Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The authors are grateful to Mr Stephen O’Neill, consultant transplant surgeon, Belfast City Hospital, for his comprehensive contribution to a previous edition of this chapter.
Surgical management of portal hypertension with portosystemic vascular shunts has essentially been rendered obsolete by the success of less invasive endoscopic and radiological treatments. However, for patients who are suitable candidates, liver transplantation has become the treatment of choice with the unparalleled advantage of curing the underlying liver disease.
Acute variceal bleeding can also present to surgical teams either directly as an undifferentiated gastrointestinal haemorrhage or via referral from gastroenterology following failure of attempted endoscopic control. Therefore, all surgeons should have an understanding of portal hypertension pathophysiology and the management options for various presentations and complications. Pharmacotherapy, endoscopic band ligation (EBL) and radiological treatment with transjugular intrahepatic portosystemic shunts (TIPSS) are the most common treatment modalities for variceal bleeding. Liver transplantation is the definitive treatment for portal hypertension but is restricted to patients with chronic liver disease who fulfil specific criteria that reflect the severity of underlying liver pathology rather than the extent of portal hypertension itself.
This chapter provides an overview of the pathophysiology and management of portal hypertension and its complications with a specific focus on liver transplantation with the aim of bringing the non-specialist up-to-date with current practice and the evidence base.
Portal hypertension arises from a pathological increase in vascular resistance to blood flow within the portal system that leads to a sustained increase in portal blood pressure (normal pressure range 5–10 mmHg). The aetiology of portal hypertension is traditionally subdivided according to the anatomical location within the portal system where the resistance occurs: prehepatic (extrahepatic portal vein), intrahepatic (within the liver) or posthepatic (at the level of the hepatic venous outflow). This is undoubtedly an over-simplification of the pathophysiology (in that many liver conditions are associated with high portal pressure at more than one level); however it remains the most relevant from a surgical perspective and for consideration of treatment options.
Prehepatic causes of portal hypertension include thrombosis of the portal, mesenteric and splenic veins or extrinsic compression of the portal vein itself (e.g. by tumour or lymph nodes). Posthepatic causes of portal hypertension are rare and include thrombosis of the hepatic veins (Budd–Chiari syndrome) or inferior vena cava (IVC), as well as cardiac causes such as right heart failure and constrictive pericarditis. Intrahepatic causes of portal hypertension are by far the most common. In the Western world, liver cirrhosis resulting in sinusoidal obstruction and increased vascular resistance is responsible for 90% of portal hypertension cases. Viral hepatitis and alcoholic liver disease (ALD) are the principal causes of liver cirrhosis, but other common causes include haemochromatosis, primary biliary cirrhosis (PBC) and primary sclerosing cholangitis (PSC).
![]() The 2018 European Association for the Study of the Liver (EASL) Clinical Practice Guidelines for the management of patients with decompensated cirrhosis provides comprehensive evidence-based guidance on the clinical management of complications of cirrhosis (including ascites, infection, bleeding and associated clinical syndromes).
The 2018 European Association for the Study of the Liver (EASL) Clinical Practice Guidelines for the management of patients with decompensated cirrhosis provides comprehensive evidence-based guidance on the clinical management of complications of cirrhosis (including ascites, infection, bleeding and associated clinical syndromes).
Portal hypertension is defined as a sustained increase in the pressure gradient between the portal and systemic venous circulation. This difference can be measured as the ‘hepatic venous pressure gradient’ (HVPG), with a normal range of up to 5 mmHg in healthy adults. HVPG above 6 mmHg is pathological, and clinically significant complications begin to manifest when the pressure gradient rises above 10 mmHg. The incidence of complications from portal hypertension (e.g. ascites, variceal haemorrhage, encephalopathy), and indeed mortality, steadily increases as the portal pressure rises. Whilst HVPG is the gold standard measure for the assessment of portal hypertension, it is seldom used in clinical practice due to the need for invasive central venous catheters and inherent inter-operator variability. As a surrogate measure, non-invasive techniques such as hepatic ultrasound elastography (measuring liver stiffness) have consistently demonstrated a good correlation with cirrhosis and portal hypertension.
![]() Transient elastography is a non-invasive technique with impressive accuracy for diagnosis of hepatic fibrosis (sensitivity of 91% and specificity of 75% with reference to liver biopsy ), and the severity of fibrosis detected correlates well with portal pressure.
