerus fractures. Concern about axillary nerve injury is valid but appears to be avoidable.
The posterior approach is a safe approach to the posterior aspect of the shoulder joint. It is generally used for scapular body, scapular neck, and glenoid fractures; fractures of the acromion; and posterior shoulder stabilization. However, it can also be used for shoulder joint replacement with simultaneous posterior glenoid reconstruction and treatment of posterior dislocated proximal humerus fractures.
In most cases, the posterior approach to the shoulder is performed with the patient in the lateral decubitus position. General anesthesia is preferred. A vacuum mattress or hip arthroplasty-positioning system is used to support the patient. A soft gel bolster is placed underneath the upper chest wall to protect both the brachial plexus and the dependent shoulder. The arm is positioned with a sterile articulating arm holder that is attached to the table on the anterior side of the patient.
The scapular spine and acromion are the landmarks for positioning of the skin incision. Depending on the goal of surgery, the incision could be vertical, horizontal (along the scapular spine), or oblique (along the lateral border of scapula). Our preferred incision is angle bisector between the scapular spine and lateral border ( Fig. 47.18 ). The deltoid muscle with a bony chip is partially detached from scapular spine. It is advantageous to start from lateral because the interval between the deltoid and infraspinatus is better defined there. Under the deltoid, the infraspinatus is exposed, and the internervous plane between the infraspinatus (suprascapular nerve) and teres minor (axillary nerve) is followed to reach the glenoid. If necessary, the scapular neck can be exposed through a more dangerous internervous plane between the teres minor (axillary nerve) and teres major (subscapular nerve). In this case, it is important to identify the axillary nerve. For better visualization of the posterior capsule and glenoid, the infraspinatus can be laterally detached at its tendinous insertion and sutured with nonabsorbable material (size #2 to #3) at the end of the procedure. The deltoid muscle is reinserted with two to four transosseous sutures using the same nonabsorbable material.
Recent trends in clinical medical practice have emphasized the importance of outcome evaluation. Numerous orthopaedic rating systems have been described. Originally, most systems were formulated to assess the outcome of specific surgical procedures, but more recent work has emphasized the importance of using measures of general health status and site- and disease-specific outcome to evaluate the results of treatment.
Early shoulder evaluation scores were developed to assess the results of specific shoulder procedures. The Neer score was devised to evaluate the results of shoulder arthroplasty ; the Rowe score evaluates the results of shoulder instability repairs. More recently, several outcome evaluation systems for assessing the shoulder have been developed, including the Constant-Murley score; the American Shoulder and Elbow Surgeons (ASES) score; and the Disability Arm, Shoulder, and Hand (DASH) questionnaire.
The Constant-Murley score evaluates pain, the ability to perform activities of daily living, shoulder motion, and abduction strength. Additionally, the score is normalized to age. It is the only measurement tool that was subjected to validation in its original publication. Conboy and associates studied the Constant-Murley score and raised questions about its validity for the generic evaluation of all shoulder disorders.
The original ASES shoulder evaluation form provides an organized format to record subjective and objective data. It was not intended to be used for calculation of a composite score. This work has been updated and evaluated in field tests. More recent work on outcome evaluation emphasizes subjective patient parameters.
The DASH evaluation was developed by the American Academy of Orthopaedic Surgeons in conjunction with the Institute for Work and Health of the University of Toronto and member organizations of the Council of Musculoskeletal Specialty Societies. It includes patient-reported domains such as symptoms, function, expectations, satisfaction, and quality of life and is designed to be a broadly applicable outcome instrument for the upper extremity.
The general health status of orthopaedic patients is most commonly evaluated with the Short Form 36 (SF-36) questionnaire. The SF-36 Health Survey was developed as an abbreviated form of the Medical Outcomes Study Survey, which assesses 40 physical and mental health concepts. It is a generic measure because it assesses health concepts that represent basic human values relevant to functional status and well-being. The eight scales of the SF-36 Health Survey assess the physical and mental aspects of behavioral functioning, perceived well-being, social and role disability, and personal evaluation of health in general.
Outcome evaluation of proximal humeral fractures is complicated by the fact that premorbid assessment is not available. Thus using outcome evaluation tools that are designed to assess treatment of chronic shoulder conditions such as glenohumeral arthritis and rotator cuff tears may not be valid. Comparison with the unaffected extremity is usually helpful, as is consideration of age-matched normal function.
The concept of a minimal clinically important difference (MCID) has been proposed for various clinical outcome scores, specifically quality-of-life assays. Knowing the minimal difference that patients may believe is quality of life improvement allows for better assessment of published studies. Instead of academic “statistical” differences, MCID should lead to a more practical and relevant interpretation of results.
Fractures and especially fracture-dislocations of the proximal humerus are challenging injuries for treating surgeons. The individuality of affected patients, fracture pattern, and vascular impairment, as well as bone quality, makes uniform treatment difficult. Since Neer's fundamental works in 1970, many attempts have been made to quantify or classify these variables more precisely to improve the treatment and patient outcome. Later, technologic progress in imaging and implant design offered new possibilities. However, there still was no gold standard for the treatment of fractures of the proximal humerus until now, and surgery is mainly dependent on the surgeon's preference and experience. This section provides a summary of what is known and what still remains controversial on this topic. The treatment is no longer focused on different fracture patterns only because the aforementioned individual factors play an important role in the decision-making process, too.
The section Surgical Treatment provides instructions and reduction maneuvers for specific fracture types, and the most important implants are described, considering their appropriate spectrum of fracture types. At the end of the section, the authors’ preferred method gives an idea for the treatment of proximal humerus fractures. It ranges from conservative to reverse total shoulder arthroplasty (RTSA) because surgery should be versatile to be appropriate to the individuality of the patient and the different fracture patterns.
In this book's edition, we first present the results of our patients treated according to the evidence-based treatment algorithm published in the fifth edition of this book. With the help of these results and our first experiences, we further developed and simplified the algorithm. In this chapter, we present the latest version currently being used in our clinic.
Proximal humeral fractures account for nearly 6% of all fractures. Although they may occur in any age group, with the earliest noted at the time of birth, an increased frequency occurs in older-middle-aged and elderly individuals because of the age-related increase in osteoporosis.
In adults, the incidence of proximal humeral fracture is lowest in the third decade of life and increases in both sexes until the age of 50 years. Thereafter, the incidence increases with a female-to-male ratio of 4 : 1. The greatest number of fractures in adult men appear during the active ages between 30 and 60 years; in women, a clear increase is noted after menopause. Court-Brown and Caesar found that the incidence increases rapidly with age, with about 80% affecting individuals older than 50 years. Epidemiologic studies demonstrate that the incidence of proximal humeral fractures is increasing as a result of increased life expectancy. Kannus and colleagues reviewed the incidence of osteoporotic proximal humerus fractures in Finland from 1970 to 2007 and found a clear increase from the early 1970s until the mid-1990s, which was followed by stabilized fracture rates of 289 per 100,000 in 2007. Reasons for this increase and later stabilization are unclear, but a healthier aging population with a reduced risk of injurious falls was one of their possible explanations.
