Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Caring for the unilateral cleft lip patient extends far beyond primary cleft lip repair. The complex needs of the cleft patient and family evolve as the child ages; therefore, a longitudinal multidisciplinary team approach is obligatory for proper care. In this chapter we present our preferred technique for repair of the unilateral complete and incomplete cleft lip deformity.
Unilateral cleft lip is the congenital separation of the upper lip that, to varying degrees, also affects the nose and underlying alveolus. Cleft lip with or without cleft palate is the most common congenital facial defect, affecting 1 : 690 U.S.-born children. Males and people of Asian and Native American descent are more commonly affected. Unilateral cleft lip can be classified as:
microform (i.e., forme fruste ): discontinuity of the vermilion cutaneous junction with a less than 3-mm difference in the subnasale to Cupid's bow peak distance between sides, variable deficiency of vermilion medial to cleft, variable muscular depression along the philtral line, subtle nasal asymmetry, and variable alveolar defect.
minor form: greater than 3-mm difference in the subnasale to Cupid's bow peak distance between sides, discontinuity of the orbicularis oris with more prominent depression of the philtral line, increased nasal asymmetry with posteroinferior displacement of the cleft side piriform aperture, and alveolar cleft.
incomplete: full-thickness separation of the upper lip with a continuous, though depressed, nasal sill and floor ( Fig. 3.1.1 ).

complete: full-thickness separation of the lip extending into the nasal cavity and discontinuity of the alveolus ( Fig. 3.1.2 ).

This chapter focuses on surgical repair of the incomplete and complete unilateral cleft lip deformity.
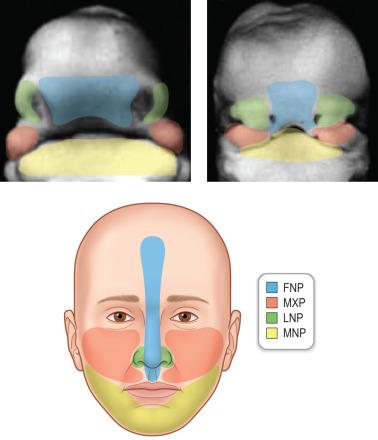
Unilateral cleft lip results from failure, or partial fusion, of the frontonasal and maxillary prominence between 4 and 7 weeks of gestation ( Fig. 3.1.3 ). Several teratogens including phenytoin and maternal smoking have been associated. Van der Woude syndrome is the most commonly associated syndrome; however, incompletely understood non-syndromic genetic associations are far more common.
A multidisciplinary cleft team including a plastic surgeon, otolaryngologist, orthodontist, speech pathologist, audiologist, social worker, and photographer evaluates the patient and family. Programs in developing countries should strive to use this team approach. A thorough history and physical examination is performed. Clinical findings help determine whether there is a need for pre-operative nasoalveolar molding (NAM). Surgical repair is typically performed at 3 months of age; however, this may be delayed as a result of pending completion of NAM or need for medical optimization in patients with comorbid conditions. The “rule of 10's” is a frequently quoted minimum safety cutoff of age (10 weeks), weight (10 kilograms), hemoglobin (greater than 10) before undergoing lip repair. This is not substantiated by recent evidence, and repair may proceed despite failure to meet all criteria if a full preoperative evaluation has been performed.
Unilateral incomplete and complete cleft lip anatomical derangements are complex ( Fig. 3.1.1 and 3.1.2 ) and involve the skin, muscle, nasal cartilage, and bony maxilla. The relevant anatomy includes the following:
There is deficient vertical height of the cleft side lip—this involves both the external skin and intraoral mucosa.
The orbicularis oris is in discontinuity, with abnormal insertion of the greater (i.e., medial) segment pars peripheralis into the anterior nasal spine and abnormal insertion of the columellar base and lesser (i.e., lateral) segment into the alar base and piriform aperture periosteum.
The lesser alveolar segment is retropositioned, and the greater alveolar segment is anteriorly rotated. Extrinsic forces of the tongue and cheek and abnormal insertions of the orbicularis oris likely contribute to this.
The cleft-side piriform aperture is posteroinferiorly displaced with decreased projection of the midface on the cleft side.
The columella is asymmetrically shortened (cleft side shorter than non-cleft side) with deviation of the columellar base toward the non-cleft side.
The nasal tip is rotated toward the cleft side.
The caudal septum is displaced out of the vomerine groove into the non-cleft side.
The septum is convex on the cleft side, projecting into the cleft nasal vestibule.
The cleft side lower lateral cartilage has a shortened medial crus resulting in retroposition of the cleft-side nostril dome, an elongated and flattened lateral crus resulting in widening and posterior displacement of the cleft nostril sill, and an obtuse angle of the cleft side nostril dome.
There is deficient cleft nostril vestibular lining.
There is vestibular webbing of the lateral cleft nostril.
Finally, there is an ill-defined cleft-side alar-facial groove.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here