Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Radiotherapy is used as one of the major treatment modalities for patients with malignant diseases at different disease stages. Currently, the most common radiation choice for the majority of cancers is photon (x-ray)-based intensity-modulated external beam radiotherapy. Notably, recent advances in technology and basic and clinical research have facilitated the safe delivery of more effective and noninvasive radiotherapy for malignant diseases using charged particles, including intensity-modulated proton therapy. Proton beams deliver most of their energy at the distal edge of their range (the Bragg peak), which leads to an increase of the radiation doses to the clinical targets and minimization of the irradiation dose to adjacent normal tissues. Moreover, photon beams are categorized as low linear energy transfer (LET), whereas proton beams, especially in the spread-out Bragg peak (SOBP), which majorly contains Bragg peaks, are categorized as high LET. Thus in addition to the physical dose distribution advantage, proton therapy also presents distinct biology advantages compared with photon radiation. Even though the biological features of tumors and normal tissues after photon radiation have been extensively studied, the biological responses of tumors and normal tissues to proton radiation are far from clear. The biological properties of proton beams that differ significantly from those of photons will be summarized in this chapter. Particular emphasis is placed on relative biological effectiveness (RBE), DNA damage, and repair effects induced by protons, proton beam–induced cell death mechanisms, the impact of proton beams on tumor immune responses, and the influence of proton beams on tumor angiogenesis.
DNA is the critical target of radiation. Photon radiation induces DNA damage by the direct action of deposing beam energy to DNA. Photon radiation also induces DNA damage by the indirect action of forming reactive species near the DNA, primarily by turning a water molecule into a free radical (hydroxyl radicals, OH). Photon radiation causes many types of DNA damage, including single-base damage and single-strand breaks (isolated), and clustered base damage and double-strand breaks (DSBs) (clustered within a few DNA helical turns). Most single-strand breaks can be repaired normally. However, repair is more difficult, and erroneous rejoining of broken ends in DSBs may result in significant biological consequences. Failure of DNA DSBs repair results in induction of mutations, chromosome aberrations, cell death, or even possibly in malignant cell transformation. It is believed that the complexity of DNA damage is the determining factor for the consequent cellular response to radiation.
Although photon radiation–related DNA damage and repair researches have been conducted extensively, the DNA damage and repair as a consequence of proton radiation remain poorly understood. Similar to that of photon radiation, it has been proven that the indirect effect of proton beams plays a major role and causes a large proportion of DNA damage compared with the direct effect of proton beams. , However, Monte Carlo simulations have indicated that the average number of DNA damages per cluster tends to increase with the increasing of the radiation beam LET, which implies a higher level of DNA damage complexity induced by proton beams versus by that caused by photon beams. , These mathematical model prediction results have been verified by several other studies by testing DNA plasmids or cell lines. Using DNA plasmids pBR322 or T7 as testing material, the direct damage effect of proton beams to DNA was proven to generate more DSB clusters compared with non-DSB clusters compared with photon beams. , Similar observations were also demonstrated in cell-based studies. An increased complexity of DNA damages and slower DNA damage repair kinetics were observed in the human skin fibroblast AG01522 cells at the distal end of the SOBP after proton radiation. Other than this, large foci, which represent the DSB clusters, were also found more commonly in Chinese hamster ovary (CHO) cell lines CHO10B2 and irs-20 after proton radiation compared with photon radiation. The more severe DNA damage caused by proton beams were also proven by another study on the thyroid-stimulating hormone–dependent Fischer rat thyroid cells. The authors found more free-end DNAs 1 hour after proton radiation than photon radiation, which means a more rapid DNA damage repair in the cells exposed to photon beams than those exposed to proton beams. They further verified their results by finding a higher rate of micronucleus formation and the presence of larger micronuclei in cells treated by proton beams than those cells treated with photon beams. Persistent DNA damage was also observed in different head and neck cancer cell lines after exposure to proton beams versus exposure to photon beams. However, conflicting results were observed in a study using the DNA plasmid pBR322. In this study, the authors did not find a difference in the amount of the clustered DNA damage induced by proton beams compared with photon beams in either the liquid or in the dry samples.
Because DNA DSBs are the key lesion leading to severe biological consequences in cells exposed to photon radiation, it is meaningful to study DSB and its processing after cells are exposed to proton beams. Because the DNA damages induced by proton beams are with higher complexity than those induced by photon beams, the repair of the damaged DNA caused by proton beams may be different from the repair of damaged DNA caused by photon beams. Compared with the extensively studied DNA damage repair mechanisms after photon beam exposure, the study of DNA damage repair after proton beam radiation is limited, and mechanisms underlying the DNA damage repair are still to be uncovered.
