Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
This chapter includes an accompanying lecture presentation that has been prepared by the authors: ![]() .
.
Prone positioning is likely the most common position in spine surgery, but it is associated with distinct physiologic changes (especially cardiopulmonary) and may carry the greatest risk for vertebral venous engorgement (and subsequent blood loss) in comparison with supine or lateral patient positioning.
Proper positioning of patients for prone spine surgery involves keeping the abdomen free from external compression to limit vertebral venous engorgement and surgical blood loss; this was a central concept driving the development of various frames and positioning devices.
Optimal intraoperative sagittal contour is critical for proper patient positioning and should be determined by the goals of surgery: decompression versus instrumentation/arthrodesis may warrant either reduction or preservation of lordosis, respectively.
The Jackson table system is the most common surgical table/frame used in spine surgery; there are multiple modular components to support prone, supine, and lateral patient positioning.
The Wilson strap-on frame, which can be used with a standard table or Jackson table, consists of two laterally placed longitudinal support pads that are adjusted for optimal intraoperative sagittal contour while keeping the patient’s breasts, abdomen, and genitalia free from compression.
Ulnar neuropathy and brachial plexopathy can be caused by compression and/or overstretching; these are the most common upper extremity position-related peripheral nerve injuries, but the risk for these complications may be reduced with intraoperative neuromonitoring and prompt repositioning.
Meralgia paresthetica is a common position-related complication of spine surgery and usually has a benign course.
Postoperative vision loss is a rare but potentially devastating complication after spine surgery; risks include prone positioning, prolonged operative duration, high blood loss, intraoperative hypotension, male sex, and comorbidities.
Risk for postoperative vision loss can potentially be reduced by avoiding direct ocular compression (i.e., proper use of foam headrests or Mayfield clamps), maintaining neutral cervical alignment when possible, and keeping the patient’s eyes above the level of the heart with 10-degree reverse Trendelenburg positioning.
For trauma patients with unstable injuries, supine transfer onto the flat-top Jackson table and then initiation of the 180-degree rotation sequence may limit unstable segmental motion during prone positioning.
Positioning on the operating table is one of the most critical first steps in performing any spine surgery procedure. The ideal position for spine surgery should facilitate access and ease of exposure while simultaneously minimizing the risk for bleeding, the likelihood of damage to vital structures, and other inherent postoperative morbidity. Many important precautions and considerations are necessary to achieve optimal safe positioning. Over the years there have been several advancements, including improvements in operating tables, frames, and other devices, aimed to make surgery safer and more efficient and ergonomic. We review some of these major advancements and discuss common equipment currently available to spine surgeons. Traditionally, supine and prone positioning were the most common positions for spine operations, but development of minimally invasive techniques has resulted in increasing use of lateral patient positioning for transpsoas or prepsoas approaches. In this chapter, we review important principles of positioning for spine surgery, with special consideration and focus on strategies to reduce the risk for complications.
Many important innovations and advancements in positioning for spine surgery occurred during the 20th century. Some of this progress can be understood as an attempt to achieve two goals during prone lumbar spine surgery: (1) limiting vertebral venous engorgement for blood loss reduction and (2) maintaining optimal lumbar sagittal contour (i.e., reduced lordosis for decompression/discectomy versus accentuating lordosis for instrumentation/arthrodesis). In comparison with supine or lateral positions, the prone position carries a greater risk for vertebral venous engorgement. When patients are prone, there can be increased intra-abdominal pressure from extrinsic factors such as poorly placed sandbags or bolsters. Subsequent elevations in central venous pressure may preferentially divert returning blood into the normally low-pressure valveless, thin-walled vertebral veins via the Batson plexus. , Moreover, chest restriction in the prone position can lead to decreased pulmonary compliance, higher airway pressures, decreased cardiac venous return and output, and ultimately higher central venous pressures. , The result is further vertebral venous engorgement with potentially increased surgical blood loss. Therefore, keeping the prone patient’s abdomen free from restriction was a guiding principle for many positioning techniques, tables, and frames. This includes positions previously described for lumbar decompression/discectomy ( Fig. 25.1 ): Ecker’s kneeling position (1949), Lipton’s Mohammedan praying position (1950), Tarlov’s knee-chest position (1967), and Wayne’s tuck position (1967). These surgeons recognized the relationship among restrictions on the prone patient’s abdomen, increased venous pressure, engorged tissue, and prevention of surgical “ooze” for blood loss reduction. Another potential benefit with these positions was that reduced lumbar lordosis, achieved through hip flexion, could widen interlaminar spaces to improve disk access with less bony removal. Also, knee flexion could relax affected lumbar/lumbosacral nerve roots, resulting in less root tension during retraction for disk exposure.