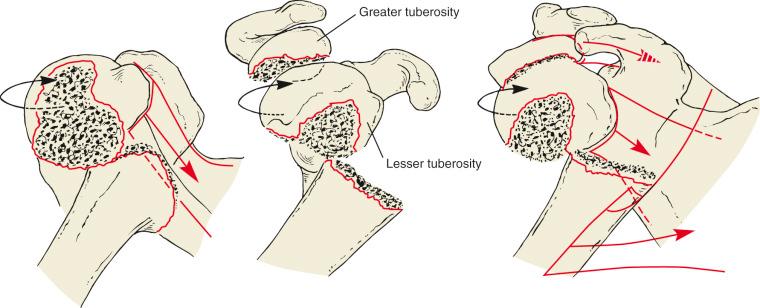
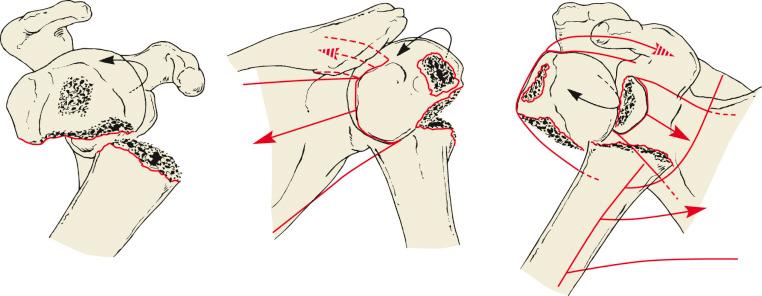
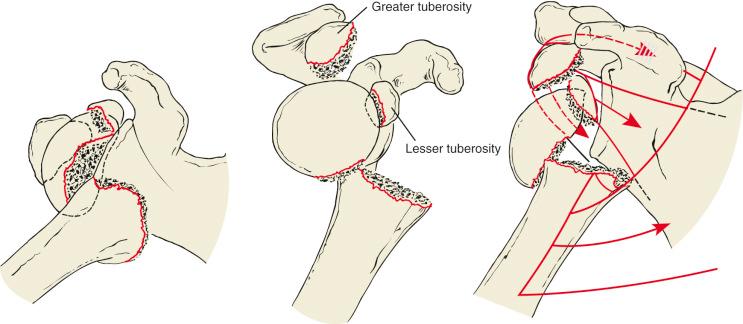
The exact mechanism of injury that leads to a proximal humeral fracture is often difficult to determine. Basically, the type of fracture depends on the position of the arm in relation to the trunk at the moment of impact, when the humeral head is pushed against the glenoid or the acromion. For example, a straight lateral impact from a fall or direct trauma on the adducted upper arm can result in a typical surgical neck fracture or a head-split fracture as described in Neer's group VI. Having the arm in a more abducted position will result in more valgus impaction. Posterior fracture-dislocation can result from direct trauma to the adducted and internally rotated extremity, but ER and abduction can lead to anterior dislocation with an avulsion fracture of the greater tuberosity, especially in older patients. Whereas the number of resulting fragments depends on the severity of impact and the bone quality, the amount and direction of fragment displacement are given by the pull of their inserting muscles ( Figs. 47.19 to 47.21 ).
With advancing age, less trauma is required to produce a fracture of the proximal end of the humerus. In patients younger than 50 years, the most common causes of proximal humeral fractures involve violent trauma, such as falls from heights, motor vehicle accidents, and athletic injuries. In patients older than 50 years, a fracture can result from minimal to moderate trauma, such as a fall from the standing position or even direct impact.
In the management of patients with multiple trauma, fractures of the proximal humerus are secondary to injuries of the head, trunk, and lower extremity. Basically, definitive surgery in terms of early total care can be considered in a stable patient with no other, more urgent skeletal injury, such as of the tibia, femur, pelvis, or spine, to improve early mobilization. In a hemodynamically unstable patient, the arm can be temporarily fixed in a body bandage until the patient is stabilized, but days 2 to 4 do not offer optimal conditions for definitive surgery. Fracture-dislocations should be reduced urgently because they can be associated with neurovascular injuries with significant disruption of the soft tissue and vascular supply of the humeral head. In locked anterior or posterior fracture-dislocations with a surgical neck fracture, closed reduction should be avoided because iatrogenic head displacement is described with detrimental outcome.
Open proximal humeral fractures are rare and usually the result of penetrating or high-energy blunt trauma. They are managed in the same fashion as other open fractures. Treatment begins with débridement and irrigation of an adequately exposed wound, prophylactic antibiotics, skeletal stabilization with either temporary external fixation or definitive internal fixation, and delayed soft tissue closure as indicated.
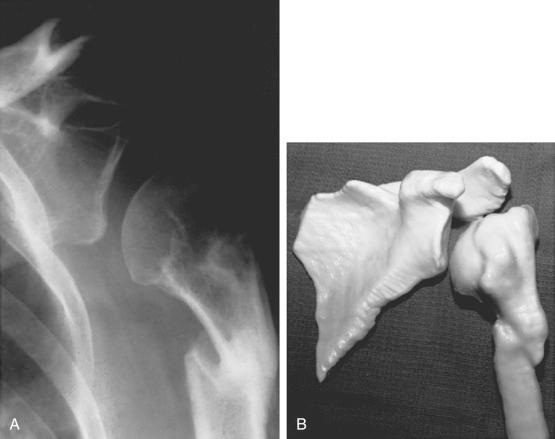
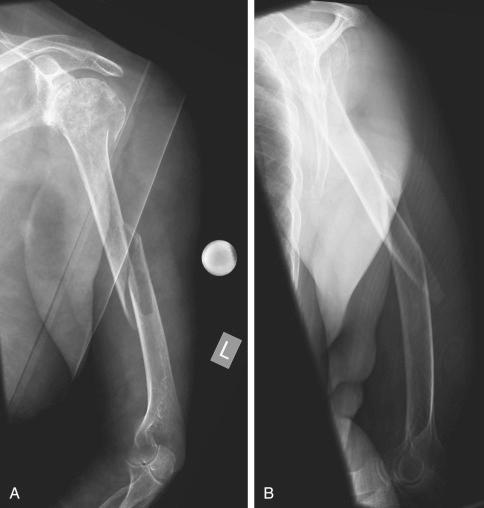
Ipsilateral upper extremity fractures are uncommon. They most often occur in the setting of multiple trauma or severe multifocal upper extremity injury. Pierce and Hodurski reported that in 21 patients with proximal humerus fractures who sustained ipsilateral radial and ulnar fractures, more than 50% experienced residual nerve injury, including injury to the brachial plexus and radial and ulnar nerves. Shaft and more distal humeral fractures may have an unsuspected associated proximal humeral fracture or fracture-dislocation ( Fig. 47.22 ).
Lehman and colleagues found an age-related increase of full-thickness rotator cuff tears (without fractures) in a large population of 456 cadavers. The overall incidence of rotator cuff tears was 17%, but it was only 6% in cadavers younger than the age of 60 years and 30% in cadavers older than the age of 60 years. Milgrom and colleagues even found an 80% incidence of rotator cuff tears in patients older than 80 years of age.