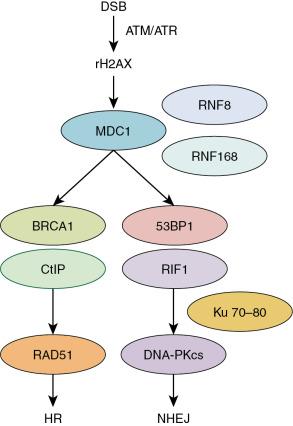
There are two major distinguished DSB repair pathways ( Fig. 1.1 ): homologous recombination (HR) and nonhomologous end joining (NHEJ). NHEJ is active throughout the cell cycle and is the predominant repair pathway for photon radiation–induced DSBs in mammalian cells. , The roles of HR and NHEJ in DNA damage repair in response to proton versus photon beams have been studied. In this study, the CHO cells AA8, CHO9, UV5, Irs1sf, and XR-C1 with different Rad51 (a protein related to HR , ) and DNA-PKcs (a protein related to NHEJ , ) status were exposed to proton or photon beams. Cell survival and DSB repair were evaluated after radiation. The authors found that when compared with wild-type cells, Rad-51-deficient or suppressed cells have a higher proton versus photon radiation response rate; however, DNA-PKcs-deficient cells have not shown a different response rate to proton versus photon radiation when compared with wild-type cells. Moreover, delayed DSB repair was also found in the Rad-51-deficient cells after proton radiation. The authors concluded that HR is preferentially required for proton beam–induced DSB repair. A similar phenomenon was also found in human lung adenocarcinoma (A549) and human glioblastoma (M059K and M059J) cells. In this study, after blocking DNA-PKcs, a higher level of delayed DSBs repair and a more profound radio response was observed after cells were exposed to photon versus proton beams. On the other hand, depleting RAD51 led to an enhanced response of A549 cells to proton beams. The authors claimed a preference of HR versus NHEJ in proton beam–induced DSB repair. On the contrary, conflicting results were reported by others. In one study, the authors compared the DSB repair of the DNA-PKcs wild-type CHO cell line CHO10B2 with its derived radiosensitive mutant cell line, the DNA-PKcs-deficient cell line irs-20 after cells were exposed to photon and proton beams. Irs-20 cells presented more persistent DSBs compared with CHO10B cells after cells were exposed to both photon and proton beams. A dependence on the DNA-PKcs in repairing DSBs caused by both proton and photon beams was verified. In another study involving the DNA-PKcs wild-type CHO cell line CHO10B2, Ku80-mutated CHO mutant cell XRS-5, DNA-PKcs null V3 cells, Rad51D-mutated 51D1 cells, and 14 cell lines derived from V3 cells with complementary human DNA PKcs containing amino acid substitutions at specific positions, the cell responses to proton beams versus photon beams were not correlated with the status of DNA-PKcs or RAD51; thus, no preferential DSB repair pathway of HR or NHEJ was observed in proton beam–induced DSB repair. Other than the previously mentioned, a study using cervical cancer HeLa cells claimed that the higher cell response rate of proton beams versus photon beams in the SOBP is in an Artemis protein–dependent manner. Because Artemis protein is a member of the NHEJ pathway, this result reflects the dependency of the repair of proton beam–induced DSBs on NHEJ. Some other studies also demonstrated the preference of the NHEJ pathway in the repair of DSBs induced by proton beams. , This evidence includes the activation of Ataxia-Telangiesctasia mutated (ATM, contributing to NHEJ ) and DNA-PKcs but not ataxia telangiectasia and Rad3 related (ATR) by proton beams in human lung adenocarcinoma A549 cells and the induction of ATM by proton beams in human prostate cancer PC3 cells.
Taken together, the overall DNA damage caused by proton is different than that of photon beams, at least to a certain extent. However, the repair mechanisms of the DSBs induced by proton beams are still unclear. Future studies specifically investigating the DNA repair pathways of proton beams will translate the findings into biology-based rationales of treatment selection between proton- and photon-based radiation and the combination of therapies that targeted specific signal pathways.
One of the severe consequences of the failure of DNA damage repair induced by radiation is cell death. The mechanisms of photon radiation–induced cell death are intensively studied. Photon radiation is known to kill cancer cells via apoptosis, necrosis, autophagy, mitotic catastrophe, and senescence. However, the mechanisms by which proton radiation induces cell death are unclear.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here