Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Platelets are highly complex cells that participate in critical steps central to hemostasis and thrombosis, including adhesion to subendothelium, aggregation, secretion of granule contents, and provision of membrane surface for activation of coagulation factors.
Abnormalities of either platelet number or platelet function can play an important role in the balance of hemostasis and thrombosis.
Almost unique to laboratory medicine and pathology, assessment of platelet pathology may be performed in real time on living cells obtained from the patient.
A number of inherited and acquired disorders, autoimmune processes, and drugs affect platelet counts and platelet function.
In a large proportion of patients with inherited platelet disorders, the underlying genetic and molecular mechanisms are unknown.
Von Willebrand factor (vWF) is a multimeric protein synthesized by endothelial cells and megakaryocytes that plays a central role in platelet adhesive interactions.
Abnormalities related to vWF lead to the bleeding disorder von Willebrand disease and thrombotic thrombocytopenic purpura, associated with vascular occlusions and hemolysis.
The authors thank Dr. Jonathan Miller for his contributions as an author of this chapter in the prior editions of this textbook.
Blood platelets are highly complex, anucleate cells that derive from bone marrow megakaryocytes. Peripheral blood film offers the opportunity for evaluation of platelet numbers, size, distribution, and structure under the light microscope.
Electron microscopy allows more precise characterization of the structural abnormalities ( ), with the opportunity to examine in greater detail specific platelet organelles ( ). An array of 3-dimensional high-resolution structural approaches have emerged and provide novel insights into platelets ( ).
Platelet features that may be visualized ultrastructurally are shown in Figure 41.1 . The outer surface of the platelet, the glycocalyx , is rich in glycoproteins. A submembranous band of microtubules , composed of the protein tubulin, provides structural support for the discoid platelet shape. Contractile microfilaments composed of actin and myosin may also be seen. An extensive open canalicular system within the platelet is in direct communication with the extracellular environment. Often seen in proximity to the open canalicular system is the dense tubular system . The dense tubular system also functions as a calcium-sequestering pump, maintaining low levels of cytoplasmic calcium in the resting platelet.
