Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Primary brain tumors account for nearly 20% of all malignancies during childhood and adolescence worldwide, with an age-standardized incidence rate of 28.2 per million persons ( ; ). These tumors are second only to leukemia in frequency among all childhood cancers and are the most common solid tumor in children ( ; ). The location, histological features, prognosis, and treatment of pediatric brain tumors are different from those of adult brain tumors and vary significantly according to age within the pediatric population ( Table 75.1 ). The location of approximately 30% of primary brain tumors in children aged 0–14 years is the posterior fossa; however, supratentorial brain tumors are the most common location in adolescents and children younger than age 2 ( ). Gliomas account for approximately half of pediatric central nervous system (CNS) tumors of which the majority are pilocytic astrocytomas (PAs) and other low-grade gliomas. In contrast to adult brain tumors, supratentorial high-grade astrocytomas (HGAs) represent only 6%–12% of all primary pediatric brain tumors, and diffuse intrinsic brainstem gliomas represent 10%. Embryonal tumors (14.5%), other gliomas (15%), ependymomas (6.5%), germ cell tumors (4.6%), and craniopharyngiomas (3%) account for most of the other types ( ). Despite significant improvements in prognosis for many pediatric cancers over the past few decades, CNS malignancies remain a major cause of morbidity and mortality. However, the pace of both clinical and laboratory research has accelerated over the past decade, and classification and management of this diverse group of tumors is undergoing a transformation owing to a new understanding of brain tumor biology and genomics on a molecular level ( Table 75.2 ) .
| Histology | Percent of All Tumors | Median Age | Rate∗ |
|---|---|---|---|
| Gliomas | 52.90 | 6 | 2.78 |
| Pilocytic astrocytoma | 17.60 | 7 | 0.93 |
| Other low-grade glioma | 14.30 | 6 | 0.75 |
| High-grade glioma | 11.10 | 7 | 0.59 |
| Ependymal tumors | 5.50 | 4 | 0.29 |
| Other glioma | 4.40 | 7 | 0.23 |
| Choroid plexus tumors | 2.30 | 1 | 0.12 |
| Tumors of the pineal region | 4.40 | 6.5 | 0.23 |
| Neuronal and mixed neuronal-glial tumors | 0.90 | 9 | 0.05 |
| Embryonal tumors | 15.00 | 4 | 0.79 |
| Medulloblastoma | 9.30 | 6 | 0.49 |
| Primitive neuroectodermal tumor | 2.20 | 3.5 | 0.12 |
| Atypical teratoid/rhabdoid tumor | 2.30 | 1 | 0.12 |
| Other embryonal tumors | 1.20 | 1 | 0.06 |
| Tumors of cranial and spinal nerves | 4.70 | 7 | 0.25 |
| Tumors of meninges | 2.90 | 9 | 0.15 |
| Lymphomas and hematopoietic neoplasms | 0.40 | 6 | 0.02 |
| Germ cell tumors | 3.70 | 9 | 0.19 |
| Tumors of the pituitary | 3.90 | 12 | 0.2 |
| Craniopharyngioma | 4.00 | 8 | 0.21 |
| Other/unclassified tumors | 4.90 | 9 | 0.26 |
| TOTAL † | 100.00 | 7 | 5.26 |
∗ Rates are per 100,000 and are age-adjusted to the 2000 US standard population.
† Refers to all brain tumors including histologies not presented in this table.
| Tumor Type | Molecular Subgroups | Main Genetic Alterations | Common Germline Predisposition |
|---|---|---|---|
| Medulloblastoma | WNT | SNV— CTNNB1, TP53, CNV—Monosomy 6 | Familial adenomatous polyposis |
| SHH | SNV— PTCH, SUFU, TP53, TERT, SMO CNV— GLI2, MYCN | Gorlin syndrome, Li-Fraumeni syndrome | |
| Group 3 | CNV— MYC | ||
| Group 4 | CNV— MYCN, CDK6, SNV— KDM6A | ||
| Embryonal tumors | ETMR | CNV—C19MC amplification, SNV - Dicer1 | |
| Embryonal—NOS | CNV—FOXR2 fusions, MN1 rearrangements, BCOR alterations, CIC fusions | ||
| ATRT | ATRT-MYC, ATRT-TYR, ATRT-SHH | SMARCB1 deletions, mutation; SMARCA4 mutations | Rhabdoid predisposition syndrome |
| High-grade glioma | DIPG/DMG | Histone H3.1 and 3.3 K27M substitution (H3K27M) | |
| Anaplastic astrocytoma/glioblastoma | SNV—Histone H3.1/3.3 G34V/R or K27M substitution, BRAF V600E, IDH1 CNV— NTRK, ALK and MET fusions Hypermutation/mismatch repair deficiency |
Constitutional mismatch repair deficiency (cMMRD), Li- Fraumeni syndrome | |
| Low-grade glioma | Pilocytic astrocytoma | SNV—BRAF V600E Germline— NF1 CNV— KIAA1549-BRAF fusion, FGFR-TACC fusions/duplication |
Neurofibromatosis type 1 |
| Diffuse astrocytoma | SNV—BRAFV600E, FGFR1/2/3 , H3K27M, IDH1 CNV— KIAA1549-BRAF, MYBL fusions |
||
| Ganglioglioma/desmoplastic infantile astrocytoma | BRAF V600E mutations | ||
| Dysembryoplastic neuroepithelial tumor | FGFR mutations | ||
| Pleomorphic xanthoastrocytoma | SNV—BRAFV600E CNV— CDKN2A deletion |
||
| Subependymal giant cell astrocytoma | TSC1, TSC2 | Tuberous sclerosis | |
| Ependymoma | PF-EPN-A | SNV— EZHIP/CXorf67 CNV—1q gain |
|
| PF-EPN-B | CNV—numerous arm level gains and losses | ||
| ST-EPN-RELA | Fusions of C11orf95-RelA, fusions on chromosome 11 | ||
| ST-EPN-YAP1 | Fusions of YAP1-MAMLD1 | ||
| Craniopharyngioma | Adamantinomatous | CTNNB1 mutations | |
| Papillary | BRAF V600E |
Medulloblastoma is a round blue cell tumor of the cerebellum and/or fourth ventricle, and is the most common malignant brain tumor of childhood. The World Health Organization (WHO) recognizes the medulloblastoma with five distinct molecular variants, termed subgroups: specifically, Wingless-activated (WNT), SHH-activated TP53 wild-type (SHH-TP53WT), SHH-activated TP53 mutant (SHH-TP53 mutant), and non-WNT/non-SHH comprising two provisional entities, Group 3 and Group 4 ( ). The WHO also recognized histological variants defined as: large-cell medulloblastoma, anaplastic medulloblastoma, medulloblastoma with extensive nodularity, and desmoplastic/nodular medulloblastoma. Medulloblastoma represents approximately 65% of CNS embryonal tumors and 10% of all pediatric brain tumors. The incidence in males is twice that of females, and the median age at diagnosis is 5–7 years. Taken as a group, 80% of all CNS embryonal tumors are diagnosed before age 10. According to the incidence data generated by the National Cancer Institute’s Surveillance, Epidemiology and End Results (SEER) registry and the CNS Tumors Diagnosed in the United States, the incidence of CNS embryonal tumors and medulloblastoma has remained fairly stable over the past 20 years ( ; ).
