Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The two most common surgical procedures of the biliary tract likely to be encountered in day-to-day practice are laparoscopic cholecystectomy (LC) and biliary-enteric anastomosis. Specifically, given the high prevalence of cholelithiasis or gallstones in the United States, with roughly 20 to 25 million people affected, a large number of patients undergo cholecystectomy each year (~700,000). The revolutionary development and refinement of laparoscopic techniques during the last two decades have allowed LC to largely supplant open surgery. The creation of a biliary-enteric anastomosis (most often hepaticojejunostomy), on the other hand, can be performed for any number of different indications, the most common of which include liver transplantation, resection of tumors involving the biliary tree, benign or malignant biliary obstruction, biliary stones, and bile duct injuries. , Whereas LC and hepaticojejunostomy are both relatively well-tolerated procedures with a low risk of complications, the large number of these procedures performed in the United States each year makes it critical for radiologists to recognize the different complications that may be associated with these surgical procedures and to understand the basic diagnostic and treatment algorithms for each of these complications. This chapter discusses a number of complications associated with LC and hepaticojejunostomy and illustrates their appearances by a number of different radiologic modalities. In addition, this chapter concludes with a discussion of the radiologic diagnosis of post-traumatic lesions of the biliary tree. These traumatic injuries to the bile ducts and gallbladder are relatively rare but can carry a high morbidity and mortality in cases of missed or delayed diagnosis.
In most cases, the imaging findings after LC should be relatively minimal.
A small amount of pneumoperitoneum is an expected finding. , The volume of free air after laparoscopic procedures is generally smaller and lasts for a shorter time compared with open surgery, largely as a result of the relatively small incisions in the anterior abdominal wall and the use of carbon dioxide for insufflation (which is rapidly absorbed). As with other abdominal surgeries, the presence of a large amount of pneumoperitoneum after surgery, or pneumoperitoneum that persists for a longer than expected duration (10–14 days), should raise concern for bowel injury or perforation during the procedure.
A small amount of subcutaneous emphysema at the incision site is not uncommon, usually resulting from the dissection of insufflated carbon dioxide around the trocars into the subcutaneous soft tissues. This finding is common in the first 24 to 48 hours after surgery but should not be seen in significant amounts thereafter. ,
Small densities in the subcutaneous fat surrounding the trocar insertion sites can develop over time and probably represent sites of fat necrosis or scarring related to the surgical intervention.
Small postoperative fluid collections in the gallbladder fossa are a common finding immediately after surgery and may be associated with a tiny amount of free fluid in the pelvis. These fluid collections are almost always asymptomatic and should resolve spontaneously. Nevertheless, if there are clinical signs of infection, reimaging may be helpful as these collections can rarely become superinfected and develop into abscesses.
Permanent surgical materials, such as surgical clips, are a common finding in the gallbladder fossa. Potentially confusing, however, is the presence of absorbable hemostatic sponges, occasionally used intraoperatively to control bleeding, which should gradually be absorbed over time. The most commonly used of these materials is gelatin sponge (Gelfoam; Pharmacia and Upjohn, Kalamazoo, MI, USA) or oxidized absorbable cellulose (Surgicel; Ethicon, Somerville, NJ, USA). The appearance of these absorbable agents on computed tomography (CT) is typically as a discrete mass with mixed or low attenuation and with central or peripheral gas collections. In the absence of a reliable clinical history, such an appearance can be extremely difficult to distinguish from a postoperative abscess or fluid collection, and a discussion with the surgeon may be necessary to arrive at the correct diagnosis. If not, this absorbable material should disappear in a period of weeks on serial CT examinations.
Postsurgical complications after LC are relatively rare. Overall, there is no evidence in the literature that the transition from open to laparoscopic surgical technique has resulted in any appreciable increases in morbidity or mortality. A Cochrane Database review that examined 38 different studies in the literature (with 2338 patients) found no difference in mortality between open cholecystectomy and LC, and although there was the suggestion of a lower overall complication rate with laparoscopic technique, this could not be validated in the highest-quality studies. Moreover, laparoscopic technique is clearly associated with a shorter hospital stay, better cosmetic results, less postoperative pain, and faster return to work.
Nevertheless, postsurgical complications are not infrequently encountered regardless of the surgical technique used. Complications are thought to be more likely in patients with active (or prior bouts of) cholecystitis, longer time (typically > 72 hours) between the onset of cholecystitis symptoms and surgery, male gender, prior upper abdominal surgery, significant pericholecystic fluid, high body mass index, diabetes, and advanced age, all of which are factors that may render LC more technically difficult. , Notably, these same patient factors represent the most common risk factors for conversion of LC into an open procedure, and the conversion rate is thought to be as high as 12%. , , As one would expect, patients with significant gallbladder inflammation (including gangrenous and emphysematous cholecystitis) are also at higher risk for complications and conversion to an open procedure.