Transient elastography is a non-invasive technique with impressive accuracy for diagnosis of hepatic fibrosis (sensitivity of 91% and specificity of 75% with reference to liver biopsy ), and the severity of fibrosis detected correlates well with portal pressure.
Cirrhosis can exist in a clinically silent, ‘compensated’ state for many years with an associated gradual increase in portal pressure. The development of clinical manifestations of acute decompensation occurs at a rate of up to 7% of patients per year and has a dramatic impact on overall median survival, from 12 years with compensated cirrhosis down to a median of 2 years.
As the portal pressure rises, shunting of blood through portosystemic venous collaterals returns up to 90% of portal blood flow back to the heart. Potentially troublesome collaterals develop at various watershed areas between the portal venous and systemic venous circulation. These areas include the oesophagus and cardia (between intrinsic and extrinsic gastro-oesophageal veins); the falciform ligament (through recanalised paraumbilical veins); and the anal canal (where the superior haemorrhoidal vein belonging to the portal system anastomoses with the middle and inferior haemorrhoidal veins which belong to the caval system).
Of relevance to the surgeon, bleeding from gastro-oesophageal varices can be torrential and constitutes the leading cause of death in patients with cirrhosis. Periumbilical collaterals of enlarged veins in the falciform ligament (‘caput medusae’) may bleed during abdominal surgery. Stomal and parastomal varices can develop secondary to venous communications between the surgically relocated mesenteric veins of the bowel and the cutaneous veins that drain into the inferior epigastric veins. Finally, anorectal varices can be identified during the course of lower gastrointestinal investigations and although they rarely cause bleeding, can be life-threatening in severe cases. At the time of diagnosis, varices are detected in 30% of patients with compensated cirrhosis, rising to 60% of patients presenting with decompensation and are associated with a corresponding risk of bleeding of 10–30% within 12 months. Without treatment, up to 90% of patients with cirrhosis go on to develop varices and endoscopic surveillance from the time of diagnosis is therefore mandated by current guidelines. .
![]() Upon diagnosis of cirrhosis, endoscopic surveillance for gastro-oesophageal varices is recommended as a mandatory component of clinical care (EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis, 2018).
Upon diagnosis of cirrhosis, endoscopic surveillance for gastro-oesophageal varices is recommended as a mandatory component of clinical care (EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis, 2018).
The pathophysiology of portal hypertension is multifactorial: intrahepatic fibrosis leads to an increase in vascular resistance whilst metabolic changes lead to a hyperdynamic circulation with an increase in splanchnic blood flow in particular. Non-selective beta-blockers (NSBBs, e.g. propranolol) reduce the portal pressure via vasoconstriction of the splanchnic blood supply.
![]() NSBBs are generally well tolerated in patients with established cirrhosis, and several clinical trials have demonstrated a clear survival advantage.
NSBBs are generally well tolerated in patients with established cirrhosis, and several clinical trials have demonstrated a clear survival advantage.
However, the systemic arterial blood pressure is also lowered and caution is therefore required in patients with cardiac failure or large volume ascites for whom development or exacerbation of hepato-renal syndrome can be a life-threatening adverse effect. Expert opinion is divided on the overall benefit of NSBBs in advanced cirrhosis with refractory ascites: there are some reports of poor survival rates, whilst recent retrospective analyses demonstrate a higher mortality in patients who discontinued NSBBs. This observation has been attributed to possible non-haemodynamic effects of NSBBs including a reduction in intestinal permeability and bacterial translocation.
![]() The sixth international consensus meeting for stratifying risk and individualising care for portal hypertension in Baveno, Italy, recommended close monitoring in patients with refractory ascites and dose reduction or discontinuation of NSBBs only for those patients who develop hypotension (SBP < 90 mmHg), hyponatraemia or impaired renal function.
The sixth international consensus meeting for stratifying risk and individualising care for portal hypertension in Baveno, Italy, recommended close monitoring in patients with refractory ascites and dose reduction or discontinuation of NSBBs only for those patients who develop hypotension (SBP < 90 mmHg), hyponatraemia or impaired renal function.
For those patients who develop hypotension (SBP < 90 mmHg), hyponatraemia or impaired renal function, substitution of NSBBs with EBL of varices or TIPSS (discussed further below) is recommended for primary and secondary prevention of variceal bleeding, respectively.