Although they are morphologically similar, integrated genomics have shown that medulloblastoma actually comprise four molecular variants, each with distinct signaling pathways that control brain development owing to different cells of origin ( ; ; ). These four molecular variants termed subgroups, are named WNT, SHH, Group 3 and Group 4 and have distinct demographics, genetics, and outcomes, and are now considered separate entities warranting dedicated approaches ( ). Approximately 10% of medulloblastoma patients have a germline predisposition, with highest incidence in children with SHH-activated medulloblastoma ( ).
The WNT tumors comprise 10%–15% of patients and are found most often in children and adults, occur equally in males and females, rarely metastasize, and are associated with an excellent prognosis ( ; ). They arise from the lower rhombic lip of the developing brainstem, and frequently invade the cerebellopontine angle ( ; ). The cytogenetic abnormality most commonly associated with this subgroup is monosomy of chromosome 6 and nearly all tumors have a somatic mutation the gene encoding beta-catenin (CTNNB1) ( ; ). These tumors almost always have nuclear immunohistochemical staining for beta- catenin, which signifies activation of the WNT pathway, although this marker should never be used in isolation due to the risk of false positives ( ). Germline adenomatous polyposis coli (APC) mutations arise in 10% of WNT patients and are mutually exclusive from CTNNB1 mutations. As such, all patients without a somatic mutation in CTNNB1 require referral to a genetic counselor for germline testing for APC ( ). WNT tumors in patients under age 16 have an excellent prognosis across many studies, and currently several trials are ongoing evaluating de-escalation of radiotherapy ( ). The gold standard for diagnosis of a WNT-activated medulloblastoma is demonstration of an activating mutation in exon 3 of CTNNB1 , with confirmation using a second method including immunohistochemistry, gene expression profiling, or DNA methylation profiling ( ).
Approximately 20%–25% of patients with medulloblastoma activation of the SHH pathway, where the majority have events such as mutations or amplifications, of which 20% are germline events ( ; ; ). The SHH pathway is critically involved in the normal development of the cerebellum and SHH-activated medulloblastoma arise from the external granule layer of the cerebellum ( ; ; ). Mutations in the SHH pathway can be either somatic or germline. The PTCH gene is the most commonly affected gene within this pathway, but mutations in other genes along this pathway including smoothened, fused, and suppressor of fused (SUFU) have also been identified ( ). Germline mutations in PTCH are associated with nevoid basal cell carcinoma syndrome, also known as Gorlin syndrome , and occur in 10%–15% of infants with SHH medulloblastoma with an excellent prognosis ( ; ). This gene encodes for the protein that is the receptor of SHH. Gorlin syndrome is an autosomal dominant disorder characterized by the development of basal cell carcinomas, multiple bony cysts, and malignant tumors including medulloblastomas in young children. Germline SUFU mutations can result in a Gorlin-like syndrome and possibly portend a worse prognosis ( ). SUFU is a suppressor of SHH signaling, downstream of PTCH and Smoothened. Older children (4–16 years) harbor germline mutations in the tumor suppressor TP53 in 15%–20% of SHH-activated medulloblastomas, as part of the Li-Fraumeni syndrome (LFS). These patients have a very poor prognosis, and frequently have concurrent amplifications of MYCN and GLI2 , with many somatic copy number changes observed, frequently harboring chromothripsis (chromosome shattering) ( ). All patients with SHH medulloblastoma should be referred to a geneticist for testing of germline ( ; ).
SHH medulloblastoma are composed of four subtypes identified using integrated genomics, two observed in infants (SHHβ/SHH-I and SHHγ/SHH-II), one in the childhood age group (SHHα) and one adult group (SHHδ) ( ). Infant SHH tumors are divided into two groups, whereby SHHβ/SHH-I have a frequent gain of chromosome 2p, PTEN loss, SUFU mutations, and a poor prognosis, whereas SHHγ/SHH-II have a blander genome and an excellent prognosis ( ; ). SHHα comprise the childhood age group, where TP53 mutations (somatic or germline), MYCN amplification, GLI2 amplification are common, and those with TP53 mutations have a poor prognosis ( ). SHHδ are primary adult-type medulloblastoma, and frequently harbor TERT promoter mutations and have an intermediate outcome ( ; ) Nearly all desmoplastic, nodular medulloblastomas are found within the SHH subgroup, although only about 50% of SHH medulloblastomas have this histology, with the remaining tumors having either classic or large-cell anaplastic histology. Within adults, SHH comprise almost 70% of all medulloblastomas. Overall, metastasis at diagnosis is much less common in SHH tumors. At relapse SHH tumors recur in the surgical cavity in 50%–60% of cases ( ; ).
Group 3 tumors comprise approximately 25% of medulloblastoma and usually occur in children and infants, are rarely observed in adults, have a 3:1 male:female ratio, harbor classic or large-cell anaplastic histology, metastasize in up to 50%, and have a poor prognosis ( ). Postnatal cerebellar progenitor cells are candidate cells of origin for this subgroup ( ; ; ). These tumors often have overexpression and amplification of the MYC oncogene, and activation of the GFI family of oncogenes ( ; ). Group 3 medulloblastomas recur almost exclusively with metastatic dissemination, particularly those children who are previously radiated ( ). Germline predisposition is rare in Group 3; however, 1%–2% of patients have germline mutations in the Fanconi anemia/BRCA pathway, and should be suspected in those patients with significant treatment-related toxicity or suggestive family histories ( ).
Group 4 is the most common subgroup, and comprises 40%–45% of medulloblastomas in children aged between 4 and 16, and 10%–15% of adults ( ). There is a 3:1 male to female incidence, and between 30% and 35% of patients have metastasis at diagnosis. Group 4 medulloblastoma arises from the unipolar brush cells of the developing cerebellum, and transcriptionally have activation of glutaminergic pathways ( ; ). Somatic nucleotide events in KDM6A have been observed to be a recurrent event in 10% of cases, with MYCN or CDK6 amplifications observed in 15%–20% of cases. The most common cytogenetic aberration is isochromosome 17q, observed in almost 80%. Whole-chromosome loss of chromosome 11 or gain of chromosome 17 and 10p loss have been found to be associated with better survival within group 4 ( ; ; ). Additional heterogeneity has been observed within Groups 3 and 4, and the clinical relevance of this is currently being validated in prospective studies ( ). Group 4 medulloblastoma patients who have received radiotherapy recur almost exclusively with metastatic leptomeningeal dissemination, with the surgical cavity almost always devoid of tumor ( ). In addition, late relapses are more frequently observed in Group 4, including after 5 years. Relapses in the surgical cavity in irradiated patients should prompt a suspicion for radiation-induced glioblastoma rather than medulloblastoma recurrence ( ; ).
