Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Fetal genitourinary system abnormalities encompass a wide spectrum of disorders varying in degrees of severity and include developmental anomalies, obstructive lesions in the urinary tract, and renal parenchymal diseases. The prenatal evaluation of the genitourinary system includes assessment of the amniotic fluid, the kidneys, the bladder, and associated anomalies. Amniotic fluid is important for normal fetal development, particularly the fetal lungs. In the first trimester, amniotic fluid forms as a dialysate of maternal serum. Fetal urine production begins by 12 weeks of gestation and becomes the major source of amniotic fluid by 16 weeks. Fetal urine production is typically 120 mL/day at 20 weeks and increases gradually to 1200 mL/day by term. The fetus voids every 30 to 60 minutes. The bladder should be visualized at least once during a prenatal imaging examination.
Identification of the fetal urinary bladder is attempted in the first trimester ultrasound, and more detailed evaluation of the kidneys and bladder is a fundamental part of the second trimester fetal anatomic assessment. Complex cases, such as bladder exstrophy, confusing duplex collecting systems, and obstructive masses, may be further evaluated by fetal magnetic resonance imaging (MRI). Sonographic fetal anatomic assessment may be limited in the setting of oligohydramnios, and MRI may be particularly useful. Prenatal findings may influence the further pursuit of genetic and laboratory testing or surgical intervention and may guide the delivery plan.
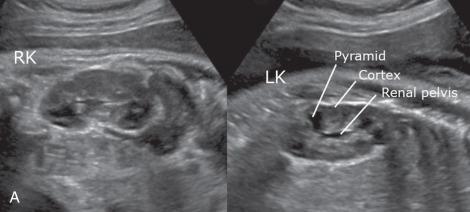
Fetal kidneys can be identified at 13 weeks of gestation. Normal renal sizes through gestation (mean kidney length in millimeters is slightly longer than weeks of gestation) are shown in Table 112.1 . Corticomedullary differentiation is apparent by 20 weeks of gestation ( Fig. 112.1 ). Renal calyces and ureters typically are not seen on ultrasound unless they are pathologically dilated, and the renal pelvis is only readily visualized once the anterior-posterior diameter exceeds 2 mm. The fetal bladder can be visualized at 10 weeks of gestation. The bladder wall should not measure more than 3 mm. Bladder wall thickening may be a sign of outlet obstruction.
| Gestational Age (wk) | Mean Kidney Length (cm) | 95% Confidence Interval (cm) |
|---|---|---|
| 18 | 2.2 | 1.6-2.8 |
| 19 | 2.3 | 1.5-3.1 |
| 20 | 2.6 | 1.8-3.4 |
| 21 | 2.7 | 2.1-3.2 |
| 22 | 2.7 | 2-3.4 |
| 23 | 3 | 2.2-3.7 |
| 24 | 3.1 | 1.9-4.4 |
| 25 | 3.3 | 2.5-4.2 |
| 26 | 3.4 | 2.4-4.4 |
| 27 | 3.5 | 2.7-4.4 |
| 28 | 3.4 | 2.6-4.2 |
| 29 | 3.6 | 2.3-4.8 |
| 30 | 3.8 | 3.9-4.6 |
| 31 | 3.7 | 2.8-4.6 |
| 32 | 4.1 | 3.1-5.1 |
| 33 | 4 | 3.3-4.7 |
| 34 | 4.2 | 3.3-5 |
| 35 | 4.2 | 3.2-5.2 |
| 36 | 4.2 | 3.3-5 |
| 37 | 4.2 | 3.3-5.1 |
| 38 | 4.4 | 3.2-5.6 |
| 39 | 4.2 | 3.5-4.8 |
| 40 | 4.3 | 3.2-5.3 |
| 41 | 4.5 | 3.9-5.1 |
Amniotic fluid volume can be a reflection of renal health. Oligohydramnios (defined by an amniotic fluid index less than 8 cm) may be seen in the setting of placental insufficiency, intrauterine growth retardation, chromosomal abnormality, premature rupture of membranes, post-dates gestation, or urologic pathology ( Box 112.1 ).
Bilateral renal agenesis
Bilateral multicystic dysplastic kidney
Bilateral severe ureteropelvic junction obstruction
Bilateral renal disease with one kidney each involved with items 1, 2, or 3 above
Severe prune-belly syndrome
Severe autosomal recessive polycystic kidney disease
Severe renal dysplasia as a result of posterior urethral valves or urethral atresia
Fetal renal echogenicity may be abnormally increased as a normal variant but more often reflects an underlying abnormality. The fetal kidney is considered echogenic if it is brighter than the fetal liver. Echogenic kidneys are observed in approximately 1 to 2 per 1000 fetal ultrasounds, and approximately 10% of cases of renal malformations include echogenic kidneys. Etiologic considerations for the echogenic kidney are summarized in Box 112.2 . If echogenic kidneys are identified and the amniotic fluid volume is normal, the findings suggest nonlethal renal disease. Echogenic kidneys with oligohydramnios are highly concerning for a poor outcome.
Idiopathic
Cystic renal disease
Infection
Chromosomal abnormalities
Toxic and ischemic insults
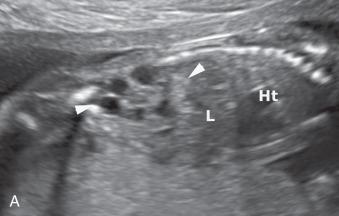
Congenital cystic renal diseases occur in about 2 to 4 in 1000 live births and include autosomal dominant and autosomal recessive polycystic kidney disease ( Fig. 112.2 and ), multicystic dysplastic kidney ( Fig. 112.3 ), cystic glomerulopathies, and other cystic renal dysplasias. The complex pathogenesis of these disorders involves an abnormal orchestration of transcription and growth factor expression ( Table 112.2 ), as well as ciliopathies affecting the renal tubule primary cilium ( Table 112.3 ). Structural and functional abnormalities in primary cilia contribute to various cystic phenotypes that involve the kidney and liver.

| Renal Abnormality | PAX2 (paired box 2 gene, 10q24.31) | HNF1B (HNF1B Homeobox B, 17q12) | EYA1 (EYA transcriptional coactivator and phosphatase 1 gene, 8q13.3) | SIX1 (SIX Homeobox 1, 14q23.1) | SALL1 (Spalt like transcription factor 1, 16q12.1) | GATA3 (GATA binding protein 3 gene, 10p14) |
|---|---|---|---|---|---|---|
| Dysplasia | √ | √ | √ | √ | √ | √ |
| Renal agenesis | √ | √ | √ | |||
| Renal hypoplasia | √ | √ | √ | |||
| Ureteropelvic junction obstruction | √ | √ | √ | |||
| Vesicoureteral reflux | √ | √ | ||||
| Glomerulocystic kidney disease | √ | |||||
| Syndrome | Renal-coloboma | MODY5 | BOR | BOR | Townes-Brock | HDR |
| Ciliopathy | Protein | Inheritance | Lesions |
|---|---|---|---|
| Autosomal dominant PKD | Polycystin 1, Polycystin 2 | AD | Cysts within the entire nephron |
| Autosomal recessive PKD | Fibrocystin | AR | Collecting duct cysts |
| Meckel-Gruber syndrome | MKS proteins 1, 3 | AR | Cystic dysplasia |
| Oral-facial-digital syndrome | OFD protein | X-linked | Glomerular kidney disease |
| Bardet-Beidl syndrome | BBS proteins 1-8 | Digenic | Tubulointerstitial nephritis |
| Von Hippel-Lindau | VHL protein | AR | Renal cysts (premalignant) and renal cell carcinoma |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here