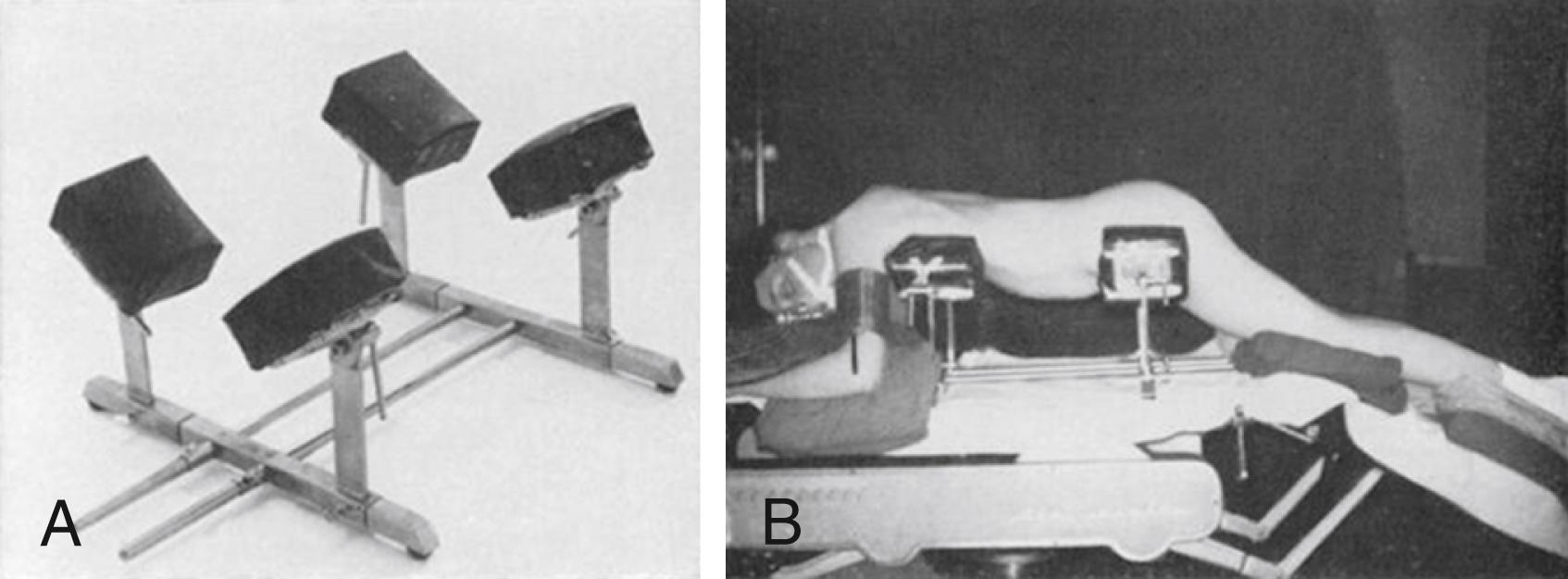
Several frames for lumbar decompression/discectomy were designed based on these principles. In 1969, Hastings described the Canadian frame with modifications to minimize overstretching the patient’s joints in the knee-chest position. The Heffington frame and Cloward surgical saddle were also devices proposed by neurosurgeons with similar objectives. , In 1979, the Andrews frame was described using the modified knee-chest position. The frame’s adjustable tibial support was lowered to achieve 90-degree hip flexion for reduced lumbar lordosis. , The frame’s tibial support could be adjusted to decrease hip flexion for lumbar fusion operations. , Currently, the most common strap-on frame used for lumbar decompression/discectomy is the Wilson frame (see the next section for further details). ,
Positioning for lumbar instrumentation/arthrodesis and/or reconstructive surgery must balance the goals of abdominal decompression and lordosis preservation. With Harrington rod instrumentation increasingly utilized in the 1960s, Relton and Hall designed the first frame to adequately support these scoliosis operations without allowing external pressure on the anterior abdominal wall ( Fig. 25.2 ). The Relton-Hall frame (Imperial Surgical, Dorval, Quebec, Canada) consisted of four well-padded vertical supports arranged in two V-shaped pairs to support the upper thoracic cage and iliac crests ( ![]() ). The vertical supports were set at a 45-degree inward tilt and were individually adjustable for length and width to avoid compressing the abdomen. Use of the frame was associated with less blood loss during Harrington rod scoliosis operations. Currently, the most commonly used spine surgery table system for scoliosis operations is the Jackson Modular Table System (Mizuho OSI, Union City, CA), which is discussed in the following section.
). The vertical supports were set at a 45-degree inward tilt and were individually adjustable for length and width to avoid compressing the abdomen. Use of the frame was associated with less blood loss during Harrington rod scoliosis operations. Currently, the most commonly used spine surgery table system for scoliosis operations is the Jackson Modular Table System (Mizuho OSI, Union City, CA), which is discussed in the following section.