The integrity of the rotator cuff in fractures of the proximal humerus has only been addressed specifically by a small number of studies. This high incidence of rotator cuff tears in a population that is also prone to proximal humeral fractures complicates the methodologies of studies on this specific topic. Neer already described a “pathognomonic” longitudinal tear of the rotator cuff when the tuberosities were separated. The repair of this tear located at or posterior to the rotator cuff interval was an integral part in the surgical treatment. In a first study specifically addressing this topic, Wilmanns and Bonnaire retrospectively found a high incidence of rotator cuff involvement at final follow-up in an inconsistently treated series of proximal humeral fractures. They also proposed that tears of longitudinal types in the interval were caused by trauma, but transverse types were caused by degeneration. The tears were in correlation with malunion of fragments and limited functional outcome at 1 year. They therefore supported the need for cuff repair during fracture reduction. However, it is not clear whether the functional limitation is the consequence of the malunion or the rotator cuff tear in this series. In a more recent prospective study on conservatively treated proximal humeral fractures with sonographic examinations at the time of injury and at 12 months, an incidence of 50% full-thickness rotator cuff tears was found by Nanda and colleagues. The tears mainly occurred in combination with three- and four-part fractures. However, no difference in clinical outcome was found; thus the authors abstain from routine imaging of the rotator cuff in patients for whom conservative treatment is preferred. These findings are in contrast to the results of Fjalestad and colleagues, who performed a prospective MRI study on conservatively treated fractures in 76 patients with a mean age of 68 years. They found rates of 5% for full- and 24% for partial-thickness rotator cuff tears at the time of injury and rates of 10% for full- and 32% for partial-thickness tears at a follow-up of 12 months. In this study, rotator cuff involvement was mainly found in complex fractures (types 11-B2 and 11-C2 according to Arbeitsgemeinschaft für Osteosynthesefragen [AO] classification). The authors found, against the findings of Nanda and colleagues, that patients with rotator cuff tears had significantly worse functional results at 12 months even when controlled to a matched fracture group without tears.
The diverse incidences in these two prospective studies might be related to the different radiographic examinations (ultrasound vs. MRI) that were used. However, the definitive nature of rotator cuff tears in fractures of the proximal humerus has not been assessed so far. Also, the influence of the cuff tear on final functional outcome in conservatively treated patients is not fully clear regarding these studies. The extent and functional effect of either traumatic or degenerative rotator cuff tears also depend on the displacement and the final position of the tubercles, which might not be anatomic after conservative treatment.
In patients undergoing ORIF, the authors try to fix detected rotator cuff tears whenever feasible to achieve the best chances to restore full shoulder function. When it comes to arthroplasty, an associated rotator cuff tear would be an indication for a RTSA rather than a hemiarthroplasty in an active elderly patient.
Traumatic brachial plexus injuries can be classified as either infraclavicular or supraclavicular. The infraclavicular plexus is mainly compromised with dislocations or fractures of the proximal humerus, and most of these nerve lesions are denervation injuries caused by traction.
In the literature, the incidence of nerve injuries associated with proximal humeral fractures ranges from 2% to 67% and depends on the diagnostic examination. Physical examination, especially sensation of the axillary nerve, is not sensitive. Visser and colleagues performed prospective electromyographic (EMG) studies on 77 patients with glenohumeral dislocation (including 12 greater tuberosity fracture-dislocations) and on 143 patients with displaced and undisplaced fractures of the proximal humerus. They found that 48% of nerve injuries were associated with glenohumeral dislocations and 67% with proximal humeral fractures. Depending on the fracture type (Neer groups II to VI), an 82% rate of nerve involvement was found in the EMG. The axillary nerve was the most frequently injured, followed by the suprascapular nerve, the radial nerve, the musculocutaneous nerve, the median nerve, and the ulnar nerve. Combinations of these nerves were frequent. The authors conclude that EMG studies are not needed routinely because the prognosis of nerve lesions after minor trauma with shoulder dislocation or fracture is favorable. They recommend EMG in patients with severe paresis or paralysis 3 weeks after trauma to determine the severity of the axonal injury and follow-up examination after 3 months if recovery is slow.
However, in cases with no recovery after 3 to 6 months despite extensive rehabilitation, surgical reconstruction may be indicated. Special attention is needed when pain is persistent or worsening after reduction or stabilization of the fracture, particularly when associated with a deepening of nerve palsy. Stenning and colleagues described low-energy arterial injury with expanding hematoma or false aneurysm compromising the brachial plexus. Undetected, this situation may threaten the viability of the limb and is an indication for emergency angiography and vascular surgery.
Generally, most nerve injuries after fractures of the proximal humerus resolve spontaneously within 5 months, but rehabilitation and functional results may be compromised. Shoulder stiffness is an especially common complication in these patients. The outcome after surgical reconstruction depends on the location of the lesion. Good recovery can be expected in 70% to 80% of grafted patients with lesions close to the effectors (axillary, suprascapular, musculocutaneous, and radial nerve), but the outcome is worse in lesions of the median or ulnar nerve, which are far from effectors.
Vascular injuries after fractures or fracture-dislocations of the proximal humerus are rare but described in several cases mainly related to atherosclerotic vessels in elderly patients but also in adolescents. No clear incidences are mentioned. Symptoms can be clear (expanding hematoma, absent pulses in a cold arm) but also vague because palpation of distal pulses is not sensitive because of collateral circulation of the shoulder. An initial neurovascular examination is therefore important, and changes or irregularities of distal pulses have to be noticed early. Doppler ultrasonography can be used for the primary assessment. Angiography is recommended if vascular injury is clinically suspected. If confirmed, it should be treated as an emergency with immediate surgery because amputation rates are reported to be up to 50% for patients with delayed diagnosis and treatment. If vascular repair can be done within 12 hours of injury, a reasonable chance of success can be expected. If possible, the open reduction and fixation of the fracture should be done before the vascular reconstruction to protect it later on. However, in a multiply injured patient, other factors have to be kept in mind, and temporary fixation of the fracture can be an option in these specific cases; prophylactic fasciotomies of the arm and forearm can be considered. Serial Doppler examinations after surgery are advised.
The violent muscle contraction that occurs in grand mal seizures and electric shock can cause fractures and fracture-dislocations of the shoulder. The large internal rotators and adductors of the arm easily overpower the external rotators and result in a posterior fracture-dislocation. However, Bühler and Gerber described a nearly equal rate of anterior and posterior dislocations in their collective of 26 patients with shoulder instability caused by seizures.