Many of the clinical manifestations of a medulloblastoma that arises in close proximity to the fourth ventricle are the result of increased intracranial pressure (ICP) due to obstructive hydrocephalus. Headache, vomiting, and ataxia are the most common initial symptoms and usually precede diagnosis by 2–8 weeks. Intractable nausea and vomiting occur frequently, characteristically in the morning. Personality changes, namely irritability, are an early feature, especially in infants, but may be difficult to recognize as a sign of a brain tumor. Other features that can lead to diagnosis include lethargy, diplopia, head tilt, and truncal ataxia. Interestingly, a longer time to diagnosis portends to an improved survival, which is related to a strong subgroup specificity ( ).
Although contrast-enhanced magnetic resonance imaging (MRI) identifies leptomeningeal metastases in 20%–30% of children with medulloblastoma at the time of diagnosis, clinical manifestations are uncommon. Back pain and radicular pain indicate the rare complication of spinal dissemination. Less commonly, intratumoral hemorrhage may lead to acute onset of confusion, headache, and loss of consciousness. Among infants with posterior fossa tumors, diagnosis can be more challenging; thus, important features include changes in mood and personality as well as macrocephaly. Delay in achieving milestones or loss of previously achieved milestones and failure to thrive are characteristic.
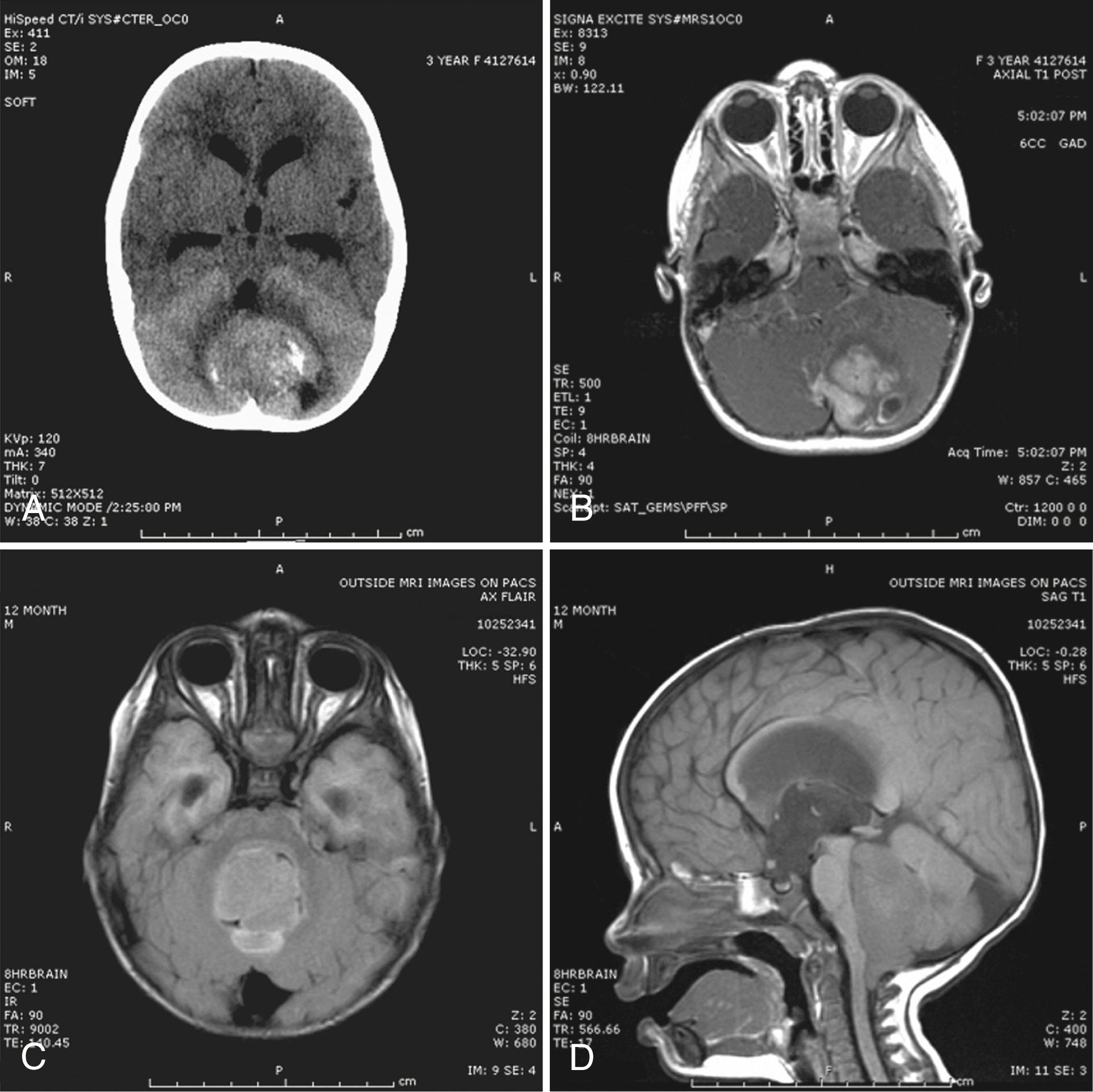
A high level of clinical suspicion is critical to make an early diagnosis. Neuroimaging is usually the first step, with computed tomography (CT) scan of the brain frequently obtained in the acute setting. Contrast-enhanced cranial MRI provides definitive imaging of the tumor. Certain MRI features may help distinguish the various types of posterior fossa tumors (medulloblastoma, ependymoma, and PA) of childhood. Although no single radiological feature is pathognomonic of a medulloblastoma, certain common characteristics exist. On CT, a medulloblastoma is generally hyperdense and homogeneously enhancing, filling the fourth ventricle ( Fig. 75.1 , A ). On contrast-enhanced cranial MRI, medulloblastomas are often isointense or hypointense to surrounding normal brain on T1-weighted images, with diffusion restriction observed in almost all tumors as a result of uniform hypercellularity (see Fig. 75.1 , B ). On T2-weighted images, medulloblastoma can appear to be hyperintense or more frequently can display mixed signal characteristics indicative of small intratumoral cysts, calcification, or small areas of hemorrhage (see Fig. 75.1 , C ). Because medulloblastoma typically arises in the roof of the fourth ventricle, a cleft of cerebrospinal fluid (CSF) beneath the tumor in the fourth ventricular canal helps distinguish this tumor from an ependymoma, which typically arises from the floor of the fourth ventricle. Ependymomas can fill the fourth ventricle and calcify more frequently than medulloblastomas. In addition, ependymomas often contain cysts, making their overall image appearance more heterogeneous. Because these tumors typically arise near the obex, ependymomas frequently extend out from the foramen of Magendie over the dorsal surface of the cervical spinal cord or through the foramen of Luschka. PAs typically arise in the cerebellar hemispheres and have the appearance of a cystic mass with an enhancing mural nodule. On T2-weighted MRI, these tumors often appear as areas of homogenous high signal intensity, with the fluid collections defining the less intense tissue components of the tumor (see Fig. 75.1 , D ). The four principal medulloblastoma subgroups have distinct imaging features, where SHH are almost always in the cerebellum, and Group 3 and 4 tumors occupy the fourth ventricle. Additionally, Group 4 tumors frequently do not enhance upon gadolinium administration, including non-enhancing metastasis. WNT tumors invade the lateral recess in 40%–50% of cases. Group 3 tumors avidly enhance upon gadolinium administration, and metastatic Group 3 tumors frequently have very small primaries. Thick bulky diffuse leptomeningeal metastasis is most commonly observed in Group 3 tumors ( ).