Cushioning the head and protecting the face and eyes are important for proper spine surgery positioning. ![]() demonstrates common equipment for face protection and cranial stabilization during spine surgery, which includes the Mayfield skull clamp (Integra, Plainsboro, NJ), Gardner-Wells tongs, and the Caspar head holder. Some anterior approaches with supine patients may simply require pillows and/or cushions for head support. For prone procedures, cushions with eye and endotracheal tube cutouts are commonly used (e.g., GentleTouch Pillow [Mizuho OSI, Union City, CA] and ProneView Protective Helmet System [Dupaco, Oceanside, CA]). Studies have demonstrated that the ProneView Protective Helmet is superior to other foam face cushions, including the OSI pillow, for reducing forehead and chin tissue interface pressures during prone spine surgery. ,
demonstrates common equipment for face protection and cranial stabilization during spine surgery, which includes the Mayfield skull clamp (Integra, Plainsboro, NJ), Gardner-Wells tongs, and the Caspar head holder. Some anterior approaches with supine patients may simply require pillows and/or cushions for head support. For prone procedures, cushions with eye and endotracheal tube cutouts are commonly used (e.g., GentleTouch Pillow [Mizuho OSI, Union City, CA] and ProneView Protective Helmet System [Dupaco, Oceanside, CA]). Studies have demonstrated that the ProneView Protective Helmet is superior to other foam face cushions, including the OSI pillow, for reducing forehead and chin tissue interface pressures during prone spine surgery. ,
The three-pronged Mayfield skull clamp can maintain rigid, stable cranial positioning during posterior cervical spine operations. For adults, the recommended force application across the clamp is 60 to 80 lbs. Skull fracture and epidural hematoma are rare complications associated with Mayfield pin application. Next, Gardner-Wells tongs can also be attached to the patient’s head when cervical traction is needed. Pulleys connected to the Gardner-Wells tongs can be used to adjust cervical spine alignment (e.g., bivector traction) during cervical spine operations ( Fig. 25.3 ). Positioning setups with weighted chin straps, rather than skull tongs, can also achieve optimal intraoperative cervical alignment ( ![]() ). The Caspar head holder, which can be used for anterior cervical discectomy and fusion (ACDF) positioning, utilizes an elastic chin strap and neck cushion for cervical extension while pulling the mandible away from the operative field.