A further challenge with pharmacological therapy is variability in response to treatment: mortality is considerably reduced when a 20% reduction in portal pressure is achieved, but unfortunately up to 50% of patients do not respond to NSBB therapy. Carvedilol is an NSBB that also acts as an alpha-1 receptor blocker, thereby vasodilating the intrahepatic vasculature and reducing the portal pressure further. , This additional mechanism is haemodynamically significant: one small randomised controlled trial (RCT) demonstrated an effective therapeutic reduction in portal pressure (HVPG) in 64% patients treated with carvedilol versus only 14% receiving standard therapy with propranolol. Despite this, a recent Cochrane review of 10 RCTs failed to demonstrate a significant reduction in mortality or serious complications of cirrhosis with the use of carvedilol over traditional NSBBs, advising that further RCTs with longer-term follow-up are required to conclusively assess clinical outcomes.
In the context of acute variceal haemorrhage, vasopressin analogues can be used to achieve a rapid reduction in splanchnic blood flow (and thereby portal pressure) without the hazard of reducing the cardiac output associated with beta-blockade. Vasopressin does however carry a significant adverse-effect profile including hypertension and arrhythmia, such that it requires invasive monitoring and a continuous infusion. Terlipressin is a synthetic analogue of vasopressin with a more specific mechanism of action (V1 receptor) that allows it to be administered in bolus doses.
![]() A Cochrane review of seven studies comparing terlipressin with placebo (443 patients) demonstrated a 34% relative risk reduction in mortality and recommended terlipressin as the vasoactive drug of choice in acute variceal bleeding.
A Cochrane review of seven studies comparing terlipressin with placebo (443 patients) demonstrated a 34% relative risk reduction in mortality and recommended terlipressin as the vasoactive drug of choice in acute variceal bleeding.
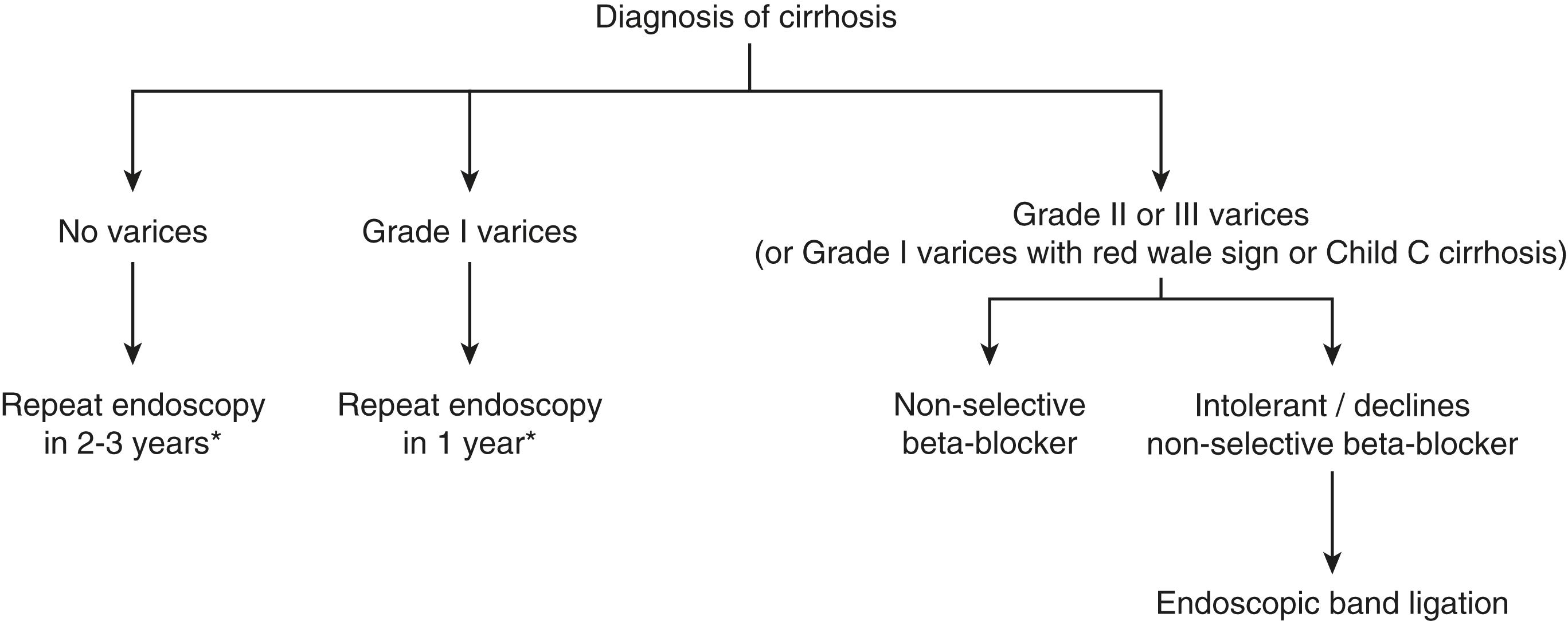
EBL of varices is effective for controlling haemorrhage in the acute setting and electively for the eradication of varices as either primary or secondary prevention (i.e. after a variceal bleed). However, endoscopic banding only treats the variceal manifestation of portal hypertension at a single site, without altering the underlying pathophysiology or portal pressure. EBL also requires endoscopic follow-up and presents a small risk of potentially life-threatening complications. It is therefore unsurprising that combination therapy with beta-blockers is associated with lower overall mortality than endoscopic banding alone, and treatment with NSBBs is generally preferred for primary prevention of variceal haemorrhage in the absence of individual patient contraindications. A summary algorithm for the recommended approach for primary prevention of variceal bleeding in patients with cirrhosis is shown in Fig. 9.1 .