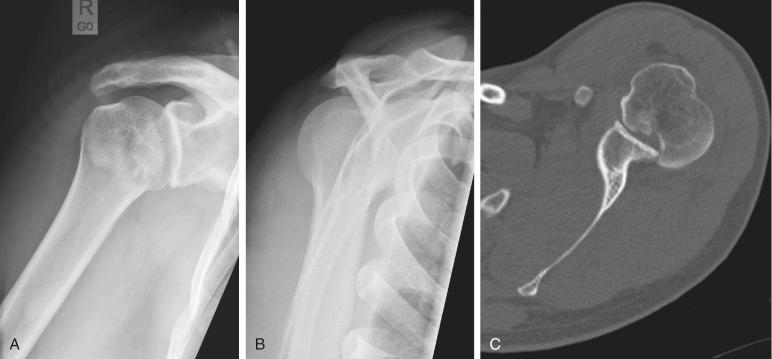
The incidence of fractures of the proximal humerus in a population with epilepsy is 4.2 times higher than for a matched “normal population.” Later, seizures were found to be one of the most important causes of posterior fracture-dislocation and the most common causes of bilateral posterior fracture-dislocations. However, these injuries can be missed easily, and severe impairment of the shoulder function has been described in such cases. Therefore it is crucial to rule out posterior glenohumeral dislocation in patients with shoulder pain or limited shoulder function (especially painful limited ER) and a known or unclear history of seizures ( Fig. 47.23 ).
Pathologic fractures result from either primary bone tumor, which is rare, or more often from metastases. The most common primary tumors that metastasize to bone are breast, lung, kidney, and prostate carcinoma. The distribution of skeletal affection is spine, ribs, pelvis, and shoulder. Depending on the location and the type of the metastatic lesion in the proximal humerus, the treatment varies among prosthetic replacement, intramedullary nailing, or ORIF with cement augmentation. The value of postoperative external-beam irradiation depends on the radiosensitivity of the primary tumor.
Clinical examination in patients with suspected fracture of the proximal humerus consists of a thorough history and physical examination. The history should give an idea of the mechanism of trauma and the severity of injury (e.g., high velocity or domestic fall). Whereas patients who sustained a high-velocity trauma are prone to associated injuries of the thoracic wall, cervical spine, or other extremities, a pathologic fracture can be suspected with a history of minimal or no trauma. Also, a history of previous osteoporotic fractures, the patient's level of activity, and the patient's ability to participate in structured rehabilitation protocols should be assessed. This is important information for the further strategy of treatment.
On physical examination, soft tissue swelling, ecchymosis, and deformity can be present. The examiner should also look for concomitant injuries in a short body check (head, spine, chest, pelvis, upper and lower extremity), especially the elbow and wrist of the affected side. Shoulder function is often too painful to examine. However, the assessment of the neurovascular status is crucial and belongs to the primary examination. The sensorimotor function of the axillary, suprascapular, musculocutaneous, and radial and ulnar nerves should be assessed and documented before further treatment. Special attention should be paid to the examination of the axillary nerve function, which is the most commonly affected nerve in fractures or fracture-dislocations of the proximal humerus. The examination of the sensation of the axillary nerve is not reliable for the presence of a lesion. A possibility to clinically assess its motor function in the situation of acute pain is to put one hand at the patient's elbow and the other hand at the surface of the deltoid muscle. The patient is then told to abduct the elbow against the examiner's hand such that contractions of the deltoid muscle can be felt with the other hand. If a contraction of the deltoid is present, the axillary nerve is certainly continuous. However, exact quantification of nerve injuries can only be assessed by EMG (see Nerve Injuries ).
For the vascular status of the affected arm, radial and ulnar pulses should be palpated at the primary examination. If pulses are irregular or weak and an arterial injury is suspected (e.g., history of high-velocity trauma), Doppler ultrasonography should be used for further examination (see Nerve Injuries ).
The exact radiographic investigations are described in detail in the first part of this chapter. Primary radiographic examination of suspected proximal humeral fractures or fracture-dislocations consists of a trauma series (AP, scapular lateral, and axillary view). Classification of the fracture and the treatment decision are usually based on these primary radiographs. In a study conducted by Sidor and colleagues, all three radiographs were necessary to achieve a 99% rate of fracture classification. Without the axial view, they reached a rate of 79%. However, the axillary view is not accurate for the determination of the sagittal angulation, but it gives important additional information when the glenohumeral joint space cannot be seen in the AP view. In this situation, for example, a locked posterior fracture-dislocation can be ruled out by an axial view (see Fig. 47.23 ). Parsons and colleagues paid special attention to the radiographic evaluation of the displacement of the greater tuberosity and found an AP view with 30 degrees of ER to be the most reliable.
CT is gaining importance for the classification of the proximal humeral fractures and their preoperative planning because fracture displacement, glenoid version, and bone stock, as well as bone quality, can be assessed.
During the past century, various classification schemes have been used to describe proximal humeral fractures. Consequently, it has been difficult to compare the results of the early but also of the actual literature on proximal humeral fractures and fracture-dislocations. Despite voluminous experience with these fractures, their treatment based on classifications remains controversial.
Early classification schemes considered the anatomic level of fracture and the mechanism of injury but did not consider the importance of fracture anatomy or displacement of the fracture. Codman noted that most proximal humeral fractures occur along the lines of the former physes of the proximal end of the humerus and described four possible fracture fragments: greater tuberosity, lesser tuberosity, anatomic head, and shaft. Based on these four fragments, Neer proposed the four-segment classification system, which included his clinical and operative findings.
In his study about classification and evaluation of fractures of the proximal humerus, Neer considered the degree of displacement to be clinically important ( Fig. 47.24 ). He originally described six groups. In group I, “minimum displacement,” all fractures with less than 1 cm or 45 degrees of displacement were included, regardless of the numbers of segments involved. These fractures were named “one-part” fractures in a later adaptation of his classification.
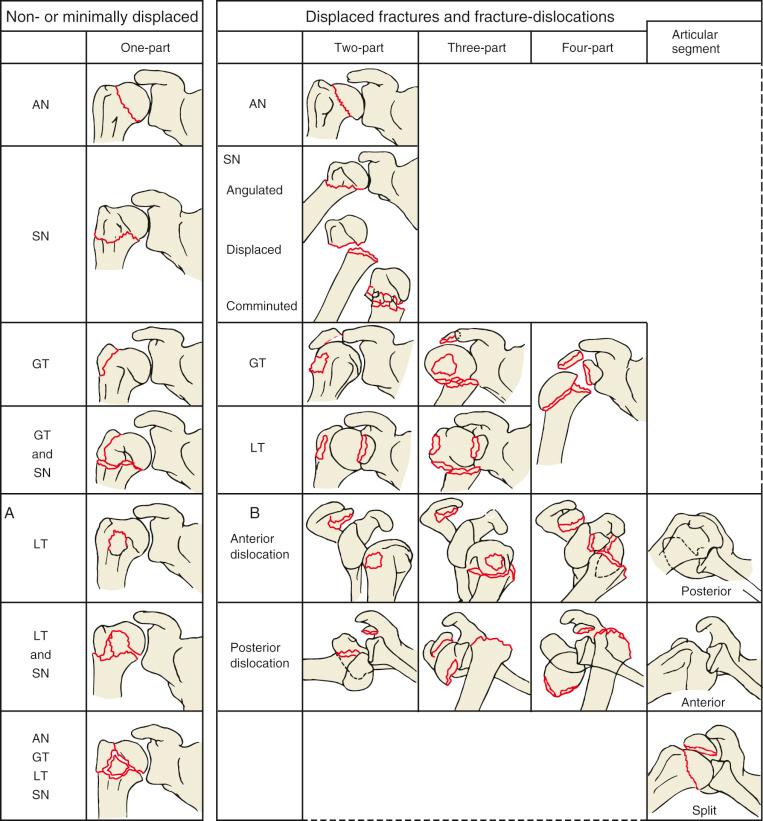
Group II, “articular-segment displacement,” included displaced fractures of the anatomic neck, which are rarely isolated but can occur as a “two-part” fracture when displaced more than 1 cm or 45 degrees. Usually, they are in relation with fractures of other segments. The displacement of the articular segment is determined by the severity of the injury rather than by any soft tissue attachments.