). The Caspar head holder, which can be used for anterior cervical discectomy and fusion (ACDF) positioning, utilizes an elastic chin strap and neck cushion for cervical extension while pulling the mandible away from the operative field.
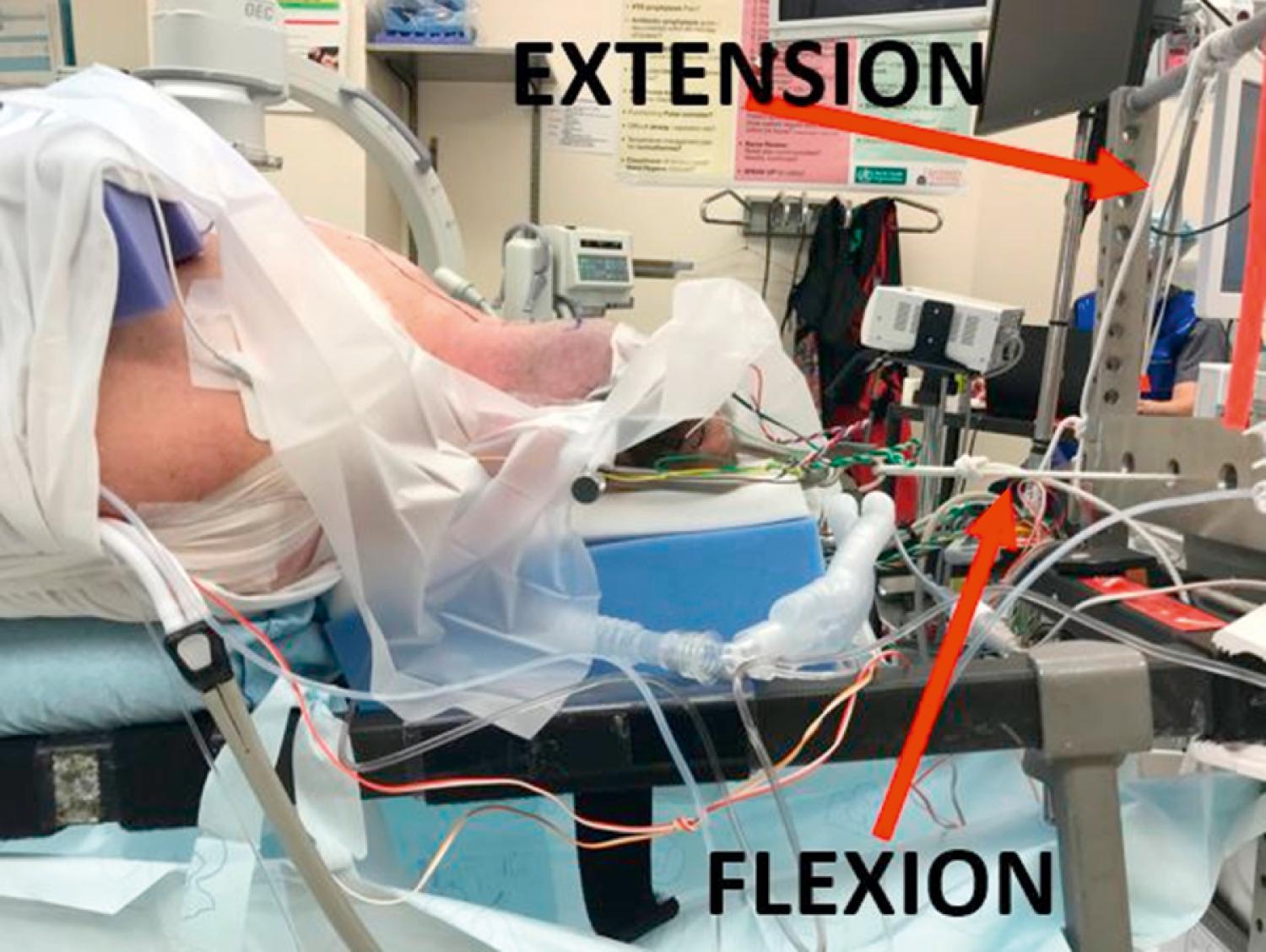
Fig. 25.4 depicts common tables and frames useful for positioning spine surgery patients. In some cases, a standard electrical operating table, modified with various pillows and/or customized cushions/rolls, may safely achieve the desired patient position. For more complex procedures, surgeons often position patients using spine-specific tables/frames such as the Jackson Modular Table System. The Jackson table’s carbon fiber, open-frame design allows unobstructed radiolucency along the entire spinal axis and supports C-arm or advanced navigation imaging acquisition. The Jackson table can be fitted with a spinal top and various modular padded components for prone posterior instrumentation cases ( ![]() ). A padded radiolucent imaging top can be used for operations that require supine or lateral positioning. The Jackson table has 360 degrees of rotational capability for unstable trauma patients or to facilitate anterior-posterior circumferential spine surgery without needing to transfer the patient between approaches (