It is becoming increasing clear that an underlying systemic inflammatory process (likely arising from abnormal bacterial translocation from the gut) may underpin the cardinal haemodynamic changes seen in cirrhosis. Indeed, recent evidence suggests that statins may have an important additional role to play in lowering intrahepatic vascular resistance, contributing to a reduction in decompensation events and overall mortality. As cirrhosis progresses and portal venous flow decreases, the risk of portal vein thrombosis steadily increases. This results in a sudden spike in portal pressure and decline in liver function as well as considerably adding to the operative risks of liver transplantation. Indeed, there is some evidence to suggest that anticoagulation in early cirrhosis is a safe and effective strategy for improving overall survival by reducing both the risk of portal vein thrombosis and the occurrence of episodes of decompensation overall.
Development of ascites is often the first manifestation of decompensation (and accounts for approximately 80% of all causes of ascites in the Western world). An effective reduction of the circulating systemic blood volume secondary to splanchnic vasodilatation plays a key role in this process. Other features of portal hypertension are almost universally present at this stage of the disease process, but diagnostic paracentesis should always be performed at the time of first presentation to confirm the diagnosis and exclude spontaneous bacterial peritonitis. The development of ascites marks a dramatic change in prognosis, with an overall predicted 1-year survival of 40%; in the absence of contraindications, referral for liver transplantation should be considered at this stage.
TIPSS ( Fig. 9.2 ) is a procedure undertaken by interventional radiology whereby a stent is placed via the jugular vein, through a hepatic vein and into an intrahepatic portal vein branch, allowing the portal circulation to decompress directly into the systemic venous return to the heart. The effectiveness and comparatively low complication rate of this procedure has essentially rendered the (elegant but hazardous) repertoire of surgical portosystemic venous shunts for treating portal hypertension obsolete.