Group III, “shaft displacement,” consists of fractures of the surgical neck with displacement of at least 1 cm or 45 degrees regardless of additional fissures or minimally displaced fractures of the proximal segments. They represent the most common type of “two-part” fractures. Whereas the pectoralis major usually pulls the shaft fragment medially and in internal rotation, the intact rotator cuff insertions hold the head in neutral position.
Group IV, “greater-tuberosity displacement,” includes fractures or avulsions of the greater tuberosity with a separation of more than 1 cm. In a “two-part” greater tuberosity fracture, the tendons attached to the greater tuberosity pull it superiorly and posteriorly. The articular segment stays in a normal relationship to the shaft even though a minimally displaced surgical neck fracture may be present. In a “three-part” fracture (see Fig. 47.19 ), the greater tuberosity and the surgical neck may be displaced. Under these circumstances, the articular part with the intact subscapularis insertion is pulled in, internally rotated, and may face posteriorly.
In group V, “lesser-tuberosity displacement,” displaced fractures of the lesser tuberosity are included. The “two-part” lesser tuberosity fracture is rare and either an isolated avulsion of the subscapularis insertion or in combination with a minimally displaced surgical neck fracture. The head and shaft stay in a neutral position, and the subscapularis muscle pulls the lesser tuberosity fragment medially. In the “three-part” constellation (see Fig. 48.20 ), the lesser tuberosity and the surgical neck are displaced. The intact insertions of the supra- and infraspinatus and teres minor muscles pull the head in ER and abduction so that the articular surface may face anteriorly. A “three-part” fracture with the involvement of both tuberosities where the surgical neck stays in continuity has been described once in literature. This constellation usually results in a “four-part” fracture because the articular segment is detached from its basis, too (see Fig. 47.21 ). Under these circumstances, the tuberosities are displaced in the direction of their muscle pull, and the articular segment can either be impacted on the shaft or detached from any other segment with severe displacement.
In group VI, “fracture-dislocation,” Neer gathered all fractures that occur with a true dislocation. This included all aforementioned combinations of two- to four-part fractures with either anteroinferior or posterior dislocation. Later, he included displaced fractures of the articular surface (head impression or split) in this group. He explained that during the impaction of the humeral head against the glenoid, the impressed fracture part stays inside, and the other articular fragment is extruded from the joint.
The Arbeitsgemeinschaft für Osteosynthesefragen/American Society for Internal Fixation (AO/ASIF) organization proposed a new classification, which was an expansion and modification of the Neer classification. The main difference was that they paid special attention to the impaction or displacement of the fracture parts in a more detailed way to come up to the vascular impairment of the injury. Later, the valgus impacted fracture ( Fig. 47.25 ) was mentioned specifically, a special type of four-part fracture, which Jakob and colleagues analyzed in detail. Basically, the AO/ASIF system separates three types of fractures ( Fig. 47.26 ): extraarticular unifocal, extraarticular bifocal, and intraarticular. Each of these groups is divided into further subgroups depending on impaction and dislocation.

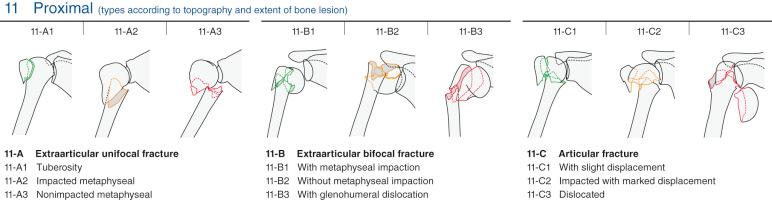
Type 11-A fractures involve one of the tuberosities or the surgical neck (“two-part” fractures). Type 11-A1 fractures are isolated greater tuberosity fractures with maximal displacement in the presence of fracture-dislocation (type 11-A1.3). Type 11-A2 fractures are impacted, and type 11-A3 fractures are nonimpacted surgical neck fractures.
Type 11-B fractures are extraarticular but involve the tuberosities with a concomitant surgical neck fracture (“three-part” fractures). Type 11-B1 are impacted, type 11-B2 are nonimpacted, and type 11-B3 are fracture-dislocations.
Type 11-C fractures are intraarticular with or without concomitant tuberosities or surgical neck fractures. In all 11-C types, the articular segment is separated from its vascular supply. Type 11-C1 are fractures with slight displacement, and type 11-C2 are “four-part” fractures and include impacted valgus (type 11-C2.1), varus (type 11-C2.2), and head-split (type 11-C2.3) types. Type 11-C3 represents articular segment fracture-dislocations (type 11-C3.1 is isolated anatomic neck without the involvement of the tuberosities, type 11-C3.2 is “four-part” anterior or posterior fracture-dislocation, and type 11-C3.3 is with extensive comminution of the humeral head).
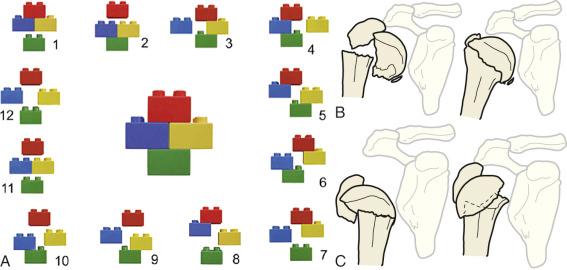
Based on the original drawings of Codman, Hertel and colleagues invented a “LEGO” classification system ( Fig. 47.27A ) with 12 basic fracture patterns (+2 additional head-split patterns). The vascular impairment was studied directly intraoperatively with the help of bore-hole bleeding and laser Doppler. They found that a dorsomedial metaphyseal head extension of less than 8 mm (see Fig. 47.27B ), a more than 2-mm disrupted medial hinge (see Fig. 47.27C ), and fractures with isolated articular segment were good predictors for intraoperative head ischemia. However, these findings did not correlate with postoperative avascular necrosis (AVN) in a later follow-up study. The authors concluded that both revascularization of intraoperatively ischemic and AVN of perfused heads may occur. They proposed that osteosynthesis may be worth a try even though the head is not perfused intraoperatively when patients have good bone stock and stable conditions for revascularization can be achieved.
Neer himself adapted his classification and abandoned the separation in six groups. He focused on the four segments and their displacement. The major modification was the use of a “one-part” fracture type despite the former group I. Therein all fractures with less than 1 cm or 45 degrees of displacement of any segment or combination of segments were included. The two- to four-part fractures were used as mentioned in his primary description (see the earlier section The Neer Classification ). Later, the valgus impacted four-part fracture was also included in this revised classification system. The adapted Neer classification has been used since its introduction and is still the most referenced classification for fractures of the proximal humerus. The AO/ASIF system, which is more detailed and also widely accepted, has not replaced the Neer classification.