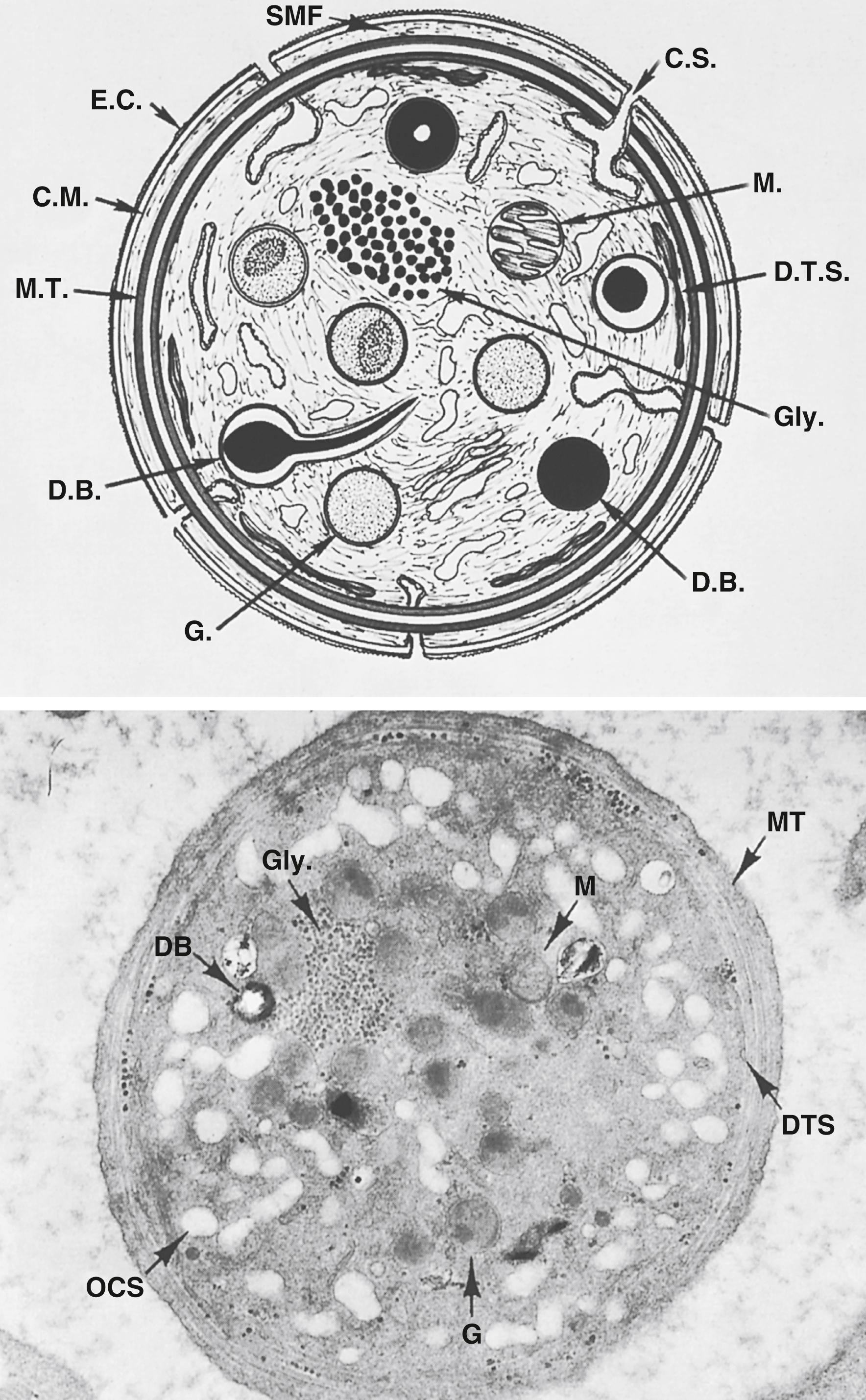
A variety of inclusions are recognized within the platelet cytoplasm, including mitochondria , glycogen , and granules . Lighter staining α-granules, less frequent dense core (or “bull’s-eye”) granules, lysosomes, and peroxisomes are also seen. Three-dimensional electron microscopic studies have revealed morphologically distinct α-granule subtypes and demonstrated that high spatial segregation of different stored proteins exists within individual α-granules ( ). The α-granule proteins derive both from endocytic uptake and de novo synthesis by megakaryocytes, and include fibrinogen, platelet-derived growth factor (PDGF), von Willebrand factor (vWF), the factor V binding protein multimerin, β-thromboglobulin (βTG), and the heparin-neutralizing platelet factor (PF) 4. P-selectin, a constituent of the α-granule membrane, translocates to the plasma membrane of the platelet when α-granule contents are released. The dense granules contain a nonmetabolic pool of adenosine diphosphate (ADP) and adenosine triphosphate (ATP), 5-hydroxytryptamine (5-HT, serotonin), calcium, and inorganic polyphosphate (polyP).
Historically, analyses of platelet surface glycoproteins in patients with inherited platelet disorders have been key to our current understanding of fundamental aspects of platelet function. Table 41.1 shows the major platelet membrane glycoproteins that function as receptors for adhesive ligands. The GPIIb-IIIa receptor complex (also referred to as integrin αIIbβ3 ), which in its activated form serves as a receptor for fibrinogen, is the most abundant platelet receptor, with ∼80,000 to 100,000 copies per platelet. This is followed by the major platelet receptor for vWF, GPIbα, at ∼30,000 copies. GPIbα is disulfide linked to GPIbβ and noncovalently linked to GPIX and GPV; together, these glycoproteins make up the GPIb-IX-V complex. The copy number for other platelet surface glycoproteins is lower. GPVI and GPIa-IIa mediate platelet interactions with collagen.
