Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Adequate post-operative pain control minimizes suffering, improves patient satisfaction, promotes early mobilization, reduces the length of stay, and minimizes costs. Optimal pain control requires pre-operative education and perioperative pain management planning that encompasses a preventative analgesic approach that utilizes multimodal therapies such as systemic analgesia, local anesthetic infiltration, peripheral regional anesthesia, neuraxial analgesia, and cognitive-behavioral modalities. These principles can and should be applied for reconstructive surgery in the developing world.
Inadequate post-operative pain control can lead to poor recovery, function, and quality of life and can increase the risk of persistent post-surgical pain and complications. With over 80% of surgical patients experiencing acute post-operative pain and approximately 75% of those with post-operative pain reporting the severity as moderate or higher, it is important to achieve adequate pain control to minimize suffering, improve patient satisfaction, promote early post-surgical mobilization, reduce the length of hospital stay, and minimize costs.
Optimal post-operative pain control requires pre-operative education and perioperative pain management planning that encompasses a preventative analgesic approach that utilizes multimodal therapies such as systemic analgesia, local anesthetic infiltration, peripheral regional anesthesia, neuraxial analgesia, and cognitive-behavioral modalities. These principles can be adapted for use in reconstructive surgery in the developing world.
Before surgery, it is beneficial for patients to receive information on treatment options as well as on the plan and goals for post-operative pain management. This includes individually tailored education on methods of pain assessment for patients (and/or caregivers) as well as instructions on administration of analgesic modalities. Patients receive better health outcomes when they are able to participate in the decision-making process and adjust their pain management in accordance with their pain level and the presence of adverse effects. Although this may be a challenge when working in developing countries where language and cultural differences exist, engaging patients through interpreters and/or written materials in the local language will provide better health outcomes.
Utilization of a validated pain assessment tool (e.g., visual analog scale, a numeric rating scale, or symbols) is important to track the responses to pain treatments and to allow for proper adjustments. The following assessments should be used to help guide the perioperative pain management plan: what interventions have been effective, how the pain affects function, type of pain (e.g., neuropathic, visceral, somatic, muscle spasms), cultural or language barriers, cognitive deficits and misconceptions, and side effects (e.g., sedation, delirium, nausea/vomiting, constipation).
Acute surgical pain occurs when inflammation is caused by tissue injury (e.g., surgical incision, dissection, burns) and/or direct nerve injury (e.g., nerve stretching, compression, transection). The patient senses pain through the afferent pain pathway ( Fig. 1.8.1 ), which can be targeted by various analgesic drugs. The multimodal analgesic approach utilizes several drugs, each acting at different sites of the pain pathway, to provide superior synergistic pain relief compared with a single drug. By relying less on a single drug class such as opioids, opioid-related adverse effects are minimized.
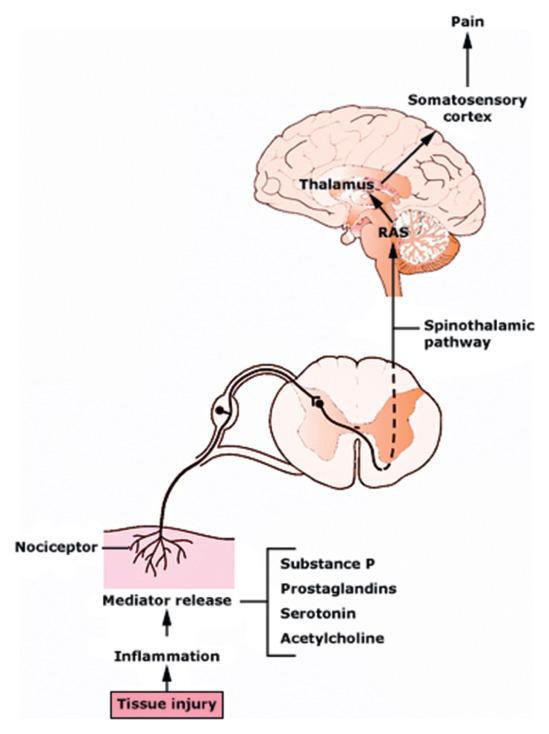
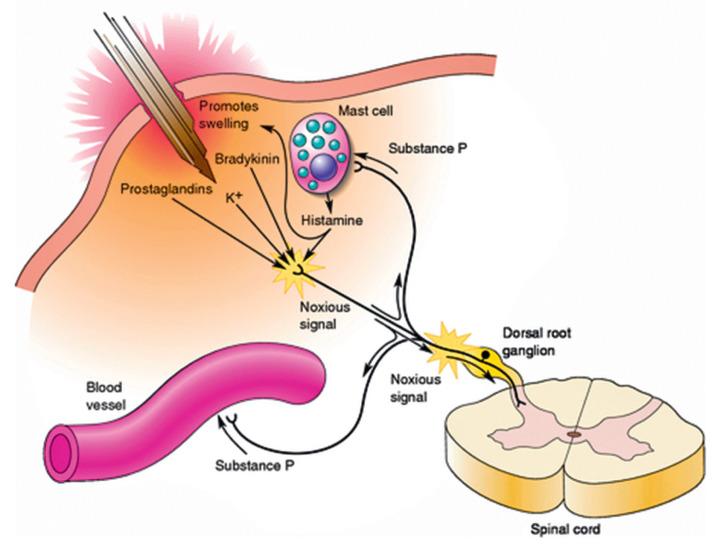