However, the main limitation in the Neer classification is the measurement of 1 cm and 45 degrees on plain radiographs, which is fundamental for the decision whether a fractured segment becomes a “part” with subsequent surgical consequences. Therefore the reproducibility of the Neer classification was the subject of many studies. In most of these studies, the inter- and intrarater reliability were only moderate. The experience of the observer but also the quality of radiographs may be important. Also, the benefit of the addition of CT to plain radiography has been studied, and a slight increase in intraobserver, but none in interobserver, reliability was found.
Comparisons of the reliability of the AO/ASIF system with the Neer classification showed advantages for the latter. Brunner and colleagues could improve their inter- and intrarater reliability from moderate to good or excellent after the use of three-dimensional volume-rendered CT scans. Additional information from CT scans plays a more important role in modern fracture classification of the proximal humerus and has therefore been used in recent studies.
Recently performed prospective randomized studies on conservative versus operative fracture treatment in elderly patients with three- or four-part fractures showed no functional benefit of surgery. Therefore the discussion of fracture classification seems to become more and more secondary in at least this selected collective because the consequences for further treatment are questionable. However, in younger patients, the understanding of the fracture remains imminent to restore anatomic reduction and full shoulder functionality. Shrader and colleagues showed that the understanding of complex fracture types rather than their classification system should be enhanced. Therefore in the authors’ institution, CT scans are used for better understanding of fractures with subtle but potentially relevant displacement and for fractures with intended surgical treatment. Based on that, the authors use the Neer classification and pay additional attention to certain fracture types and configurations that have been found to behave in a special manner.
In an epidemiologic study on 1027 proximal humerus fractures, a 19% incidence of isolated greater tuberosity fractures was found. Thereof, 5% were fracture-dislocations according to AO 11-A1.3. These fractures need special mention because their treatment, and therefore their classification, is controversial. Neer suggested treating them operatively with more than 1 cm of displacement. Park and colleagues introduced a strategy that depends on the patient's activity level. He recommends surgical fixation in young and active patients with a displacement of more than 5 mm and in athletes and overhead laborers with more than 3 mm. This strategy has been supported by the findings of a biomechanical study performed by Bono and colleagues. They found significantly increased abduction forces of the deltoid muscle with a superior displacement of 5 mm and 1 cm. Also, other authors agreed with the surgical treatment with a displacement of more than 5 mm. However, the clinical studies on this topic are retrospective with several limitations. Also, Parsons and colleagues found difficulties in evaluating the exact displacement of the greater tuberosity on plain radiographs and recommended the use of an AP view with the arm in 30 degrees of ER. Depending on the radiographic projection, about 50% of their involved experts would have recommended surgery for 5-mm displaced fractures.
The evidence on this topic is not strong, and the treatment therefore mainly depends on the surgeon's preference. In active patients, the authors use CT scans to determine the exact direction and amount of displacement and consider arthroscopic or open surgical reduction in cases with more than 5 mm of displacement. In the case of conservatively treated patients with symptomatic malunion, greater tuberosity osteotomy has usually been performed. However, the authors also prefer arthroscopic resurfacing of the greater tuberosity with subsequent repair of the detached rotator cuff tendon as a valuable option.
Neer suggested osteosynthesis for three-part and primary hemiarthroplasty for four-part fractures, but Jakob and colleagues were the first who paid special attention to a valgus impacted four-part fracture pattern. After minimal osteosynthesis of 18 such cases, they found 74% good and 26% poor results that were related to AVN. They concluded that this four-part fracture type deserves special attention and must not be treated by prosthetic replacement. Also, Court-Brown and colleagues described a retrospective series of 125 elderly patients with three-part valgus impacted fractures. All patients were treated conservatively and reached 80% good or excellent results at 1 year. In their opinion, it would be difficult to reach better results with any surgical treatment. Therefore these fractures should be separated from other three- or four-part fractures. A possible reason for their special behavior could be the impaction, which makes them stable, and the often-intact medial hinge with preservation of the head perfusion.
Since Neer's definition of group VI fractures (see the earlier section The Neer Classification ) head-split and head-impression fractures are also mentioned together with fracture-dislocations. However, these injuries are relatively rare. Court-Brown and colleagues found rates of about 6% for anterior, 0.4% for posterior fracture-dislocations, and 0.7% for articular surface fractures. Neer proposed primary prosthetic replacement for four-part fracture-dislocations and articular fracture involvement of more than 50% of the humeral head. However, posterior fracture-dislocations should be mentioned separately. Despite their rarity, Robinson could describe a series of 26 younger patients with this injury. They were treated with ORIF and had excellent functional results after 2 years.
Special attention should be paid to locked anterior greater tuberosity and posterior lesser tuberosity fracture-dislocations because Hersche and Gerber described a series of these fractures with additional obscure anatomic or surgical neck fractures. During the reposition maneuver, the head fragment stayed in its primary locked anterior or posterior position. All of these patients developed AVN ( Fig. 47.28 ). Therefore the authors first rule out such an obscure fracture by CT scan when the radiograph is suspicious. When a neck fracture is excluded, a careful try of closed reduction under general anesthesia can be made. If a fracture of the anatomic or surgical neck is detected on the CT scan, one careful try of closed reduction under fluoroscopy can be done with standby for ORIF in the operating room. However, direct ORIF is the safest procedure in this situation.
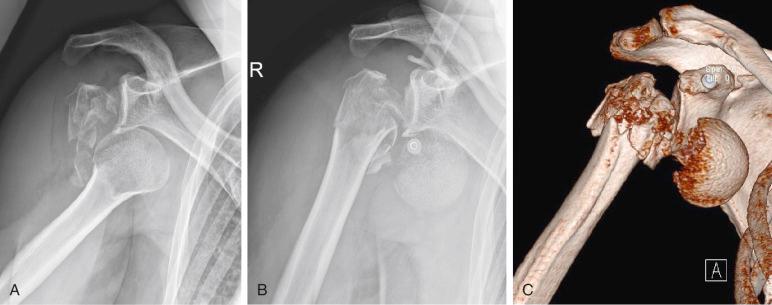
Despite voluminous literature on the treatment of fractures of the proximal humerus, there is still no standard of care, and a lot of controversies remain. The high variety of this injury, the difficult classification of the fractures, and the high number of treatment strategies with new implants (that are promoted by manufacturers) are possible reasons for these disagreements. Prospective randomized studies comparing different treatment options for specific fracture types are relatively rare, and the management and especially the surgical technique are mainly based on the surgeon's experiences and preferences. This section gives a general view on the nonoperative and operative management of fractures of the proximal humerus based on the actual literature, including the authors’ preferences at the end. General considerations, which should be considered for the decision-making process, are explained at the beginning. Open reduction techniques are described for different fracture types. Finally, the most commonly used surgical techniques are explained in detail and compared with one another based on the actual literature.