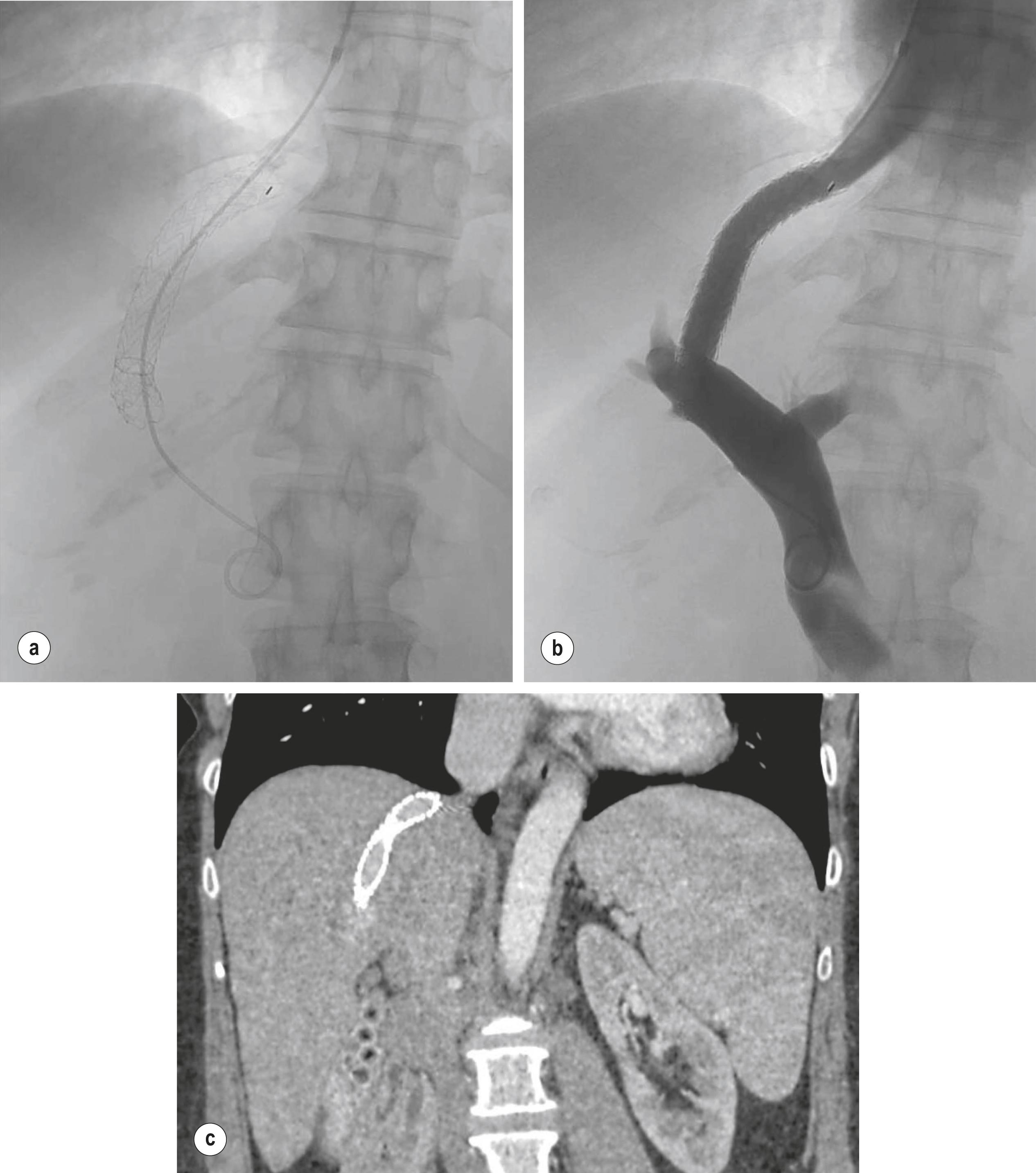
TIPSS can be employed in the elective setting for treating complications of portal hypertension including refractory ascites, hepatic hydrothorax and portal hypertensive gastropathy (PHG) after failure of medical therapy. It is also a very effective rescue therapy for treating active variceal bleeding when effective haemostasis cannot be achieved endoscopically (successful in 95% of cases with a re-bleeding rate of 18%). Up to 90% of the portal blood flow can be diverted to the systemic circulation with TIPSS. This augments the venous return to the heart and can provide a substantial benefit to patients with perilous haemodynamic instability and renal function, such as those requiring recurrent large-volume paracentesis (LVP) for refractory ascites. However, shunting portal venous blood directly into the systemic circulation without any hepatic metabolism also underpins the foremost complication of TIPSS—the onset or exacerbation of encephalopathy (risk factors include age > 65 years, Child–Pugh score > 12 and previous history of encephalopathy). The incidence of post-TIPSS encephalopathy has been reported as high as 50%, but this rate has reduced considerably after the introduction of PTFE-covered metal stents and stents that can be dilated to variable diameters as required (e.g. 8–10 mm depending on indication and pressure gradient). Additional procedural complications of TIPSS include intraperitoneal bleeding, biliary puncture, hepatic ischaemia and exacerbation of heart failure.