When tissue injury occurs, the release of local inflammatory mediators leads to hyperalgesia (i.e., an increased response to a painful stimulus) and allodynia (i.e., a painful response to a normally innocuous stimulus) ( Fig. 1.8.2 ). Once the pain pathway is activated, sensitization of the peripheral pain receptors (primary hyperalgesia) and increased excitability of central nervous system neurons (secondary hyperalgesia) also contribute to hyperalgesia and allodynia. Preventative analgesia is a strategy to augment peripheral and central nervous system processing of painful stimuli, thereby reducing central sensitization, hyperalgesia, and allodynia. Preventative administration of analgesic modalities throughout the perioperative period includes preemptively administrating analgesia before surgical tissue trauma. By minimizing sensitization, preventative analgesia effectively reduces post-operative pain and/or analgesic consumption beyond the duration of action of the treatment drug or technique. Evidence-based analgesic modalities available for post-operative pain control include opioids, acetaminophen/paracetamol, nonsteroidal anti-inflammatory drugs (NSAIDs), cyclooxygenase-2-specific inhibitors, anti-convulsants, IV lidocaine infusion, steroids, ketamine, local anesthetic infiltration, peripheral regional anesthesia, and neuraxial analgesia ( Table 1.8.1 ) .
| Cleft Lip | Cleft Palate | Burn Skin Grafting | Upper-Extremity Procedures | Lower-Extremity Procedures | |
|---|---|---|---|---|---|
| Pre-operative |
|
|
|
|
|
| Intra-operative |
|
|
|
|
|
| Post-operative |
|
|
|
|
|
Opioids continue to be widely used for post-operative pain control because they provide rapid and potent analgesia—especially when given intravenously. They can also be given through oral, intramuscular, subcutaneous, transdermal, and transmucosal routes. If not contraindicated, the route of choice is orally for short-acting opioids, given the need for round-the-clock dosing to manage continuous pain during the first 24 hours after surgery. There is no difference in IV vs. oral administration. Insufficient equipment, facilities, and support personnel common in developing countries prevent the use of patient-controlled analgesia. Avoid using the intramuscular route given its unreliable absorption and associated pain on injection. Appropriate monitoring of sedation and respiratory status with nurse observation, pulse oximetry, and/or capnography is recommended. Other common side effects such as nausea/vomiting, pruritus, and opioid-induced constipation should be treated with anti-emetics and bowel regimens; alternatively, the opioid can be changed or its dose adjusted accordingly.
Intravenous opioids are given at the lowest effective dose on an as-needed basis until either pain relief is achieved or adverse effects are present (e.g., excess sedation, hypoventilation, hypotension, etc.). Common opioids used for pain control that are available in developing countries include:
Fentanyl (adult: 25–100 mcg ≥ q5min; pediatrics: 0.5–1 mcg/kg ≥ q5min): Onset is 1 min; peak effect is 3 to 5 min; duration is 0.5 to 1 hr. Decrease dose in renal dysfunction.
Morphine (adult: 1–5 mg ≥ q10min; pediatrics: 0.02–0.1 mg/kg ≥ q10min): Onset is 1 to 2 min; peak effect is 30 to 60 min; duration is 3 to 4 hr. Histamine release may cause flushing, hypotension, tachycardia, pruritus, and bronchospasm. Decrease dose in renal dysfunction.
Oral opioids should be prescribed at the lowest effective dose and shortest effective treatment duration. Reduce the dose in patients with renal and liver dysfunction. They are more effective when combined with acetaminophen and/or ibuprofen. The most readily available oral opioid in the developing world is codeine:
Codeine (adults: 15–60 mg q4–6 hr; pediatrics: 3–12 years old: 0.5–1 mg/kg q4–6 hr): Onset is 30 to 45 min; peak effect is 60 to 120 min; duration is 4 hr. The liver's CYP2D6 converts codeine into codeine-6-glucuronide and morphine with genetic variability in the drug's metabolism. As a result, some patients have inadequate pain relief, whereas others who are “ultrarapid metabolizers” (e.g., children and those with obstructive sleep apnea) have a much stronger effect and are at risk for respiratory depression after taking standard doses of codeine.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here