In a multiply injured patient, the treatment of a proximal humerus fracture is not of high priority (see Polytrauma Patient ). In an unstable patient, the arm can be temporarily fixed in a body bandage until the patient is stabilized. Fracture-dislocations should be reduced urgently because they can be associated with neurovascular impairment. Open fractures are rare and are treated with primary débridement, temporary or definitive fixation, and antibiotics (see Polytrauma Patient ). If a vascular injury is suspected, emergent angiography and vascular repair are recommended (see Vascular Injuries ). A nerve affection is generally not an indication for an emergent treatment because most nerve affections are due to traction injuries and resolve spontaneously. However, special care must be taken in case of high-energy trauma or worsening pain and nerve palsy. In such cases, vascular injury with subsequent damage to the brachial plexus must be suspected, and emergent angiography is indicated (see Nerve Injuries ).
The age and sex distribution and the high incidence of low-energy trauma underscore the role of osteoporosis in fractures of the proximal humerus. Low bone mineral density (BMD) has shown to be an important risk factor for fractures of the proximal humerus with significant influence on their treatment. Regarding this association, elderly patients with fractures of the proximal humerus should undergo a fragility workup, including an assessment of previous fractures in their skeletal history. Osteoporosis should be considered in the planning of the fracture treatment. Several options may be used to quantify osteoporosis in the proximal humerus. Tingart and colleagues introduced an expanded cortical thickness measurement concept that correlated to local BMD of the proximal humerus. On an AP-view radiograph, two levels were defined to calculate the cortical thickness. The first one is chosen at the level where the endosteal borders of the diaphyseal cortex become parallel and the second level is 2 cm distal to the first one. The combined cortical thickness is calculated as a mean of the medial and lateral cortical thickness at the two levels and adjusted for the magnification error of the radiograph ( Fig. 47.29 ). They found a combined cortical thickness of less than 4 mm to be a reliable and reproducible predictor for low BMD of the proximal humerus. In a later study, the combined cortical thickness showed a strong correlation to the dual-energy x-ray absorptiometry (DXA) of the femur and lumbar spine, which is the gold standard for the diagnosis of osteoporosis. However, the threshold value of 6 mm resulted in a sensitivity of 93% and a specificity of 53% for predicting osteoporosis. This threshold had a negative predictive value of 95% and was found to be useful for ruling out osteoporosis in this study. The authors use the 4-mm cutoff described by Tingart and colleagues because it correlates to the local BMD of the proximal humerus.
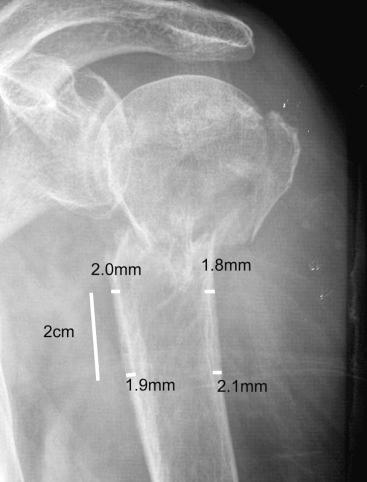
Peripheral quantitative CT (pQCT) also provides a good method to assess BMD of the proximal humerus, as shown by Krappinger and colleagues. This method can be combined with the CT scan, which is often used for definitive fracture classification and planning of surgery.
In a study performed in our institution, we defined the deltoid tuberosity index (DTI), a simple one-level measurement on the AP fracture radiograph. The index is calculated just proximal to the deltoid tuberosity, where the outer cortical borders become parallel for the first time. At this level, the outer cortical diameter is divided by the inner endosteal diameter, resulting in a ratio that does not need to be corrected for the magnification error ( Fig. 47.30 ). A further upside of this measurement is that this region of the humerus is barely involved in proximal humerus fractures. We found a very good correlation of DTI values of less than 1.4 with low bone quality of the humeral head measured on pQCT. Furthermore, we were able to prove the clinical relevance of low bone quality (DTI <1.4) for complications after angular stable surgical treatment of proximal humerus fractures.
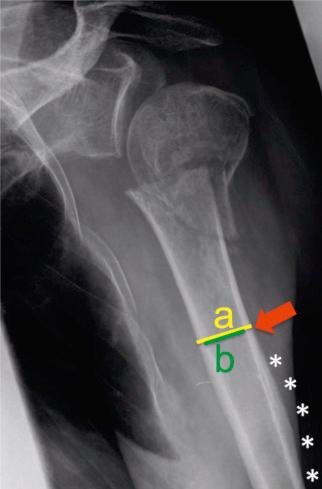
Since Neer suggested conservative treatment for one-part (non- or minimally displaced; see Fig. 47.24 ) fractures, they have been the scope of only a few studies. However, most found good functional results in the majority of the treated patients. For more complex fractures, Neer and other authors described the nonoperative treatment as unsatisfying, with a range of 47% to 61% of poor or unsatisfactory results, according to Neer's outcome criteria, especially for three- and four-part fractures. These studies, even though retrospective and mainly on a small number of patients with the same fracture types, supported the operative treatment of patients with three- and four-part fractures.
However, it might be due to relatively high complication rates after ORIF or to the consistently restricted functional results after fracture hemiarthroplasty that the conservative treatment has become the scope of more recent studies again. These studies mainly focus on older patients with special fracture types, and their findings are in contrast to the older studies mentioned earlier.
For example, Court-Brown and colleagues found 80% good or excellent results, according to Neer's outcome criteria, after conservative treatment of valgus impacted fractures. The mean age of their retrospectively studied 150 patients was 71 years, the mean Neer score was greater than 80 points, and the mean Constant score was between 65 and 73 points, depending on the fracture types. The amount of displacement had a negative influence on the final functional outcome after 1 year, and increasing age had a positive influence. The authors recommended conservative treatment for valgus impacted three-part fractures in elderly patients.
Recently published prospective randomized studies focused on the conservative treatment of all three- and four-part fractures. They mainly included patients older than 60 years, and none of these studies found any significant difference in the functional outcome compared with ORIF or hemiarthroplasty. In the studies performed by Olerud and colleagues, patients with valgus impacted three- or four-part fractures were not included because they were treated conservatively. Later, they treated patients operatively, when the surgical neck was completely displaced without bony contact. The conservatively treated patients with three-part fractures reached a mean Constant score of 58 points compared with 61 points in the ORIF group at 2 years of follow-up. The DASH score and the quality of life score (EQ-5D) were in favor of the ORIF group but did not reach significance, but the rate of complications and revisions was clearly worse after ORIF. The mean Constant score of conservatively treated patients with four-part fractures was 49 points and 48 points in patients with hemiarthroplasties. The quality of life score (EQ-5D) was found to be significantly better in the hemiarthroplasty group, in which pain relief and DASH scores were also favorable but not statistically significant. The authors concluded that the tendency of better functional results or quality of life after a surgical procedure of these fractures has to be balanced against the higher risk of revision rates. They found that the overall acceptable outcome and limited need for surgical intervention might justify a conservative treatment of elderly, low-demand patients with three- or four-part fractures ( Fig. 47.31 ).