With regard to overall (transplant-free) survival, multiple meta-analyses of the six RCTs that compared TIPSS with recurrent LVP have provided conflicting results with no overall consensus. However, the rate of complications from the covered stents in current standard clinical practice is dramatically lower (including the rate of stent thrombosis, leading to longer patency rates). Encouragingly, a recent RCT comparing covered stent TIPSS with LVP for recurrent ascites reported improved 1-year survival with TIPSS and no evidence of an increase in the rate of encephalopathy. However, favourable outcomes remain confined to carefully selected patient groups.
The presence of varices increases progressively with the severity of cirrhosis (e.g. as classified by the Child–Pugh Classification, Table 9.1 ) from 42% of patients with Child’s A cirrhosis, up to 72% of patients with Child’s B or C cirrhosis. Untreated, variceal bleeding is the second most common manifestation of decompensation (after ascites) and presents an immediate threat to life with an overall mortality rate of up to 25% at 6 weeks.
| Clinical/lab value | Points assigned | ||
|---|---|---|---|
| 1 | 2 | 3 | |
| Bilirubin (mmol/L) | < 34 | 34–50 | > 50 |
| Albumin (g/L) | > 35 | 28–35 | < 28 |
| Prothrombin time (seconds prolonged) | < 4 | 4–6 | > 6 |
| Encephalopathy | None | Mild | Marked |
| Ascites | None | Mild | Marked |
Balloon tamponade can be an effective temporising measure for uncontrolled massive haemorrhage from oesophago-gastric varices, until definitive treatment (either TIPSS or surgery) is available. A recent series reported effective haemostasis with oral-gastric tube placement in 79% of patients. The Sengstaken–Blakemore tube (three-lumen tube) is the most commonly encountered oral-gastric tubes in clinical practice. Intubation and airway protection should be considered early in the management of any massive gastrointestinal haemorrhage but it is mandatory prior to oral-gastric tube insertion. Blind insertion of the tube is challenging (even with the assistance of a laryngoscope) and carries an inherent risk of fatal oesophageal rupture if the tube coils in the oesophagus prior to inflation of the gastric balloon. This can be largely prevented by railroading the tube over an endoscopically placed stiff guidewire (e.g. Amplatz®), although time and available resources do not always permit this approach.
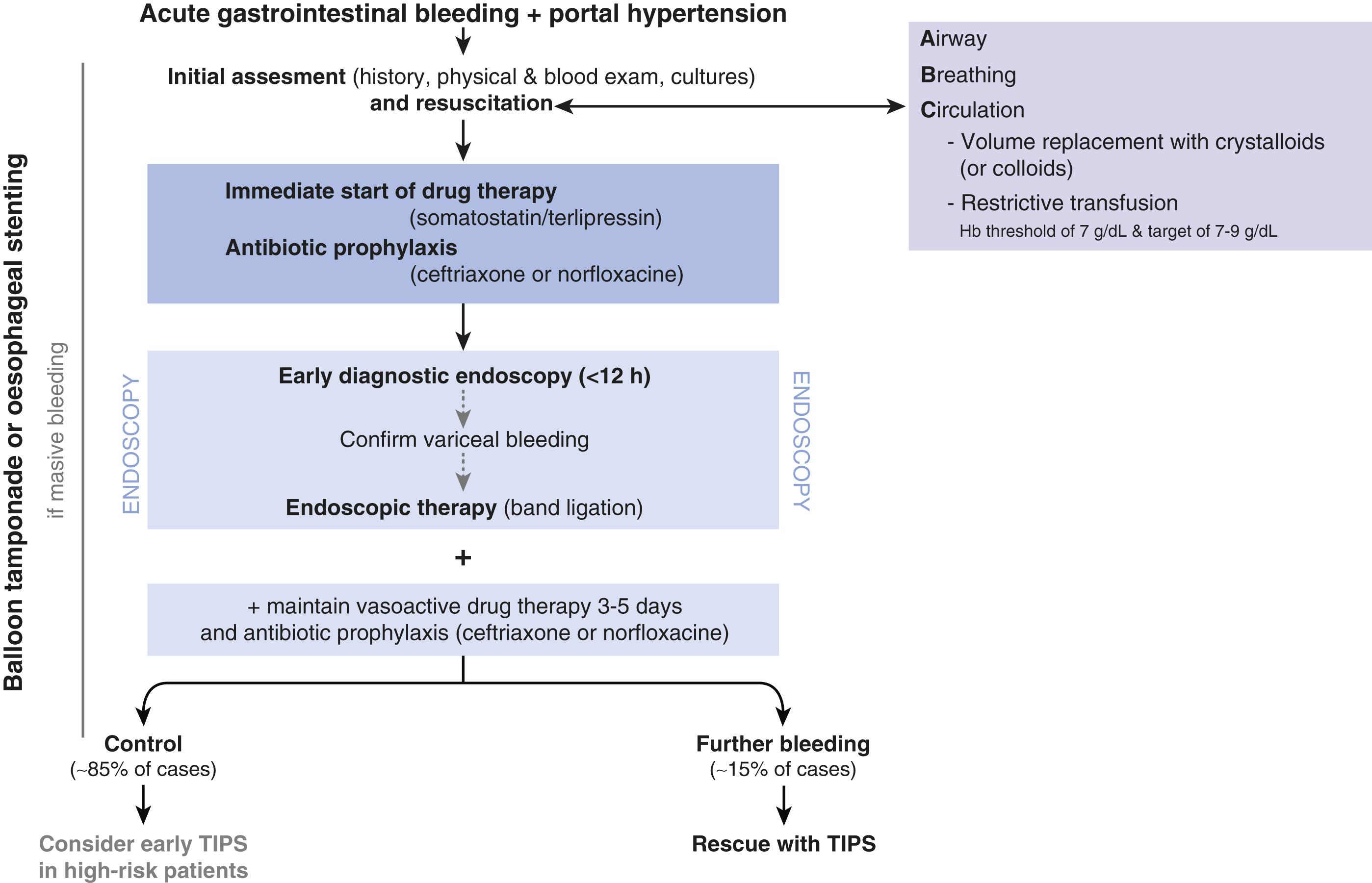