The first step in management after stabilization of the patient is surgery, which serves to decompress the posterior fossa and provide tissue for diagnostic purposes. In children in whom the diagnosis of medulloblastoma is suspected, a contrast-enhanced spinal MRI also should be obtained prior to surgery to assist in neurosurgical planning and staging. After imaging diagnosis, corticosteroids are frequently used to control increased ICP. If the child has unstable mental status or vital signs, emergency external ventricular drainage may be required before surgery. The goals of surgery are to control ICP, achieve a maximal safe surgical resection, establish a molecular diagnosis, and bank frozen tumor for molecular analysis prior to protocol therapy. Placement of a ventriculoperitoneal (VP) shunt before surgery is no longer commonly practiced but may be necessary after surgery. A lumbar puncture for CSF cytological evaluation should be performed 14–21 days after surgical resection to avoid false positivity. Potential complications of posterior fossa surgery include cerebellar mutism and aseptic meningitis. The posterior fossa syndrome (PFS), or cerebellar mutism, may occur in as many as 40% of children undergoing posterior fossa surgery ( ). The characteristics include reduced speech output or mutism, personality changes, hypotonia, ataxia, and reduced oral intake. Symptoms typically appear 1–2 days after surgery and may last for a few months, with varying degrees of recovery ( ).
Risk stratification is currently based on clinical staging and certain neuropathological features, although molecular observations are being incorporated into the next generation of clinical trials. Clinical staging follows the completion of perioperative brain and spine MRI and lumbar CSF cytological analysis. The M (metastasis) staging criteria include: M0, no metastases; M1, positive CSF cytology alone; M2, intracranial metastases; M3, spinal metastases; and M4, systemic metastases. The major determinants of clinical risk categorization are age at diagnosis, metastasis (M stage), primary tumor site, and volume of residual postoperative disease.
Patients are currently stratified into either standard-risk or high-risk prognostic groups. Standard-risk patients are those with medulloblastoma who are older than age 3–5 years at diagnosis, have residual tumor volume of less than 1.5 cm 2 , have no evidence of metastasis (M0), and do not have anaplastic medulloblastoma. Children younger than age 3–5 are always at higher risk because they are frequently treated with radiation-sparing approaches, where the goal of therapy is delay and/or reduction of radiotherapy. In addition, patients with residual tumor volume greater than 1.5 cm 2 , any metastatic disease, or large-cell/anaplastic medulloblastoma are at higher risk for recurrence. More recently, a molecular risk stratification is emerging which is helping to guide therapy, specifically, the division of patients into low, standard risk, high risk and very high risk. WNT patients under age 16 comprise low-risk patients. Metastatic and/or MYC amplified Group 3 and TP53 mutant SHH-activated medulloblastoma comprise very-high risk patients, with survivals under 40% ( ).
Treatment of medulloblastoma is dependent on age, where infants are treated with radiation-sparing approaches, frequently at the expense of survival, due to the devastating side effects of craniospinal irradiation to the very young brain. The definition of “infant” is variable and depends on the cooperative group; historically, infants were defined as under 3 years old in North America, under 4 years old in International Society of Paediatric Oncology (SIOP) trials, and under 5 years old in France. Treatment of non-infants usually consists of surgery, radiation therapy, and chemotherapy. Maximal safe surgical resection is recommended for all patients, particularly those with non-metastatic disease, with the residual tumor being less than 1.5 cm 2 . The current recommended therapy for standard-risk patients includes craniospinal irradiation (23.4 Gy) with a boost to the tumor bed to 55.8 Gy. Vincristine is commonly administered weekly with radiation therapy. Following radiation therapy, 4–8 cycles of cisplatin-based chemotherapy are administered, with either cisplatin, lomustine, and vincristine; or cisplatin, cyclophosphamide, and vincristine—both with similar survival. Those with metastatic dissemination or residual disease over 1.5 cm 2 are treated with 36–39 Gy of craniospinal irradiation with a boost to the tumor bed to 55.8 Gy, followed by 4–8 cycles of cisplatin, cyclophosphamide, and vincristine-based chemotherapy. In some cooperative groups, those with anaplastic and/or large-cell histology are treated on high-risk protocols; however, it is unclear if there is any benefit to this, particularly in WNT and Group 4 tumors. WNT patients are the subject of reductions in therapy, with the Children’s Oncology Group (ACNS1422) and the European Society of Pediatric Oncology (PNET5) evaluating reductions to 18 Gy of craniospinal irradiation and the St. Jude group (SJMB12) evaluating reductions to 15 Gy for standard-risk patients. In Europe, the PNET5 trial allows WNT patients with metastatic disease or residual tumor to be treated with 23.4 Gy of craniospinal irradiation.
In addition to developing effective chemotherapy regimens with less toxicity, several groups are trying to decrease the toxicity associated with radiation therapy. The use of proton-beam radiation therapy as an alternative to high-energy x-rays (photons) has been studied and found to have the potential to limit late effects of radiation therapy by reducing the exposure of normal tissue to radiation ( ). Proton radiation can spare adjacent critical structures such as the optic apparatus, cochlea, and hypothalamus as well as limit exposure to the trunk when they are not adjacent to tumor volume, potentially resulting in fewer long-term sequelae ( ).