). A padded radiolucent imaging top can be used for operations that require supine or lateral positioning. The Jackson table has 360 degrees of rotational capability for unstable trauma patients or to facilitate anterior-posterior circumferential spine surgery without needing to transfer the patient between approaches ( ![]() ).
).
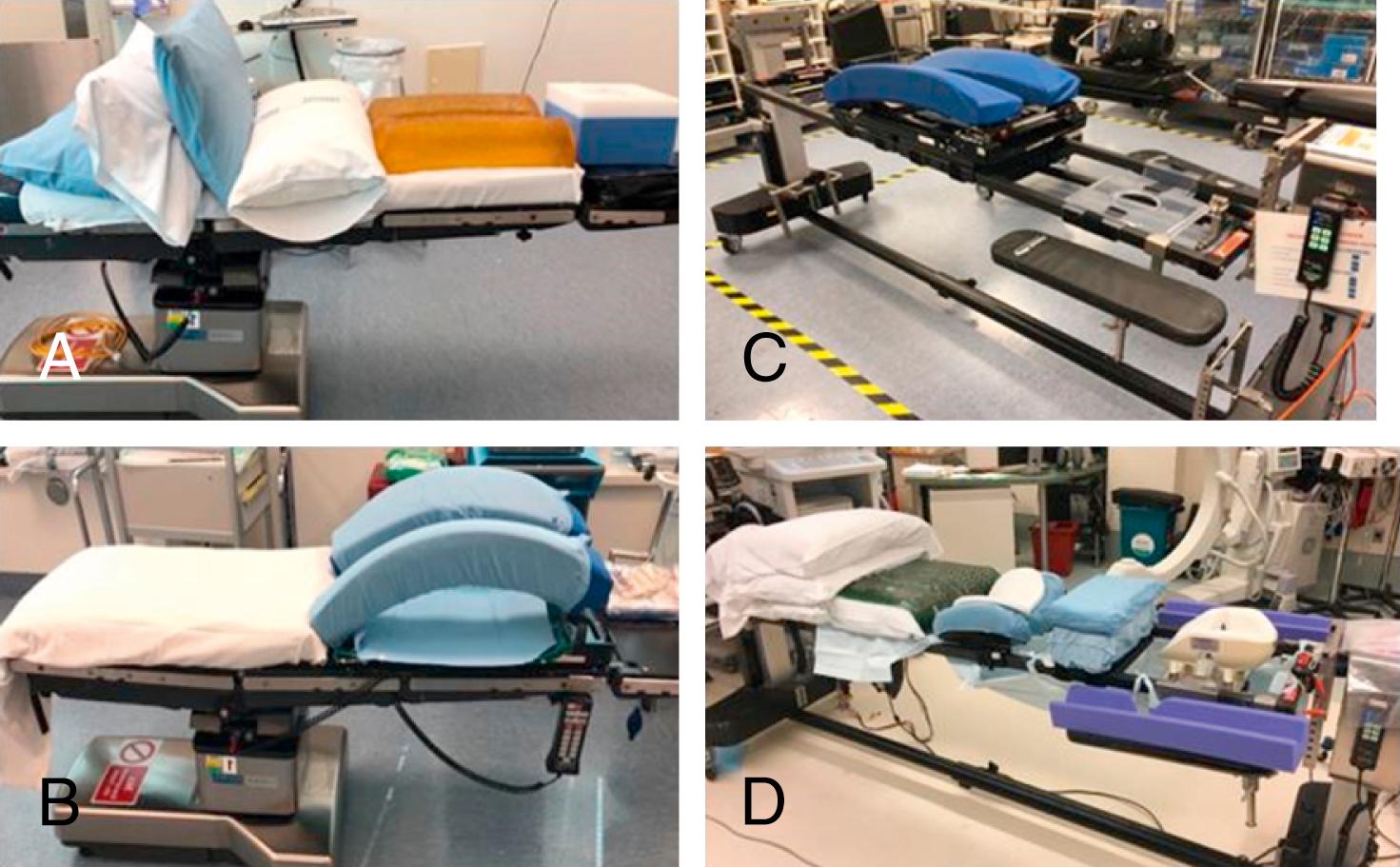
A critical aspect of prone positioning is adjusting the patient’s thoracolumbar sagittal contour to facilitate either reduction or preservation of lordosis, which can be helpful for spinal decompression versus instrumentation/arthrodesis, respectively. To help accomplish this, the modular Jackson table includes a leg sling (reduced lumbar lordosis) and a flat leg board (accentuated lumbar lordosis). A Wilson frame can be fitted to the Jackson table for further manipulation of thoracolumbar sagittal contour. , The Wilson frame consists of two laterally placed, curved full-length support pads for the chest and pelvis, which allow the abdomen, breasts, and genitalia to hang free ( ![]() ). Much like an open-top spinal table, the Wilson frame facilitates reduction of intra-abdominal pressure, which may decrease venous bleeding during surgery. A more recent evolution is the Wilson Plus frame (Mizuho OSI, Union City, CA), which allows 360 degrees of unobstructed radiolucency and intraoperative C-arm integration. The Wilson frame can be used with a standard operating table, which is a common positioning setup useful for lumbar decompression/discectomy (
). Much like an open-top spinal table, the Wilson frame facilitates reduction of intra-abdominal pressure, which may decrease venous bleeding during surgery. A more recent evolution is the Wilson Plus frame (Mizuho OSI, Union City, CA), which allows 360 degrees of unobstructed radiolucency and intraoperative C-arm integration. The Wilson frame can be used with a standard operating table, which is a common positioning setup useful for lumbar decompression/discectomy ( ![]() ). Of note, use of the Wilson frame is a potential risk factor for ischemic optic neuropathy (ION) after spinal fusion surgery (see the “Reducing Position-Related Complications” section later in this chapter).
). Of note, use of the Wilson frame is a potential risk factor for ischemic optic neuropathy (ION) after spinal fusion surgery (see the “Reducing Position-Related Complications” section later in this chapter).