The gastric balloon is inflated in the stomach (e.g. with 30 mL of water) and placed on gentle traction against the gastro-oesophageal junction. Even for oesophageal varices, inflation of gastric balloon alone achieves haemostasis in the majority of cases; inflation of the oesophageal balloon should be delayed and only undertaken if bleeding persists as there is an increased risk of necrosis at the gastro-oesophageal junction. The oesophageal balloon must be deflated every 12 hours to prevent necrosis, and for similar reasons the gastric balloon should not be inflated for more than 48 hours. Upon deflation of the balloons, re-bleeding occurs in 50% of patients with oesophago-gastric varices and re-bleeding is the rule for gastric varices unless more definitive control of bleeding is established. Placement of an oro-gastric balloon is a high-risk intervention that requires appropriate expertise and timely availability of definitive treatment options. When endoscopy is immediately available, placement of (removable) covered self-expanding metal oesophageal stent appears to be an attractive novel alternative, with a recent RCT reporting superior haemostasis (85% vs 47%) with fewer serious adverse events (15% vs 47%). A systematic approach to the management of acute variceal bleeding is summarised in Fig. 9.3 .
PHG is an abnormality of the gastric mucosa characterised endoscopically by a mosaic-like pattern resembling ‘snake skin’, with or without red spots. The overall prevalence of PHG in cirrhosis is roughly 80% and it is strongly correlated with the severity of cirrhosis. The same pathology can arise in other areas of the GI tract, albeit less commonly (portal hypertensive colopathy or intestinopathy). Clinically, the primary relevance of PHG is as a source of persistent occult bleeding leading to iron-deficiency anaemia; significant acute haemorrhage is rare. No effective endoscopic therapeutic options exist, so treatment revolves around lowering the portal pressure in the same way as for variceal bleeding (pharmacologically or with TIPSS), with consideration of liver transplantation if appropriate.
Segmental portal hypertension resulting from splenic vein thrombosis should always be considered as the potential cause of bleeding gastric varices in patients with pancreatic pathology. Gastric varices have a variable appearance and are often covered with normal mucosa; caution (and/or endoscopic ultrasound assessment) is required before undertaking biopsy of any lesion of the gastric fundus or cardia, particularly in a patient with a history of pancreatic pathology. Patients with chronic pancreatitis who develop variceal bleeding as a result of thrombosis of the splenic vein should be considered for splenectomy (or splenic vein embolisation), which is often curative.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here