Infants are treated with radiation-sparing approaches post-surgery, where the treatment is highly dependent on both molecular subgroup and/or histology. In Europe the approach is to administer intraventricular methotrexate with induction chemotherapy, and in North America infants are treated with induction chemotherapy followed by 1–3 cycles of myeloablative chemotherapy with autologous stem cell transplant ( ; ; ). Using this approach, patients with SHH medulloblastoma (or desmoplastic medulloblastoma) have excellent radiation-free survival of nearly 90%. Efforts to reduce therapy through omission of myeloablative chemotherapy or intraventricular methotrexate have resulted in dismal results for SHH medulloblastoma ( ). Group 3 infants have a poor prognosis without radiation, particularly those with metastatic disease and likely warrant new approaches. The role of focal radiation is not clear, and is likely of little to no benefit in Group 3 or 4 infants considering the metastatic pattern of relapse.
Standard-risk medulloblastoma patients have a 5-year survival of approximately 80%; 5-year survival in high-risk medulloblastoma patients is approximately 50%–60% ( ; ; ; ; ). Infants with SHH/desmoplastic histology can have radiation-free survival of close to 90% with intensive therapy, whereas Group 3 and 4 infants have dismal radiation-free survivals of less than 40% for non-metastatic disease, and less than 10% for metastatic disease ( ; ; ). The presence of CNS dissemination is the single most important factor that correlates with outcome, independent of subgroup ( ; ). Relapsed medulloblastoma in previously irradiated patients is associated with dismal survival rates of less than 10%, and although some approaches can provide extension of survival with good quality of life, these are essentially palliative ( ; ). Lifelong serial surveillance imaging is recommended in anticipation of radiation-induced secondary malignancies such as meningioma or high-grade glioma ( ). Radiation therapy, particularly in young children, can also cause significant adverse late effects in cognitive development, growth, and endocrine function ( ; ).
Embryonal CNS tumors are the most common group of malignant brain tumors in children and include medulloblastomas, CNS embryonal tumors, embryonal tumor with multilayered rosettes (ETMR), and atypical teratoid/rhabdoid tumors (ATRT). There have been several changes to the categorization of embryonal tumors in the 2016 revised WHO classification of CNS tumors ( ). A significant change from the 2007 WHO classification is the removal of the diagnosis ‘CNS primitive neuroectodermal tumor (CNS-PNET)’ and the inclusion of ETMR. CNS embryonal tumors are a diagnosis of exclusion, and morphologically are frequently mistaken for other supratentorial tumors, particularly high-grade gliomas. ATRT, ETMR, ependymoma, CNS sarcoma, and choroid plexus carcinoma must also be excluded. The remaining tumors formerly included in the diagnosis of CNS-PNET now comprise CNS neuroblastoma, CNS ganglioneuroblastoma, medulloepithelioma and CNS embryonal tumor not otherwise specified (NOS). Applying DNA methylation classification and unsupervised clustering, the majority of entities previously labeled CNS-PNET are reclassified as other entities. However, within the proportion of CNS embryonal tumors that do not reclassify, recurrent fusions and duplications of FOXR2 , BCOR , MN1 , and CIC1 have been identified representing new brain tumor entities ( ; ). ETMR are divided into tumors harboring an amplicon at a microRNA (miRNA) cluster on chromosome 19, or with the morphological diagnosis without the amplicon. Pineoblastomas are embryonal tumors arising from the pineal gland, and frequently harbor recurrent homozygous deletion of DROSHA, the core nuclease that initiates miRNA processing in the nucleus (Snuderl et al., Nat Commun. 2018).
There is limited understanding of the etiology of CNS embryonal tumors, which have emerged as a highly heterogeneous group. A unifying molecular signature, including amplification of the C19MC oncogenic miRNA cluster and high LIN28 expression, has been found that encompasses several CNS embryonal tumor histological classes, including ETMR, medulloepithelioma, and CNS embryonal tumor NOS ( ; ; ). These tumors have a very poor prognosis and tend to occur in children younger than 4 years old. Other markers for CNS embryonal tumors have not yet been defined, making further histopathological classification difficult. A major confounding issue to understanding the incidence and presentation of CNS embryonal tumors is that a significant proportion of these tumors are glioblastomas, resulting in difficulties in interpreting previous studies ( ).
Trilateral retinoblastoma is a well-recognized syndrome characterized by bilateral retinoblastomas occurring concurrently with a pineoblastoma with retinoblastic features. Although approximately half of the cases of trilateral retinoblastoma are associated with the familial form of retinoblastoma, one analysis indicates that most children with trilateral retinoblastoma have ordinary hereditary retinoblastoma that is complicated by trilateral disease by chance, thus dispelling the notion that trilateral retinoblastoma is caused by a different allele than that which causes ordinary retinoblastoma ( ).
Although earlier reports of supratentorial PNET have occurred in patients with the LFS (mutations in the TP53 gene on chromosome 17), it is likely that these tumors represent misdiagnosed high-grade gliomas or glioblastomas, and molecularly defined cohorts are required to help elucidate this. Tumors previously described as PNET that are not reclassified as another entity after extensive molecular work-up, fall into one of four entities: CNS neuroblastoma with FOXR2 activation; CNS Ewing sarcoma family tumor with Capiciua transcriptional repressor (CIC) alteration; CNS high-grade neuroepithelial tumor with MN1 alteration; and CNS high-grade neuroepithelial tumor with Bcl6 co-repressor (BCOR) alteration. These entities require either DNA methylation analysis and/or RNA sequencing for diagnosis, and are the subject of ongoing studies ( ; ). The clinical implications and precise diagnosis of these groups is still emerging, and rendered challenging due to their rarity.
Similar to medulloblastoma, the presenting features of all CNS embryonal tumors are highly dependent on their location, including progressive headache, nausea, vomiting, seizures, and lethargy secondary to increased ICP. Children with pineoblastomas often present with dorsal midbrain compression (Parinaud syndrome) and obstructive hydrocephalus secondary to aqueductal occlusion.
CNS embryonal tumors, ETMR, and pineoblastomas have historically been stages and treated according to medulloblastoma protocols. Prognosis for tumors previously classified as supratentorial PNETs has been highly variable. ETMR usually arise in young infants, and carry a very poor prognosis, with survival less than 20%, despite aggressive therapies with upfront radiotherapy and high-dose chemotherapy with autologous stem cell transplant. The prognosis of CNS embryonal tumors and pineoblastoma are variable across studies. However, those with metastatic disease have much inferior survival compared with those with non-metastatic disease, as do infants treated with radiation- sparing approaches. Future molecularly informed clinical trials are required to adequately determine optimal therapies for this heterogeneous group of patients.