| Alternate Designation(s) | Structural Family | Principal Ligand(s) | Major Function | |
|---|---|---|---|---|
| GPIIb-IIIa | CD41-CD61, α IIb β 3 , | Integrin | Fibrinogen, von Willebrand factor (vWF) | Aggregation (platelet-platelet interaction) |
| GPIb-IX-V | CD42a-d complex | Leucine-rich glycoprotein | vWF, thrombin, P-selectin, coagulation contact factors | Adhesion (platelet-subendothelium interaction) |
| GPVI | Immunoglobulin receptor superfamily | Collagen | Signaling following platelet-collagen interaction | |
| GPIa-IIa | CD49b-CD29, α 2 β 1 | Integrin | Collagen | Adhesion (platelet-collagen interaction) |
| P-selectin | CD62P, GMP 140, PADGEM | Selectin | P-selectin–glycoprotein ligand-1 (PSGL-1) | Platelet-leukocyte interaction |
| PECAM-1 | CD31 | Immunoglobulin receptor superfamily | PECAM-1/PECAM-1 homophilic interactions | Platelet-endothelial cell interaction |
| GPIV | CD36, GPIIIb | Scavenger receptor family | Thrombospondin, collagen, oxidized low-density lipoproteins | Scavenger, adhesion |
Platelet membranes contain several phospholipids that play a major role in platelet function, including phosphatidylinositol, phosphatidylcholine, phosphatidylserine (PS), and phosphatidylethanolamine. Phosphatidylinositides are the source of signaling molecules inositoltrisphosphate and diacylglycerol, which are produced following platelet activation. Negatively charged PS is expressed in the inner membrane leaflet of the resting platelet; on platelet activation, PS translocates to the outer leaflet, an essential step in the formation of a procoagulant platelet surface that is critical in several blood coagulation mechanisms.
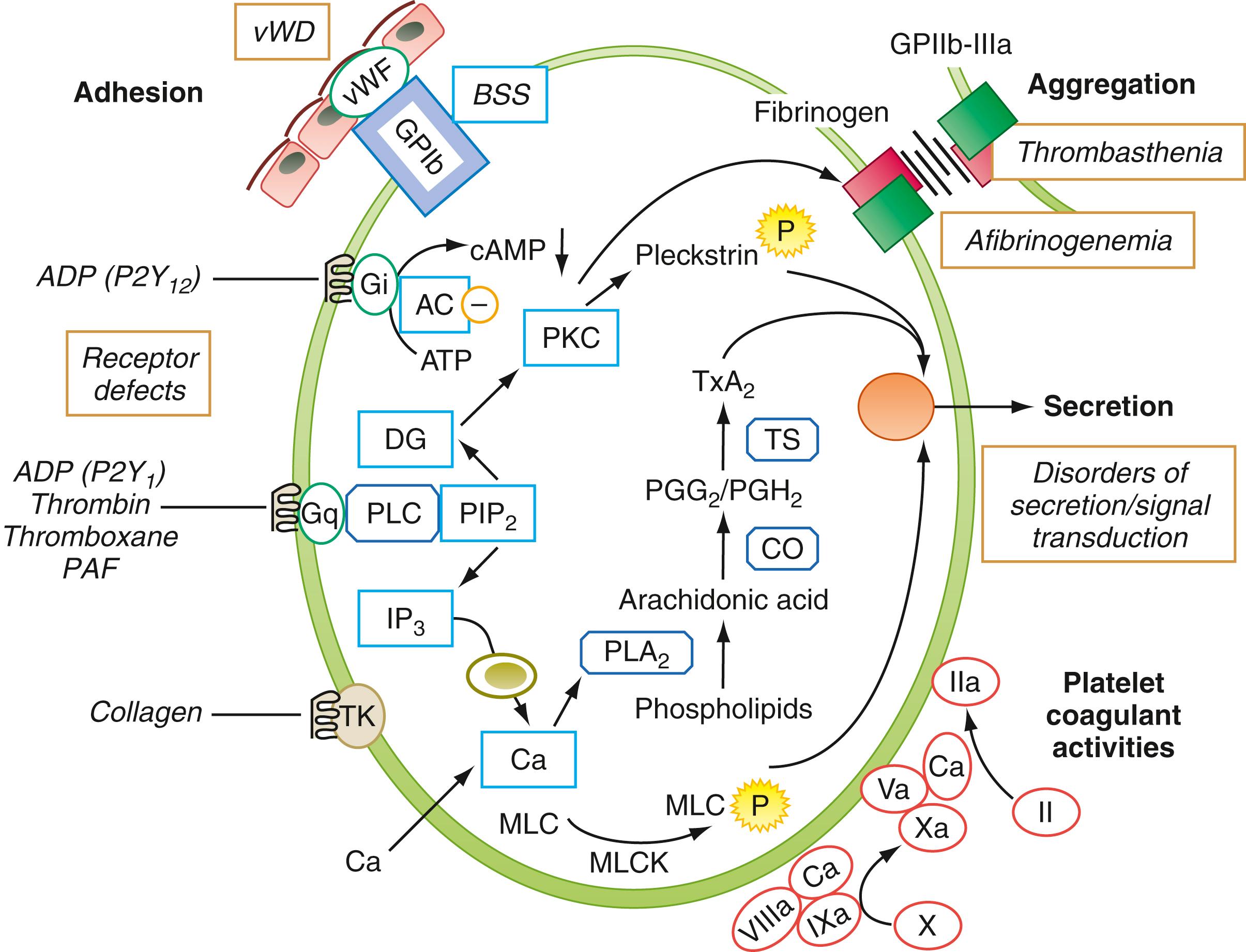
