Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Computed tomography (CT) is the most common imaging modality for evaluation of the pancreas after surgery. Complications that can be detected on CT include anastomotic leak, abscess, fistula, and bleeding (see Chapters 62 and 117 ).
Fluid collections, such as seromas, abscesses, and pancreatic pseudocysts, can be identified on CT ( Fig. 28.1 ). Rim enhancement suggests abscess or pseudocyst. Gas within a collection suggests infection or enteric leak. Enteric leaks can have a thin tract containing gas and fluid, extending from an enteric anastomosis to an abscess. Oral contrast given before the CT can leak into the abscess, which is diagnostic of an enteric leak.
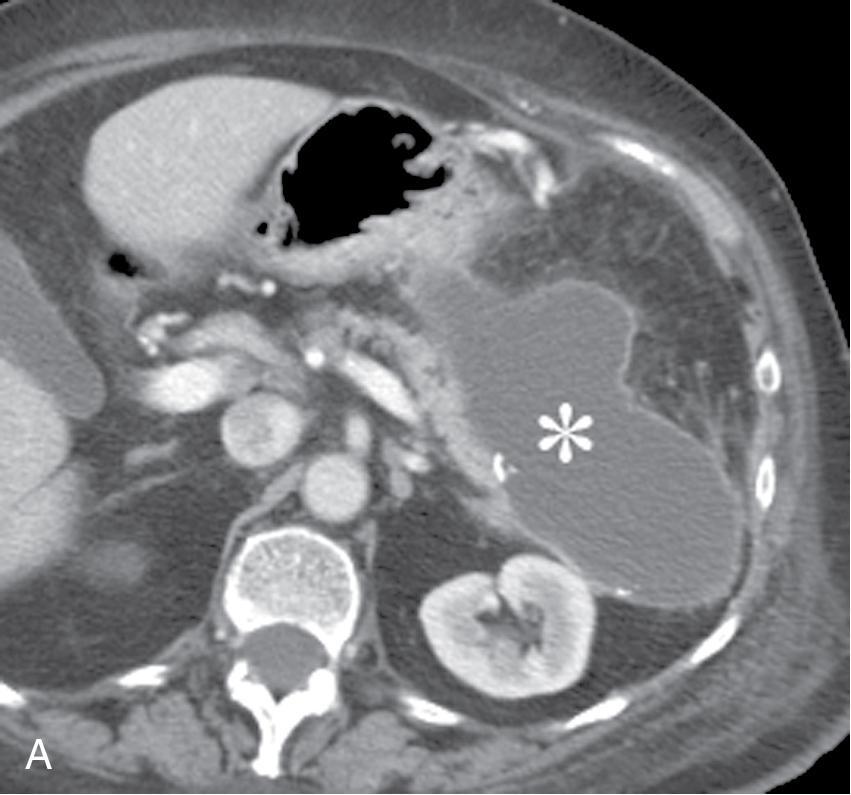
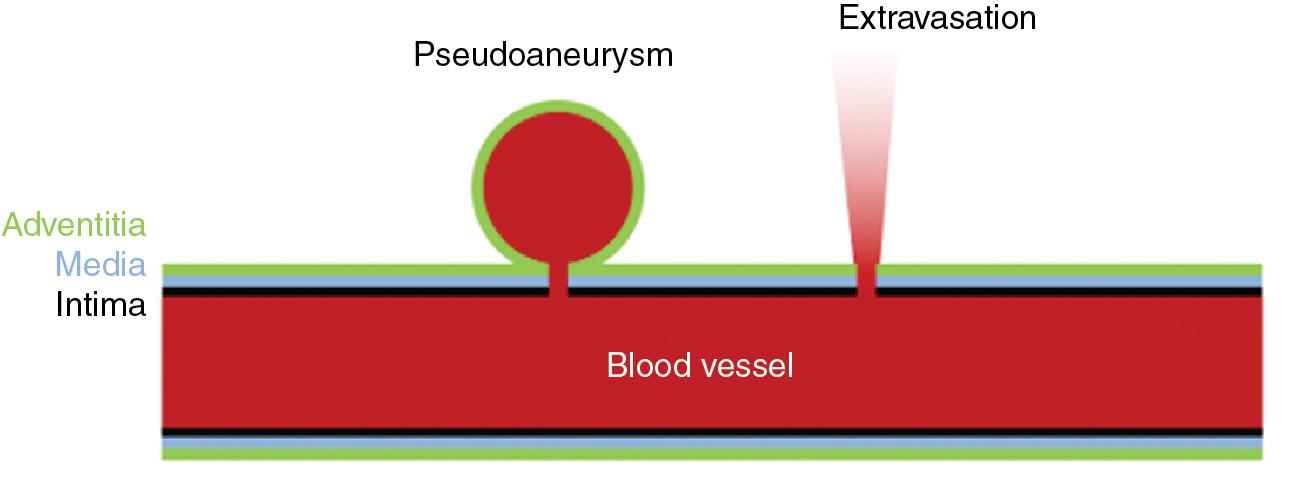
Postoperative bleeding can be evaluated using a CT angiogram, which should include noncontrast and arterial phases. Hematomas are visible on noncontrast CT as high density (greater than 20 Hounsfield units) collections. Active arterial bleeding is seen as extravasation of contrast on arterial phase contrast-enhanced CT (CECT) scans. On delayed phase images (if obtained), the extravasated contrast continues to spread if there is active bleeding. On the other hand, a pseudoaneurysm (which can bleed intermittently) is an enhancing structure next to an artery, which maintains its shape on delayed CT images ( Figs. 28.2 and 28.3 ).
Magnetic resonance cholangiopancreatography (MRCP) is a fluid-sensitive magnetic resonance imaging (MRI) sequence that clearly shows the pancreatic duct, bile ducts, fistulas, and fluid collections. The MRCP is typically reconstructed into axial and coronal slices, as well as a three-dimensional (3D) images. The site of a pancreatic fistula can be identified in 75% of patients on CT, compared with 93% on MRCP.
Many postpancreatectomy complications are managed using image-guided percutaneous interventions, reducing the need for reoperation. After pancreaticoduodenectomy, 12% to 22% of patients require percutaneous intervention, , including intra-abdominal abscess drainage (72%), percutaneous biliary drainage (PBD; 18%), and angiography with or without embolization (10%).
Postoperative abscesses can be drained percutaneously, using ultrasound or CT guidance (see Fig. 28.1 ). Small abscesses (<3 cm) can usually be treated with antibiotics alone, but larger collections require both antibiotics and drainage. Complications of image-guided drainage of fluid collections are infrequent but include bleeding, sepsis, and peritonitis.
Abscesses are typically drained using the Seldinger technique. A needle is advanced into the collection under ultrasound or CT guidance. After aspirating fluid, a stiff guide wire is placed through the needle into the collection. The needle is then removed, and a drain is placed over the wire into the collection. Typically, 8 to 10 French (Fr) drains are placed in thin, serous collections, and 10 to 12 Fr drains are placed in thick bloody or purulent collections. Larger drains are available for very thick collections, up to 20 Fr for locking loop drains and 36 Fr for straight drains. Biliary-type drains (which have additional side holes) may be helpful for long, multiloculated collections.
After catheter placement, the abscess is emptied, and specimens are sent for gram stain and culture. The fluid can also be sent for amylase (to evaluate for pancreatic leak) and bilirubin (to evaluate for bile leak). Drain fluid to serum bilirubin ratio greater than five indicates a bile leak, and drain amylase to serum ratio greater than five indicates a pancreatic leak.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here