ATRT is a highly malignant tumor that was first recognized in the 1980s as a distinct entity ( ; ). Rhabdoid tumors may arise anywhere in the body, but are most common in the kidney where they are referred to as malignant rhabdoid tumors and in the CNS where they are classified as ATRT. ATRTs can occur anywhere in the nervous system, and occur primarily supratentorially or in the posterior fossa, either in isolation or in association with germline predisposition, in other parts of the body such as the kidneys, or even with metachronous primary tumors. ATRT are defined by the loss of INI-1/BAF47, the protein encoded by the SMARCB1 gene located on chromosome 22q, and is a germline event as part of the rhabdoid predisposition syndrome in 25%–35% of all cases.
Integrated genomic studies have revealed significant heterogeneity across ATRT, with at least three epigenetically defined subgroups. These groups—termed ATRT-SHH, ATRT-MYC, and ATRT-TYR—have distinct gene expression and DNA methylation patterns, distinct demographics, and genetics. The ATRT-SHH group is predominantly infratentorial with broad SMARCB1 mutations, ATRT-TYR are composed of both infratentorial and supratentorial tumors with focal lesions in SMARCB1 , and ATRT-MYC are composed of predominantly supratentorial tumors in older children ( ; ). The prognostic and therapeutic implications of these groups are currently unclear.
ATRTs are seen primarily in infants and young children, with a peak incidence between birth and age 3. ATRTs account for approximately 1%–2% of all childhood brain tumors, but these neoplasms represent nearly 10% of CNS tumors in infants ( ). Children with ATRT often present with signs and symptoms consistent with the location of the primary tumor, similar to those with medulloblastoma or CNS embryonal tumor, including vomiting, loss of milestones, irritability, and increasing head circumference.
Owing to similar morphology, these tumors may be confused with medulloblastomas, CNS embryonal tumors, and choroid plexus carcinomas, and as such need to be considered in any young child presenting with a small-blue-cell tumor. The definitive diagnosis of ATRT is based on loss of immunoreactivity to INI1 and/or identification of a genetic lesion in the SMARCB1 gene, which is present in almost all cases. There is a small, relatively poorly defined subset of molecularly defined ATRT lacking lesions in SMARCB1 , but rather having inherited mutations in SMARCA4 , with a poor prognosis ( ). All patients diagnosed with ATRT should be referred to a geneticist for germline screening and counseling, and a surveillance protocol should be considered after completion of therapy ( ).
Historically, ATRT have been treated as medulloblastoma with very poor survival, with the POG-9923/4 and CCG-9921 studies of conventional chemotherapy resulting in less than 10% survival. More recently, rhabdoid-specific multimodal therapy has been applied, with more favorable results, and the emergence of long-term survivors in upwards of 50% of patients. These treatments have included various combinations of aggressive surgery with complete resections and intensive chemotherapy, with and without irradiation, resulting in survivals of between 40% and 50% overall ( ; ; ; ). The Children’s Oncology Group has recently completed a trial using multidrug chemotherapy with high-dose methotrexate, high-dose chemotherapy with autologous stem cell rescue, and radiation therapy, with promising results ( ). Germline predisposition is felt to have a worse survival; however, this is also unclear at the present time.
The spectrum of astrocytic tumors is broad and includes a wide range of glial neoplasms that differ in anatomical location, morphological features, degree of invasiveness, and clinical course. Grading of astrocytomas by the WHO is predictive of patient survival ( ) ( Box 75.1 ). Astrocytomas can be classified as low grade (WHO grade I and II) or high grade (WHO grade III and IV). Analogous to adult gliomas, the advent of molecular diagnostics has brought into question of the utility of WHO grading in isolation. However, currently, treatment protocols and clinical trials still rely on the distinction between low-grade and high-grade glioma. A crucial distinction between adult and pediatric low-grade gliomas are that pediatric low-grade gliomas rarely transform to higher-grade tumors, and in many instances eventually senesce, with the exception of a subset of BRAF mutant tumors harboring CDKN2A loss, and as such the approach and treatment should be commensurate with its natural history ( ; ). The most common pediatric subtypes recognized by the current WHO classification will be discussed.
| Astrocytic Tumors | Oligodendroglial and Oligoastrocytic Tumors | Neuronal and Mixed Neuronal-Glial Tumors |
|---|---|---|
| Pilocytic astrocytoma (I) | Oligodendroglioma (II) | Gangliocytoma (I) |
| Subependymal giant cell astrocytoma (II) | Anaplastic oligodendroglioma (III) | Ganglioglioma (I) Anaplastic ganglioglioma (III) Desmoplastic infantile astrocytoma and ganglioglioma (I) Dysembryoplastic neuroepithelial tumor (I) Central neurocytoma (II) |
| Pilomyxoid astrocytoma (II) | ||
| Diffuse astrocytoma (II) Pleomorphic xanthoastrocytoma (II) |
||
| Anaplastic astrocytoma (III) Glioblastoma (IV) |
PAs are well-circumscribed, slow-growing tumors classified as WHO grade I ( ). These tumors are the most common gliomas found in children and represent approximately 20% of all childhood brain tumors. PAs are typically diagnosed in the first two decades, with no clear gender predilection. Neurofibromatosis type 1 (NF1) is associated with an increased risk of PA ( ). No other definite predisposing factors are known. Histologically, PAs consist of bipolar cells with long “fiber-like” processes: hence the name pilocytic. Other distinctive histological features of PAs include Rosenthal fibers, eosinophilic granular bodies, and microcysts. Constitutive activation of the mitogen-activated protein kinase (MAPK) signaling pathway through specific, recurrent gene fusions of BRAF and less commonly activating mutations (V600E) are by far the most common somatic events identified in PAs, as well as other pediatric low-grade astrocytomas (LGAs) ( ; ; ; ). This provides an opportunity for the development of molecular targeted therapies.
PAs can arise anywhere in the CNS, but most commonly occur in the cerebellum, optic pathways, hypothalamus, cerebral hemispheres, midbrain, and medulla. PAs of the spinal cord are less common. The spectrum of clinical manifestations depends on the structures involved and may include visual deficits, obstructive hydrocephalus, macrocephaly in younger patients, ataxia, endocrine dysfunction, focal neurological deficits, long-tract signs, cranial nerve dysfunction, and seizures if the tumor involves cortical structures. Cerebellar PAs usually present with symptoms indicative of increased ICP, such as headache, nausea, and vomiting. Brainstem PAs are usually dorsal and exophytic with obstructive hydrocephalus often the presenting feature. The diencephalic syndrome is unique to low-grade gliomas, usually juvenile PAs arising in infants in the hypothalamus or optic pathways, and consists of emaciation with normal linear growth, frequently accompanied by hyperemesis, hyperkinesis, and nystagmus ( ; ; ). Indeed, a hypothalamic glioma should be considered in young children presenting with failure to thrive without another apparent etiology.