Following injury to the blood vessel, platelets adhere to exposed subendothelium by a process ( adhesion ) that involves the interaction of a plasma protein, vWF, and a specific glycoprotein complex on the platelet surface, GPIb-IX-V ( Fig. 41.2 ), which binds vWF particularly under conditions of high shear stress. Adhesion is followed by recruitment of additional platelets, which interact with each other to form clumps, a process called aggregation . This involves binding of fibrinogen to specific platelet surface receptors—a complex composed of GPIIb-IIIa, which is platelet- and megakaryocyte-specific and binds vWF as well. Resting platelets do not bind fibrinogen. Stimulation of platelets leads to a series of intracellular signaling responses, including binding of the adapter proteins talin and kindlin to the cytoplasmic tails of the GPIIb-IIIa receptor complexes ( ). These events produce conformational changes in the GPIIb-IIIa complex that expose binding sites for fibrinogen, a prerequisite for platelet aggregation. Activated platelets release contents of their granules ( secretion or release reaction ), such as ADP and serotonin from the dense granules, which cause recruitment of additional platelets. In addition, platelets play a major role in coagulation mechanisms; several key enzymatic reactions occur on the platelet membrane lipoprotein surface ( platelet coagulant activity ).
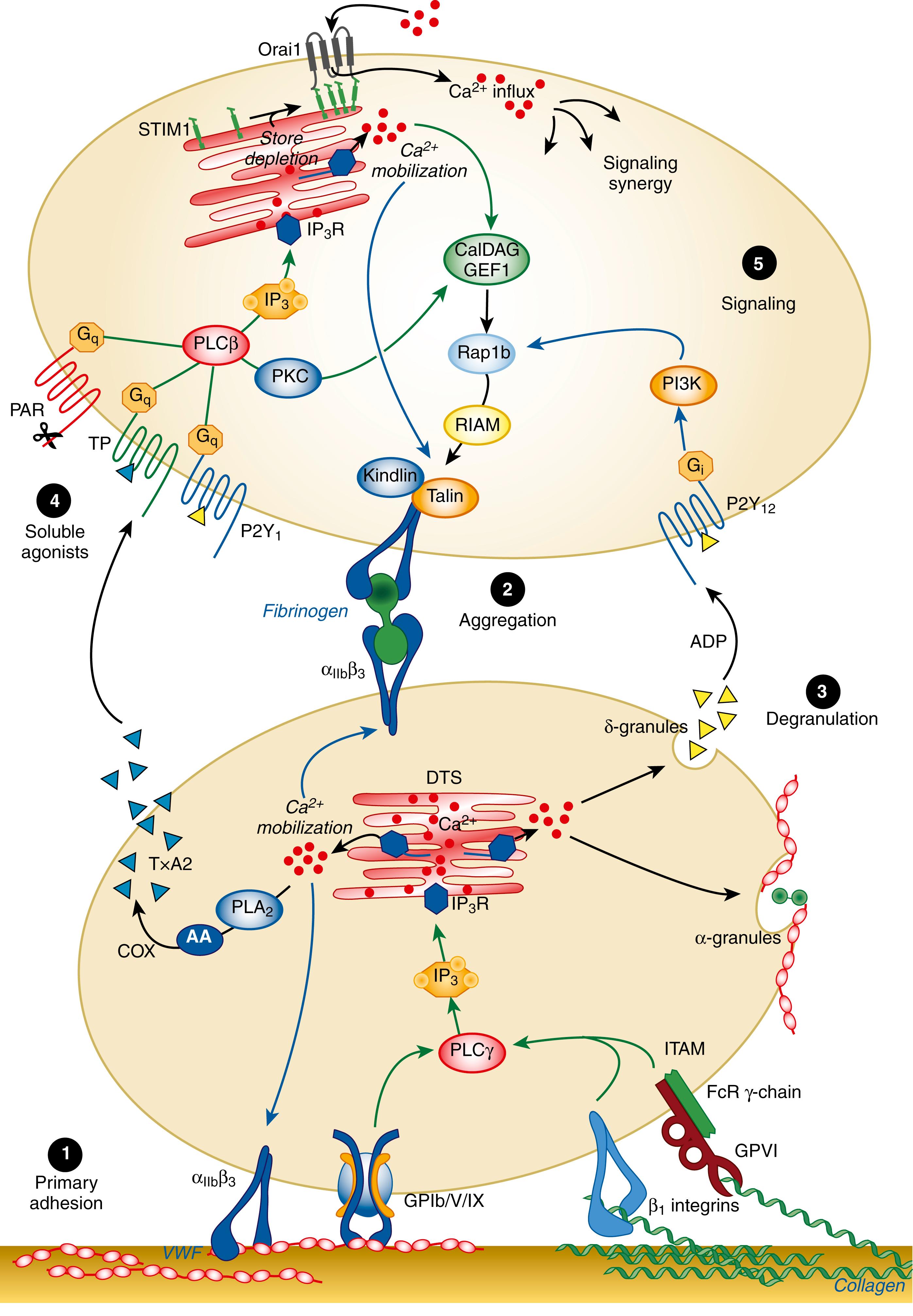
Several physiologic agonists interact with specific receptors on the platelet surface to induce events that culminate in well-recognized responses, including a change in platelet shape from discoid to spherical (shape change), aggregation, secretion, and thromboxane A2 (TXA2) production ( ; ). These agonists include ADP, collagen, thrombin, TXA2, epinephrine, and platelet-activating factor (PAF), and they induce signaling events in platelets. Platelets possess at least three well-defined purinergic receptors that mediate the responses to ADP: P2Y1, P2Y12, and P2X1 (not shown). The P2Y1 receptor mediates the rise in cytoplasmic Ca 