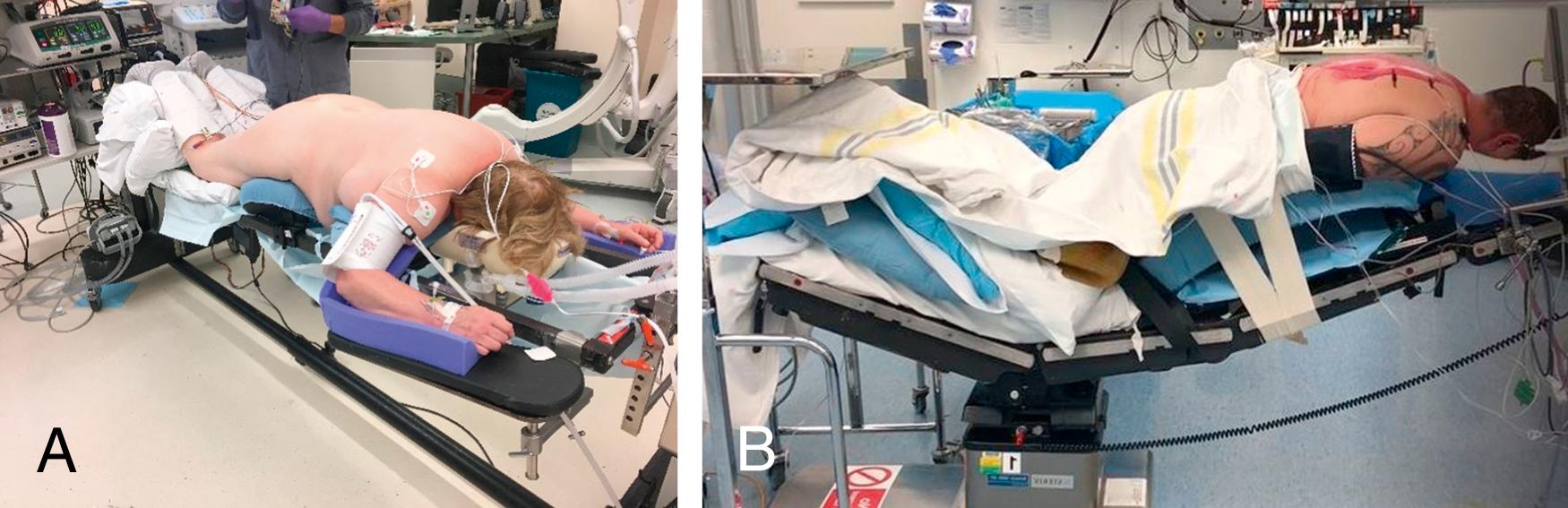
For spinal pathology caudal to the T6–T7 level, the patient’s upper extremities are positioned above the head on padded arm boards with both shoulders abducted and elbows flexed, each less than 90 degrees. Although some sources suggest that patients in prone superman position may comfortably tolerate shoulder abduction greater than 90 degrees, many surgeons still limit shoulder abduction to less than 90 degrees to reduce the risk for brachial plexopathy. To reduce the risk for compression ulnar neuropathy, the surgeon must avoid excessive flexion of the elbow, again using 90 degrees as an upper limit, and ensure that there is adequate padding of the inner arm and elbow, especially at the medial epicondyle. , However, despite meticulous adherence to these precautionary principles, patients placed in the prone superman position may have a higher incidence of position-related impending upper extremity peripheral nerve injury, as detected by somatosensory evoked potentials (SSEPs; see the “Reducing Position-Related Complications” section later in this chapter) compared with nonlateral positions (prone arms tucked, supine arms tucked, supine arms out). , Therefore, the safest approach to positioning involves awareness of these potential risks, clear communication and collaboration between the operating team, and optimal intraoperative monitoring and management of physiologic, position-related parameters. Common indications for prone superman patient positioning include lumbar decompression/discectomy (see ![]() , ) and posterior thoracolumbar instrumentation (
, ) and posterior thoracolumbar instrumentation ( ![]() ). We emphasize the importance of correct operative positioning and its impact on segmental spinal alignment. Peterson et al. previously demonstrated that prone positioning on a Jackson table maintained standing lumbar lordosis and increased lumbosacral lordosis, which are both important considerations when performing reconstructive procedures.
). We emphasize the importance of correct operative positioning and its impact on segmental spinal alignment. Peterson et al. previously demonstrated that prone positioning on a Jackson table maintained standing lumbar lordosis and increased lumbosacral lordosis, which are both important considerations when performing reconstructive procedures.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here