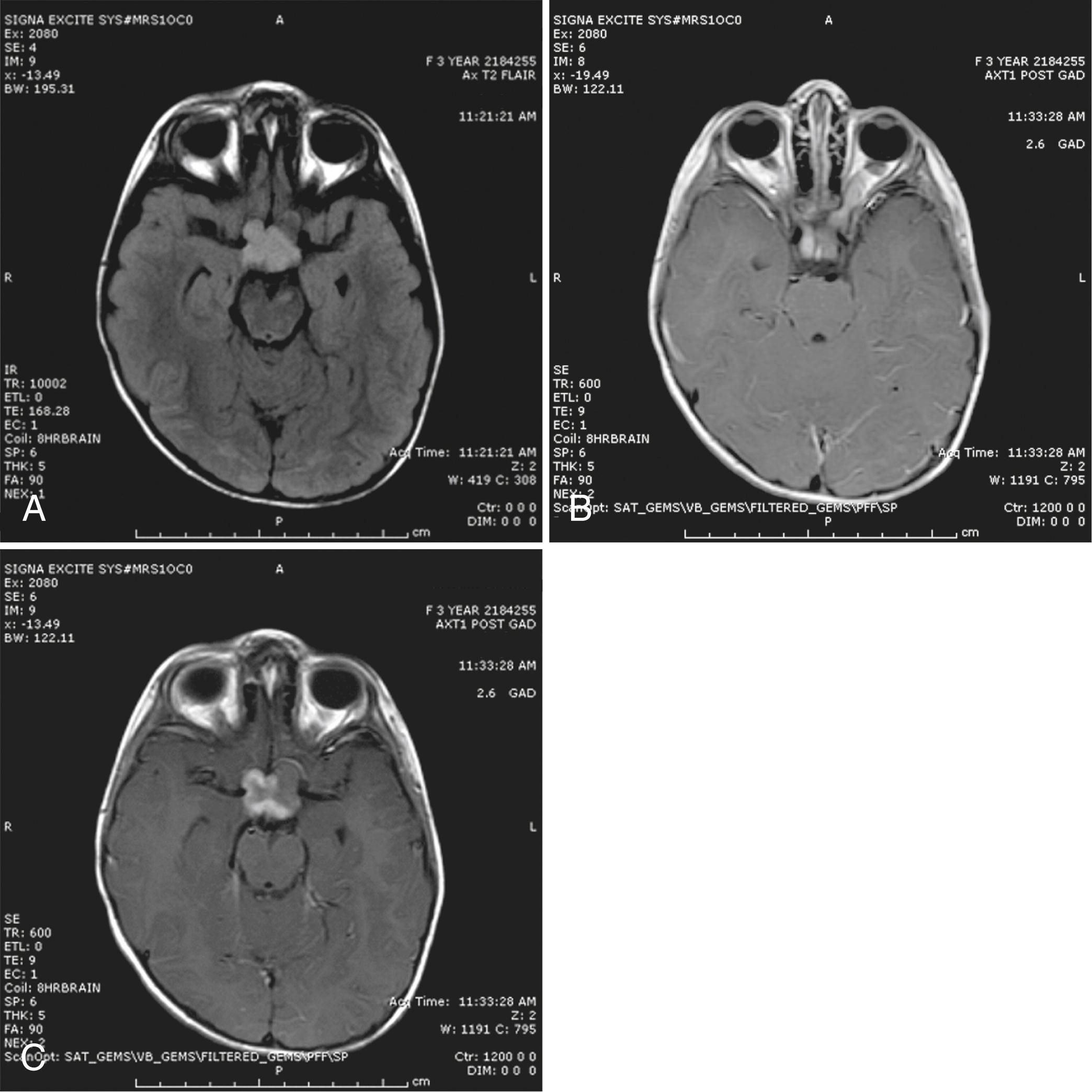
A tissue diagnosis should be attempted in all children presenting with a suspected low-grade glioma and no clinical signs of neurofibromatosis type 1. The emergence of molecular diagnostics is significantly changing the diagnosis of low-grade gliomas, specifically the PA. Treatment and risk stratification now require the identification of specific alterations in BRAF, either tandem duplications with a fusion to KIAA1549, or, less frequently, point mutations at the V600E position. The history of illness is usually long; other signs of chronicity—such as bone remodeling, scoliosis, or hemihypotrophy—may be present, depending on the primary tumor location. The typical MRI appearance is a homogeneously enhancing mass with only minimal associated edema. Intratumoral cysts are common, depending on location—particularly in the cerebellum, where the typical appearance is one of a large cyst with mural nodule ( Fig. 75.2 ). In approximately 5% of patients, PAs present with diffuse leptomeningeal dissemination, especially in infants and as such a baseline spinal MRI should be performed prior to initiation of therapy or surveillance ( ).

The mainstay of therapy for PAs is surgery. If feasible, gross total resection is “curative” even though residual microscopic disease always remains, and radiation or chemotherapy are typically not required. In situations where resection is not possible, tissue biopsy should be attempted to allow for an accurate molecular and histopathological diagnosis prior to initiation of therapy. Partial resections have little role in the treatment of PAs, with the exception of a symptomatic patient. Progressive or unresectable PAs, or those arising in infants or young children causing visual symptoms, may require adjuvant treatment.
Chemotherapy has an important role in the management of all progressive low-grade gliomas. The three most commonly used regimens are carboplatin/vincristine, TPCV (thioguanine, procarbazine, lomustine, and vincristine), and single-agent vinblastine monotherapy ( ; ). Carboplatin/vincristine and TPCV regimens were compared in a randomized phase III trial by the Children’s Oncology Group, and although TPCV was found to be moderately superior in regard to event-free survival, carboplatin/vincristine or vinblastine is considered the primary first-line therapy due to the poor safety profile of TPCV and increased risk of secondary malignancy ( ). Historically, a substantial proportion of patients require multiple courses of chemotherapy, but eventually most low-grade gliomas stop progressing. The emergence of targeted agents in the form of MEK and/or BRAF inhibitors have emerged as powerful second-line options: specifically, BRAF/MEK inhibitors for BRAF V600E mutant tumors and MEK inhibition for BRAF fused tumors ( ; ). These agents have shown very impressive responses in early-phase clinical trials and randomized studies versus chemotherapy are currently ongoing through the Children’s Oncology Group and the European Society of Pediatric Oncology. Because of concern for adverse effects, including neurocognitive and endocrine effects as well as secondary malignancies, early stroke, and the moyamoya syndrome, radiation therapy is usually deferred or omitted in children with low-grade gliomas, including those with multiple relapses ( ; ; ). Radiation is a relative contraindication in children with NF-1 due to the very high risk of secondary high-grade gliomas and vasculopathies.