Complications of LC include those associated with the laparoscopic component of the procedure as well as those related to the cholecystectomy itself. The most common complications related to laparoscopy include abdominal wall or omental bleeding, intraperitoneal or retroperitoneal vessel injury, bowel injury or perforation, and solid visceral organ injury. The most common complications related to cholecystectomy include gallbladder fossa bleeding, bile duct injury, bile leakage, gallbladder perforation (with stone spillage), retained biliary stones, and biliary strictures. Less commonly, laparoscopic cholecystectomies can be complicated by vascular injuries, with an incidence ranging between 0.05% and 0.25%. Vascular injury is the second leading cause of death in patients undergoing laparoscopic procedures (of any kind), and the hepatic artery is the most frequently injured vessel during LC. Given that the mortality rate for patients suffering vascular injuries during laparoscopy can be as high as 9%, careful evaluation of the hepatic artery along its entire course is critically important in evaluating multidetector CT (MDCT) studies in patients who have recently undergone LC. ,
Biliary tract complications are the most important complications of cholecystectomy and represent a major source of litigation. Biliary tract complications can be encountered with both open and laparoscopic cholecystectomies, and there is little evidence of any increase in biliary tract complications with laparoscopic technique. Many of these complications are often not recognized at the time of surgery and are not uncommonly diagnosed after a significant delay, resulting in considerable patient morbidity and mortality. , , , The most important biliary complications for the radiologist to recognize are bile duct injury, bile leak, retained stones, bile duct strictures, and spilled stones in the peritoneal cavity.
There are more than 2500 bile duct injuries related to LC in the United States each year, and many of these injuries are attributable to acute or chronic inflammation obscuring fat planes surrounding the gallbladder or intraoperative misidentification of the common bile duct (CBD) by the surgeon. Other risk factors include inadequate exposure, patient obesity, congenital anatomic anomalies of the bile ducts, emergent surgery, and failed cholangiography. The incidence of bile duct injury after LC is 0.1% to 1.3%, and although there does not appear to be a significant difference in the incidence of bile duct injuries compared with open procedures, injuries after LC may possibly be more severe. , ,
Bile duct injuries encompass a wide range of different lesions, including tears, transections, and ligations. The most common injury results in a defect of the CBD due to a portion of the CBD having been mistaken for the cystic duct and, as a result, being partially or completely transected. Many minor bile duct injuries (perhaps seen in up to 1.2% of patients) are now successfully treated with endoscopic management (usually internal drainage), allowing bile flow away from the site of injury into the duodenum and consequently allowing the injured bile duct segment to heal. On the other hand, complex or severe bile duct injuries (i.e., common hepatic duct, CBD, right hepatic duct, or transection of the right posterior sectoral duct) are almost always treated with surgical biliary reconstruction. ,
There is debate within the surgical literature as to whether the routine use of intraoperative cholangiography (IOC) can help reduce the incidence of bile duct injury, and some surgeons advocate that cholangiography should constitute a routine component of every LC. Proponents argue that IOC can help better define biliary anatomy, thereby reducing the incidence of biliary injuries. Moreover, in those cases in which injuries occur, proponents argue that IOC allows earlier discovery of these injuries. However, those who argue against routine cholangiography suggest that instead of reducing the incidence of bile duct injury, surgeons performing IOC may actually cause a bile duct injury while attempting to cannulate the cystic duct or by inadvertently cannulating the CBD. Moreover, IOC undoubtedly increases operative time and surgical costs.
Depending on its severity, bile duct injury can result in a frank bile leak ( Figs. 52.1 – 52.3 ). Whereas bile leaks can theoretically occur at any site of bile duct injury, the most common locations are the cystic duct stump, the duct of Luschka, and the gallbladder bed. When leaks occur at the cystic duct stump (the most common site of bile leak), causes can include a misplaced surgical clip, resulting in inadequate closure of the cystic duct; necrosis of the cystic duct after placement of a clip; elevated CBD pressures (often due to a distally impacted CBD stone) transmitted to the cystic duct, resulting in cystic duct “blow-out”; and operative injury to the cystic duct. In those cases attributable to operative injury, leaks may occur because of difficulty in dissecting the cystic duct and common hepatic duct, particularly when adhesions are present, and as a result of unrecognized aberrant ducts. The second most common site of bile leak is from the duct of Luschka, an accessory duct in the right hepatic lobe that traverses the gallbladder fossa and can drain into either the right or common hepatic duct. This bile duct is uniquely vulnerable to injury and leak as a result of its variable course and location within the operative field.