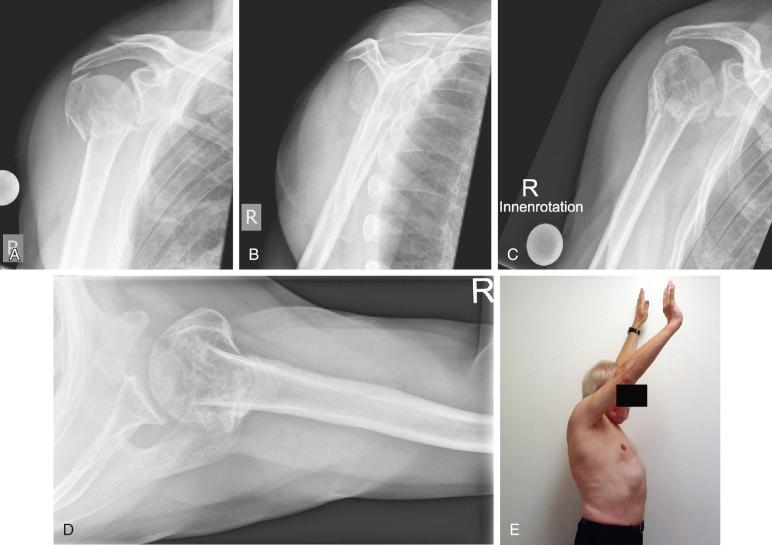
For young and active patients, the question arises of whether they tolerate less fracture displacement to regain full shoulder function and to return to work as quickly as possible. An analysis of studies with special focus on conservative treatment in younger patients showed a mainly successful outcome for one-part fractures ( Fig. 47.32 ). Furthermore, some other specific fracture types may be managed without relevant loss of functionality. However, the available studies on this topic are mainly based on retrospective data, and further prospective studies should give more information in the future.

Koval and colleagues studied 128 conservatively treated patients with stable one-part fractures. Their mean age was 63 years, ranging from 24 to 94 years. At a mean follow-up of 41 months, 77% achieved good or excellent results, with 88% of ROM compared with the uninjured shoulder. The clinical outcome was dependent neither on age nor on the amount of displacement of the greater tuberosity.
Hanson and colleagues retrospectively analyzed 139 conservatively treated patients with a mean age of 63 years, of which 35% were workers and 40% were active in sports, with perfect shoulder function before the injury. The included fracture types were 47% one-part fractures, 36% two-part fractures, and 17% four-part fractures, mainly with the involvement of the greater tuberosity and the surgical neck. Four patients dropped out of surgery because of secondary displacement, and five patients were treated with secondary arthroscopy because of impingement. At the 1-year follow-up, the union rate was 93%, and the mean Constant score was 80 points, without a difference for one- or two-part fractures. They found a not-significant tendency of worse results for three- and four-part fractures. Of special interest was that 41 of 42 laborers returned to work between 8 and 16 weeks. The authors concluded that conservative treatment is safe and effective in type 11-A and 11-B fractures.
Court-Brown and colleagues retrospectively described the outcome of 135 conservatively treated patients with varus impacted surgical neck fractures (type 11-A2.2). Their collective included 23% of patients younger than 60 years. All fractures healed, and 79% showed good or excellent functional results independent of the final varus angle. The only predictor for limited function was increasing age.
Lefevre-Colau showed in his prospective randomized controlled trial (RCT) that physiotherapy with early mobilization is safe for conservative treatment of patients with stable impacted proximal humeral fractures. He compared a “conventional” treatment with 3 weeks of immobilization in a sling with an “early-mobilization” protocol, in which the patients wore a sling for 4 to 6 weeks and started physiotherapy after 3 days with pendulum and passive ROM exercises. After 6 weeks, they started with active ROM exercises. Compared with the conventional group, the patients in the early-mobilization group had significantly better Constant scores at the 3-week and 3-month follow-ups. However, at the final follow-up of 6 months, the scores were still better but no longer statistically significant.
In case of unstable fracture, the arm can be immobilized in a sling for 2 weeks. Then physiotherapy may be started with pendulum exercises and passive elevation and abduction up to 90 degrees. After 4 to 6 weeks, patients can be allowed free active ROM. In case of severe surgical neck displacement and intended conservative treatment, the head and shaft alignment may be corrected by closed reduction under general anesthesia. Depending on the preferred arm position for optimal reduction, a sling with a pillow in the axilla or even an abduction brace can be used for immobilization. If consolidation is uncertain after 2 weeks, the fracture can be examined under fluoroscopy to see if the head and shaft rotate as one unit.
For one-part fractures, the most frequent complication is limited ROM, especially internal and ER. Markedly limited shoulder function, mainly caused by stiffness, has occurred in up to 10% of patients. However, nonunion and AVN are very rare and have not been found in two large series. Conservatively treated two- and three-part fractures can result in impingement, nonunions, and AVN, but the rate of these complications depends on the primary stability of the fracture type. Initial manipulations and smoking are predictors for nonunions in nonoperatively treated patients.
After the indication for a surgical treatment is made, the preoperative planning consists of a full understanding of the fracture pattern, maybe with the help of an additional CT scan. Furthermore, the surgeon should be experienced with variable devices because the treatment may change during surgery (e.g., when internal fixation is not stable enough and primary arthroplasty is needed). For most cases, an interscalene block with or without general anesthesia is preferred. Good muscle relaxation is helpful for fracture exposure and reduction. If general anesthesia is precluded for medical reasons in an elderly patient, the operation can be done with an interscalene block alone.
There are mainly two important surgical approaches to the proximal humerus. The first is the deltopectoral approach, which includes the internervous plane between the pectoralis major and the deltoid muscle. The second is the superior approach through the deltoid muscle. They are discussed in detail in the first part of this chapter.
Acute displaced greater tuberosity fractures can be approached through either a deltopectoral or a superior deltoid-splitting approach. The former approach facilitates access to the surgical neck and is especially helpful if the greater tuberosity fragment is long. Although it would appear to be difficult to reach a posteriorly retracted greater tuberosity from the deltopectoral approach, this is not usually a problem. Sequential placement of traction sutures (nonabsorbable heavy braided suture) in the supra- and infraspinatus tendons provides a handle for manipulating, mobilizing, and reducing the greater tuberosity. If the biceps tendon is involved and dislocated, it can be cut at its origin through the longitudinal cuff tear or through the interval. In young patients, a tenodesis with suture anchors can be made distal to the fracture in the bicipital groove. The humerus is rotated and abducted to allow anatomic repositioning of the fragment. When brought in anatomic position, the fragment can be fixed with two screws if it is big enough. If comminuted, a buttress plate can be used and the fragment additionally fixed to the plate with the placed traction sutures.
Displaced lesser tuberosity fractures are exposed through the deltopectoral approach. The conjoined tendon and coracoid process are left in place. Special care is taken to preserve the anterior circumflex humeral vessels and protect the axillary nerve at the inferior border of the subscapularis. Nonabsorbable heavy braided sutures are placed through the subscapularis insertion around the lesser tuberosity. The tuberosity and subscapularis muscle are mobilized sufficiently to allow easy reduction and preservation of shoulder ER. The treatment of a possibly involved biceps tendon is equivalent to the technique described earlier for greater tuberosity fractures. Heavy, braided nonabsorbable suture is passed through drill holes in the fracture bed and laterally out either through the biceps groove or the greater tuberosity. The rotator cuff interval can be repaired laterally. Also, screw fixation can be used.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here