The prognosis for resectable tumors is excellent, with 5-year recurrence-free survival of greater than 90% after gross total resection ( ). The most critical variable in the treatment of PAs is the anatomical location of the tumor. Complete resections are most difficult for tumors located in the brainstem, spinal cord, and hypothalamus. As such, the progression-free survival of children with centrally located tumors (e.g., optic chiasm, thalamus, hypothalamus) is reduced. The use of chemotherapy as initial treatment in patients with centrally located or unresectable tumors allows for the sparing or delay of radiation therapy until the child is less likely to suffer major developmental and neuropsychological sequelae. Ultimately, the quality of survival depends on multiple factors including tumor location, extent of tumor resection, timing of any radiation therapy, and side effects of surgery, chemotherapy, and radiation. Malignant transformation of PA and other LGAs in children is rare ( ). Targeted inhibitors v-Raf murine sarcoma viral oncogene homolog B (BRAF) and Mitogen-activated protein kinase kinase (MEK) now provide an option with a significant likelihood of tumor size reduction; however, the impact of these agents on long-term outcome and functional status is unknown.
Optic pathway gliomas (OPGs) may be considered a subset of PAs, but their unique features and management requirements warrant a separate discussion. OPGs represent approximately 4%–6% of all primary pediatric brain tumors. These tumors may involve various parts of the optic pathway, such as the optic nerves, optic chiasm, optic tract, and optic radiations. The tumor may also infiltrate the adjacent hypothalamus and temporal lobes. Optic nerve gliomas are strongly associated with NF1, and NF1 patients represent about 50% of patients treated for OPG. Although approximately 20% of NF1 children scanned prospectively from birth will acquire MRI abnormalities suggestive of an anterior or posterior OPG, less than half of those will develop progressive neurological and radiological disease, and the occasional tumor may undergo spontaneous regression ( ). OPGs in NF1 patients have been suggested to have a more indolent course than those arising in patients without NF1 with improved progression-free survival compared with non-NF1 patients ( ). Non-NF1 OPGs frequently harbor either BRAF fusions or BRAF mutations, similar to other low-grade gliomas of childhood ( ).
Most OPGs are LGAs, primarily PAs (WHO grade I) ( ). Although most OPGs are of lower histological grade, the clinical course of these tumors may be aggressive when the optic pathways and hypothalamus are invaded. Age is an important prognostic factor: children younger than 5 years of age experience a more aggressive course. Unilateral optic nerve gliomas present with the classic triad of vision loss, proptosis, and optic atrophy. Chiasmatic involvement may lead to unilateral or bilateral vision loss, optic tract involvement may lead to a visual-field deficit, and large dorsally exophytic or hypothalamic components of the tumor may lead to obstructive hydrocephalus. Further invasion into brain parenchyma may result in visual-field defects and hemiparesis. The diencephalic syndrome is unique to infant presentations of OPG and hypothalamic PA and presents with irritability, failure to thrive, nystagmus, visual loss, and hydrocephalus in the first or second year of life ( ).
The clinical diagnosis of an OPG should be suspected when a child presents with visual impairment associated with nystagmus and optic atrophy. It is very difficult to ascertain visual loss in younger children, but close behavioral observation during play may raise suspicion. Contrast-enhanced cranial or orbital MRI typically shows a solid, cystic, or solid and cystic tumor with enhancement ( Fig. 75.3 ). MRI studies and clinical presentation may distinguish an OPG from other childhood tumors that arise in the suprasellar location, such as a germ cell tumor or craniopharyngioma. The unpredictable clinical course of patients with OPGs has led to controversy regarding the optimal management of these tumors. The clinical course, age of onset, severity of symptoms, size and extent of the tumor, and the presence of NF1 may all impact management decisions. Preservation of vision is paramount and the major indication for treatment, and although chemotherapy may cause stabilization or regression of the tumor on imaging studies the correlation with visual outcome is poor ( ; ). The emergence of targeted agents, specifically MEK and BRAF inhibitors, has the potential to significantly improve visual outcomes even in young children; however, the timing of their use is still not clear ( ; ). The chemotherapy regiments used for PA are also used for the treatment of OPG, most commonly carboplatin/vincristine and vinblastine monotherapy. Bevacizumab has shown the potential to significantly improve vision and can be considered in patients with progressive visual loss ( ).
Although OPGs are histologically low-grade tumors, the location of these neoplasms often results in serious morbidity. The growth rate of OPGs often slows in older children and young adults. The most robust adverse prognostic factor across multiple studies has been age younger than 1 year at diagnosis, although some suggest that children with NF1 may have a longer progression-free survival ( ). Patients with OPGs associated with NF1 may remain stable for several years, and the indication for treatment is visual loss. Close observation and symptomatic management are appropriate for this subpopulation.
Subependymal giant cell astrocytomas (SEGAs) usually originate in the ependymal lining of the lateral ventricles and are associated almost exclusively with tuberous sclerosis (TS). Sporadic SEGAs are rare. TS is an autosomal dominant genetic syndrome caused by mutations in either TSC1 (hamartin) or TSC2 (tuberin), which are regulators of key cellular signaling pathways including the mammalian target of rapamycin (mTOR) pathway ( ).
Subependymal giant cell astrocytoma is sometimes the presenting feature of TS in patients without the typical physical stigmata of the syndrome. Although patients with TS typically have multiple periventricular SEGAs, the tumors that produce symptoms of hydrocephalus arise in close proximity to the foramina of Munro. Most patients with known TS have been followed with serial MRI scans, and newly identified SEGAs are typically removed in anticipation of more serious neurological syndromes such as headaches, altered sensorium, or weakness. These children may have other neurological symptoms such as seizures related to cortical tubers and cognitive deficiency.
Contrast-enhanced cranial CT and MRI are essential for early and accurate diagnosis. Whereas the former is better for detecting small calcified lesions, MRI is superior to CT in identifying areas of gliosis, heterotopia, and SEGA, which gives the typical imaging appearance of candle dripping ( ). SEGAs typically demonstrate diffuse contrast enhancement on both CT and MRI studies. Pharmacological inhibition of the mTOR signaling pathway with everolimus has been approved by the US Food and Drug Administration (FDA) and the European Medicine Agency (EMA) for the treatment of SEGA associated with TS ( ; ). SEGA may respond dramatically to mTOR inhibitors, but the tumors will recur once mTOR inhibition is terminated. Everolimus also improves seizure control in TS patients ( ; ; ). The dramatic and sustained responses to mTOR inhibitors, along with the improvements in seizures, autism, and angiomyolipoma, has largely resulted in surgical intervention being displaced as a first-line approach, with surgery being reserved for those cases refractory to medical therapy.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here