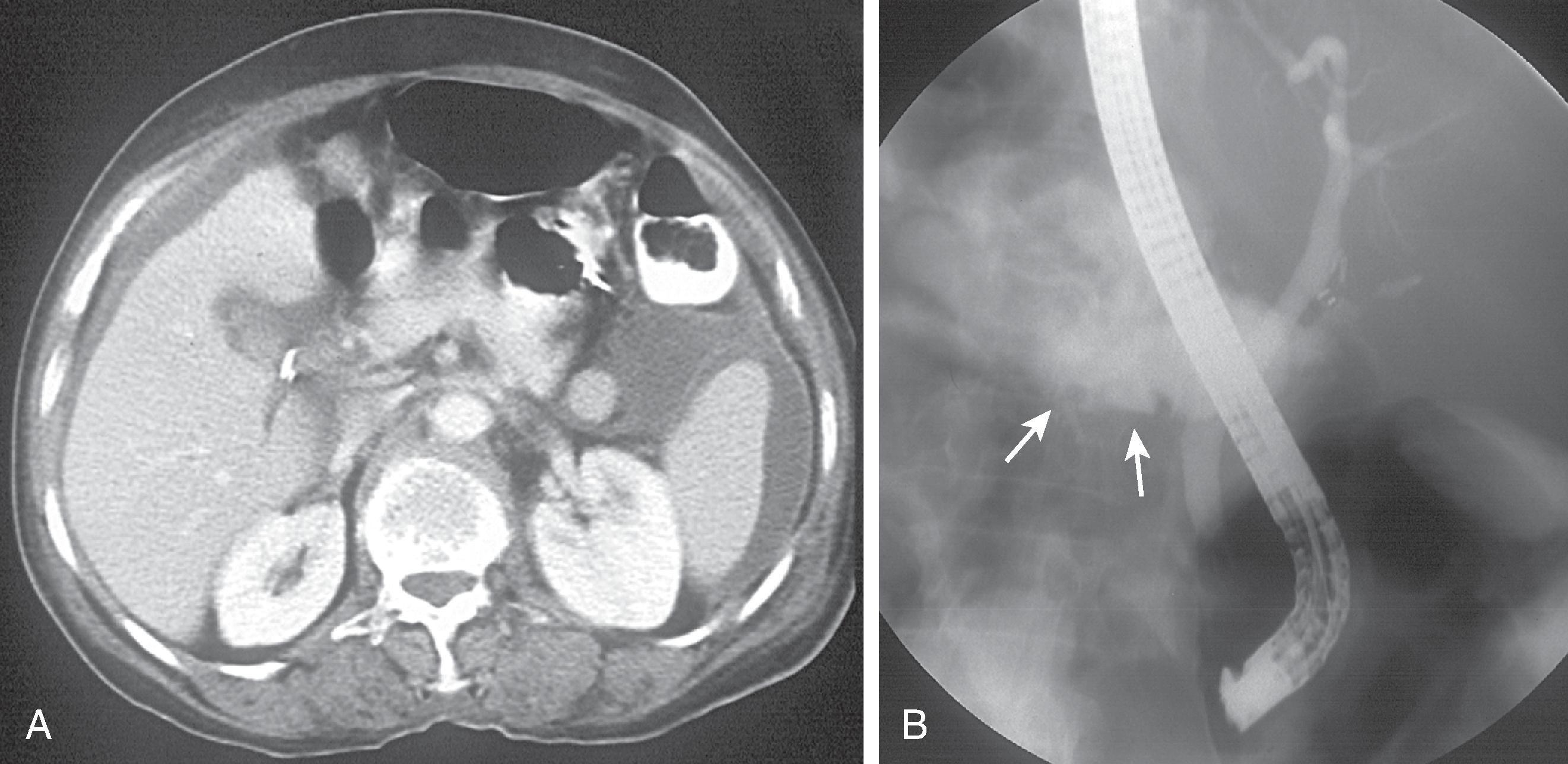
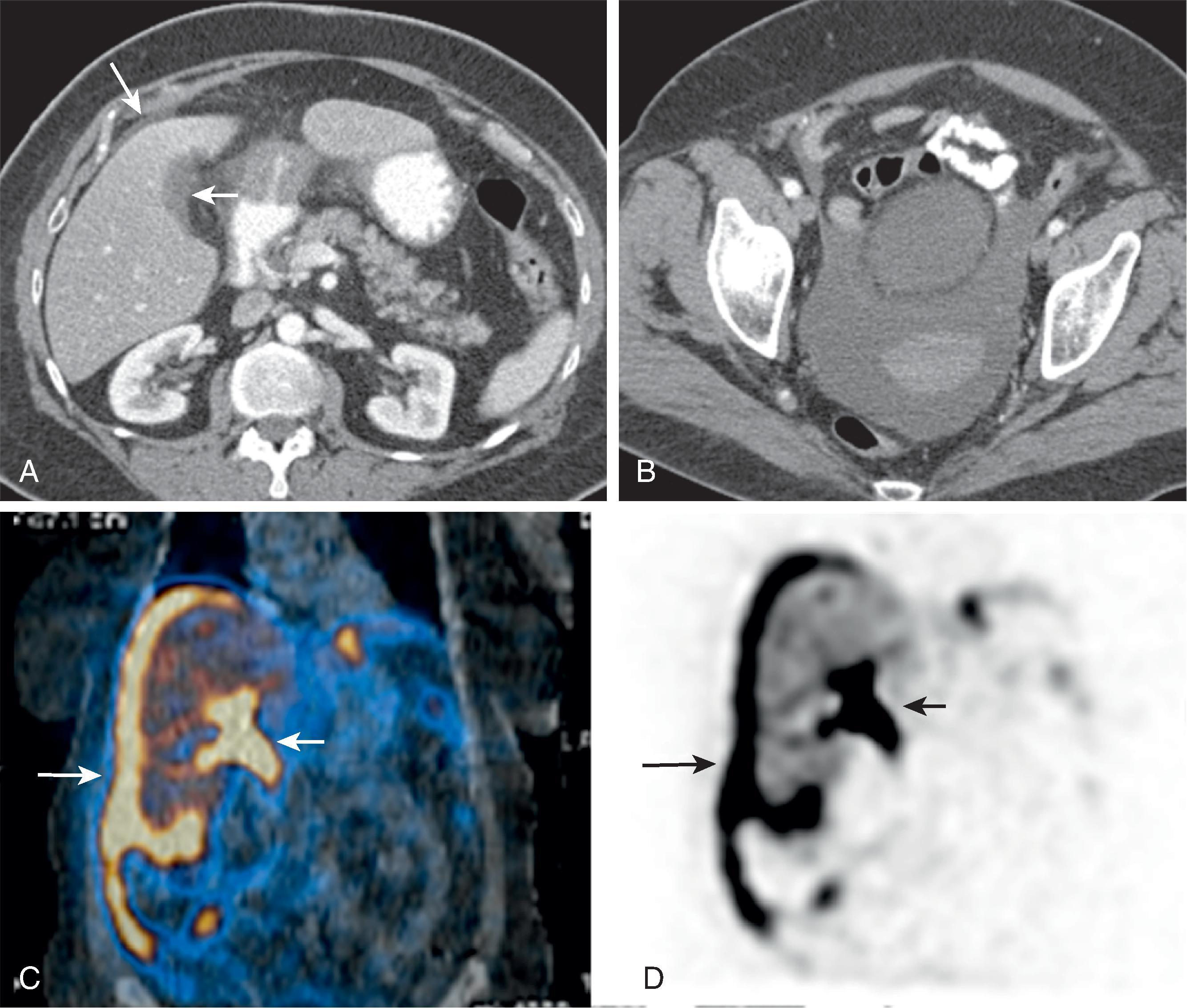
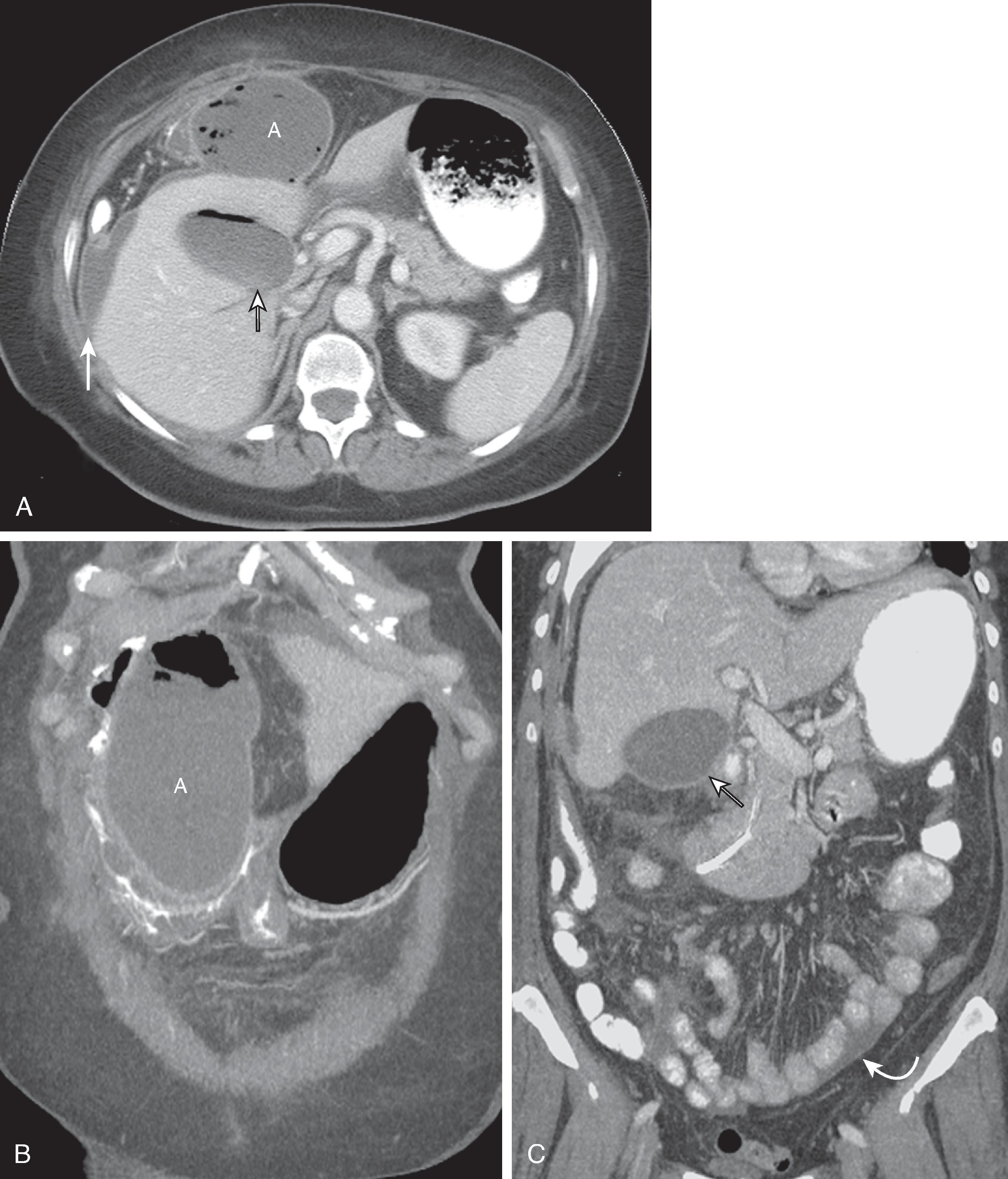
Bile leaks carry a high risk of morbidity and mortality and should be suspected in any patient who presents with fever, jaundice, abdominal pain, peritonitis, or elevated liver function test results in the first week after surgery. , , In particular, a markedly elevated serum bilirubin level and, alternatively, the presence of significant bile output from an abdominal drain are both features highly suggestive of a large biloma, although the absence of bile output from an abdominal drain cannot exclude a bile leak. Bile can leak freely into the peritoneal cavity, resulting in either sterile or infected biliary ascites (see Figs. 52.1 – 52.3 ), or accumulate into a loculated fluid collection, resulting in a sterile biloma (see Fig. 52.3A ) or an infected abscess ( Fig. 52.4 ). ,
Small biliary stones occasionally remain after LC, often within the intrahepatic or extrahepatic biliary tract. Moreover, in some cases in which LC is technically challenging as a result of difficulty in identifying anatomic landmarks, adhesions, marked bleeding, or severe gallbladder inflammation, portions of the gallbladder infundibulum may be inadvertently left behind (subtotal cholecystectomy), and this gallbladder remnant may contain stones. Such incomplete resection of the gallbladder is relatively common, occurring in up to 13.3% of cholecystectomies. For the same reasons, particularly in patients with an unusually long cystic duct, portions of the cystic duct containing stones may also be left behind after surgery.
These retained stones, regardless of whether they reside within the intrahepatic biliary tree, CBD, cystic duct stump, or gallbladder remnant, may subsequently migrate distally into the CBD, resulting in biliary obstruction. The overall incidence of retained stones, regardless of location, after LC is 0.5%; the most common location for retained stones is within the CBD, with an incidence ranging between 5% and 15%. , There is some debate in the literature as to the necessity of defining the presence of biliary tract stones (outside the gallbladder) by preoperative magnetic resonance cholangiopancreatography (MRCP), and some surgeons advocate performing IOC for the purpose of detecting biliary stones in the highest risk patients during cholecystectomy. ,
It is thought that retained stones in the biliary system after cholecystectomy may be a common cause for postcholecystectomy syndrome, a term used to describe the recurrent biliary colic symptoms suffered by 10% to 40% of patients after cholecystectomy. Symptoms of retained biliary stones can include jaundice and right upper quadrant pain, and the diagnosis is usually made in the first 2 months postoperatively. , Rarely, retained distally impacted stones in the CBD may secondarily result in biliary leakage from the cystic duct remnant by causing increased biliary pressure that displaces the cystic duct clips, a phenomenon often referred to as cystic duct blow-out. Retained stones can usually be extracted by endoscopic retrograde cholangiopancreatography (ERCP) and sphincterotomy. Open or laparoscopic CBD exploration is only rarely necessary. , ,
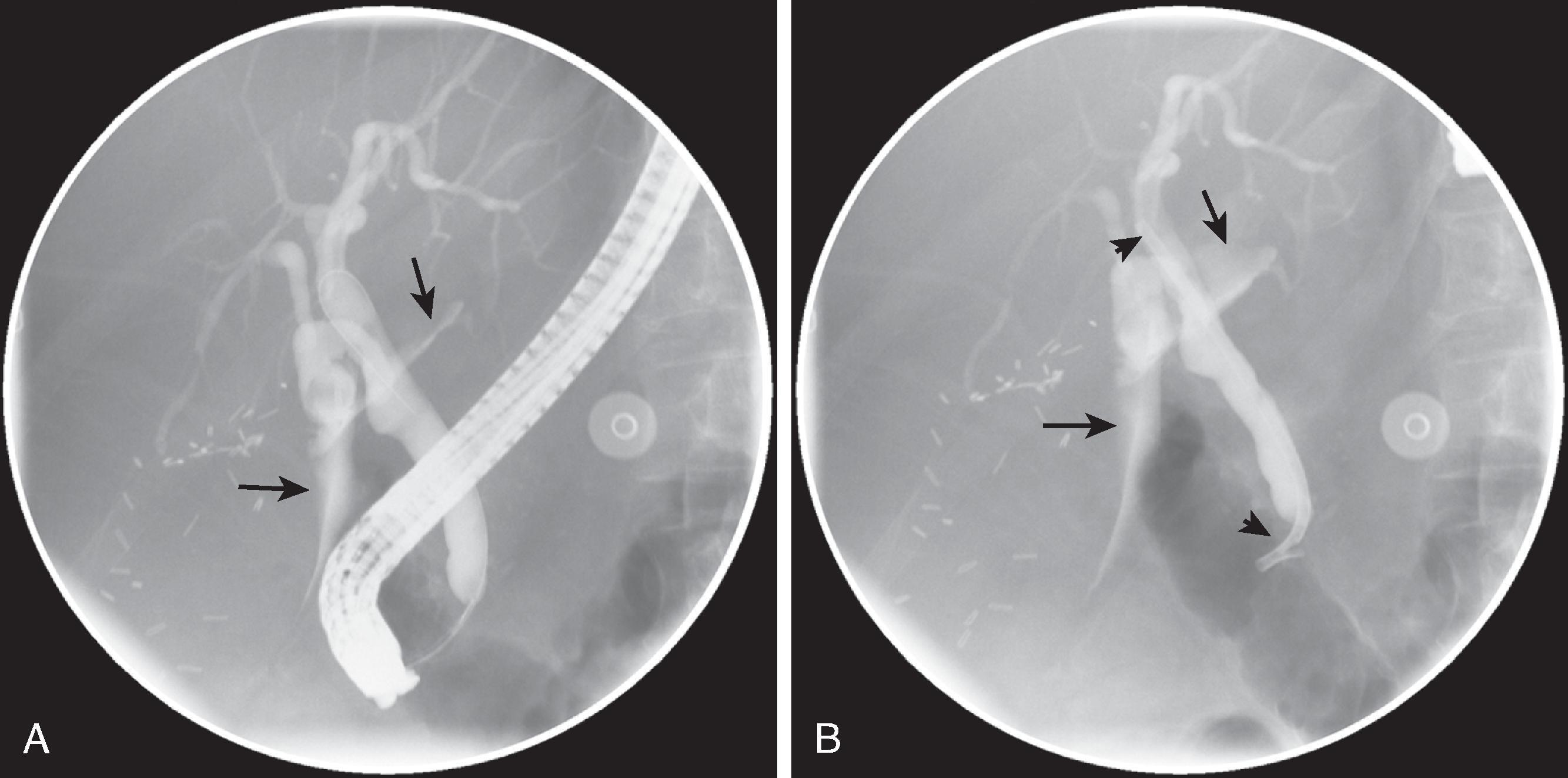
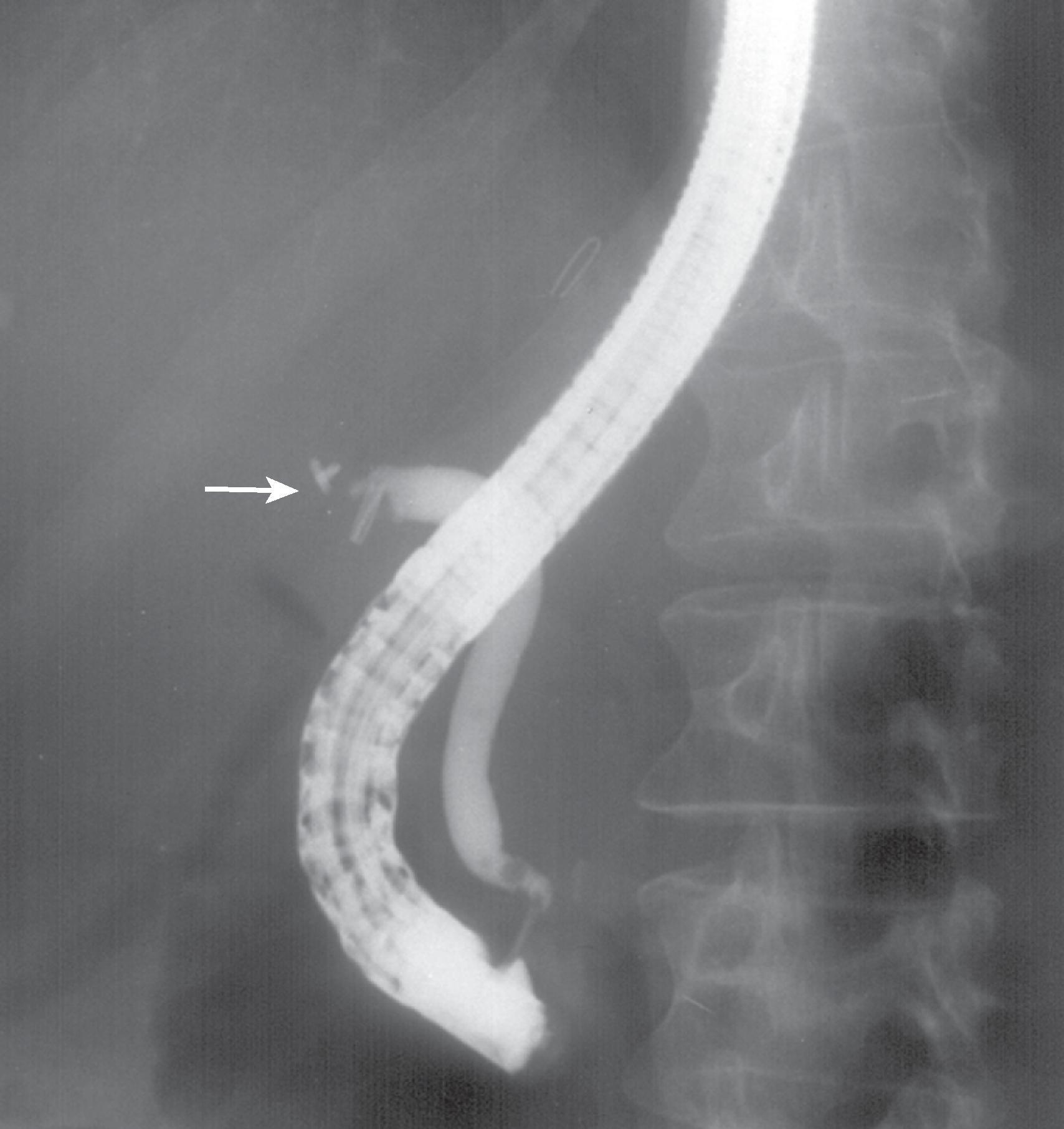
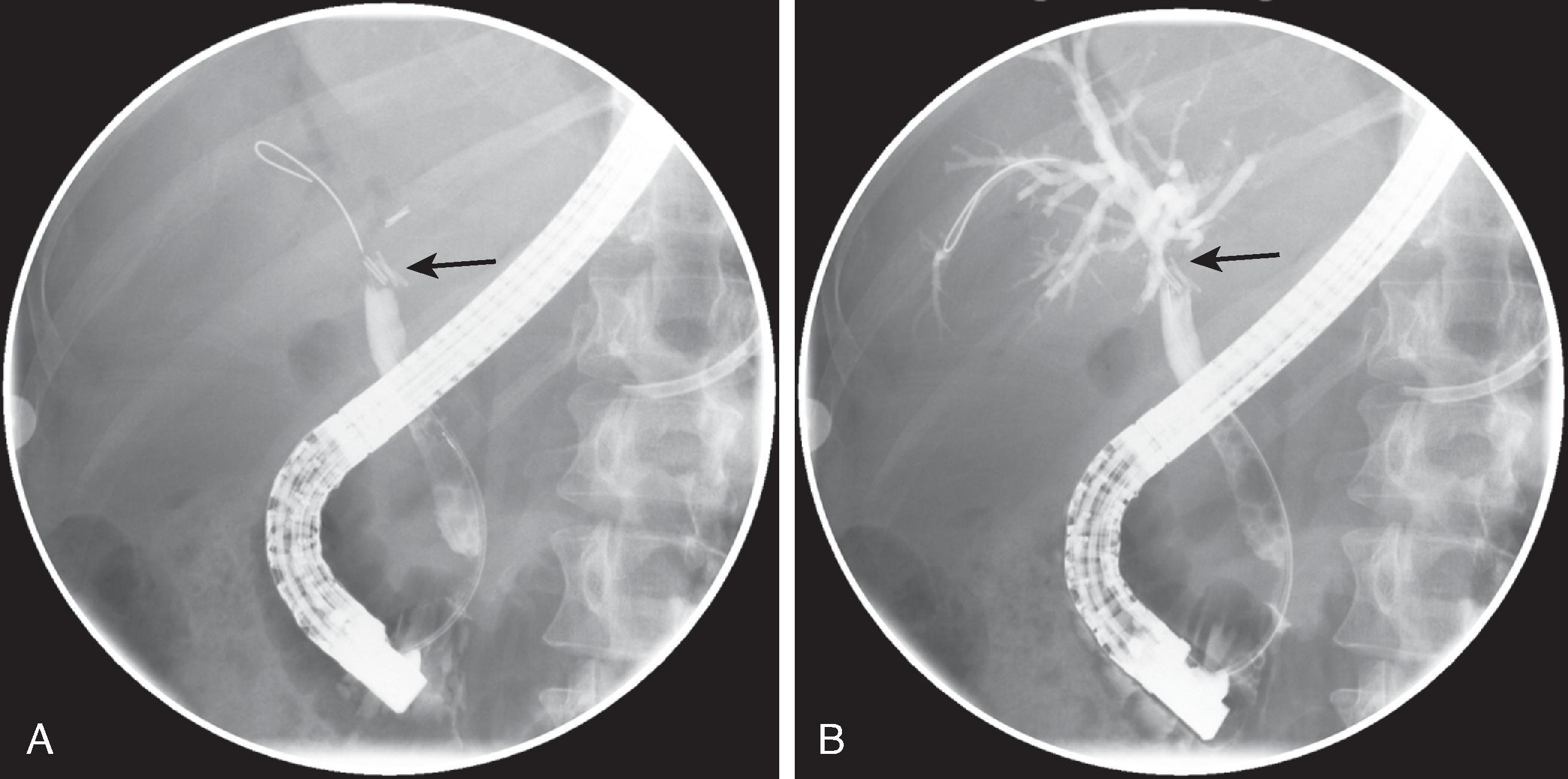
Postoperative biliary strictures are not uncommon with both open and laparoscopic cholecystectomies. Several different causes have been proposed, including focal bile duct ischemia due to intraoperative damage and thermal injury during surgical dissection, intense connective tissue response with fibrosis and scarring as a result of bile duct manipulation, inadvertent clipping or ligation of the bile duct, and scarring as a result of T-tube placement ( Figs. 52.5 and 52.6 ). , , ,
Biliary stricture after cholecystectomy is relatively rare, occurring in 0.2% to 0.5% of patients. In many cases, these strictures are not recognized for months or years after the patient’s surgery, with a mean time to stricture of 3 to 6 months. Many patients are not overtly symptomatic, and the diagnosis is often made on the basis of progressive biliary dilation on cross-sectional imaging. In other cases, patients can present with painless jaundice, cholangitis, or sepsis. Patients with a markedly delayed diagnosis may ultimately present with advanced biliary cirrhosis and its complications.
Whereas surgical treatment (usually in the form of a Roux-en-Y hepaticojejunostomy) has traditionally been the treatment of choice for iatrogenic biliary strictures related to LC, endoscopic treatment is increasingly becoming the first-line treatment of choice. , In addition to being safer and better tolerated (with lesser degrees of associated morbidity and mortality), endoscopic balloon dilation with stent placement has been associated with a lesser risk of recurrent strictures and cholangitis, although patients may require multiple sessions of balloon dilation with periodic replacement of bile duct stents. In particular, endoscopic approaches appear to be more effective for strictures in the distal CBD, whereas surgery may still be the preferred option for complex strictures in the more proximal CBD.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here