2+ ; the P2Y12 receptor mediates inhibition of adenylyl cyclase to lower cyclic adenosine monophosphate (cAMP) levels in platelets and is the receptor targeted by antiplatelet agents, such as clopidogrel and prasugrel. P2X1 functions as an ion channel to amplify the platelet activation process. Thrombin induces platelet responses through the protease-activated receptors (PARs); human platelets possess PAR1 and PAR4 receptors. GPVI is the principal collagen receptor in platelets and is a member of the immunoglobulin (Ig) receptor superfamily. Ligation of the platelet receptors by agonists such as thrombin, TXA2, and ADP initiates the production of several intracellular messenger molecules, including products of hydrolysis of phosphoinositides (PI) by phospholipase C (diacylglycerol, and inositol 1,4,5-triphosphate [IP3]) and conversion of arachidonic acid to TXA2. These mediators induce or modulate the various platelet responses of Ca 2+ mobilization, protein phosphorylation, aggregation, secretion, and thromboxane production. The interaction between the platelet surface receptors and the key intracellular enzymes (e.g., phospholipases A2 and C, adenylyl cyclase [not shown]) is mediated by a group of distinct proteins called G-proteins that bind and are modulated by GTP. These include rap1A and rap1b (or RIAM) proteins, shown in Fig. 41.2. As in most secretory cells, platelet activation results in a rise in cytoplasmic ionized calcium concentration; IP3 functions as a messenger to mobilize Ca 2+ from intracellular stores. This increase in cytoplasmic Ca 2+ levels regulates other events, such as the activation of phospholipase A2, leading to TXA2 production, and phosphorylation by myosin light-chain kinase of myosin light chain, which is involved in shape change and secretion. Diacylglycerol (DAG) activates the protein kinase C (PKC) family of enzymes that phosphorylate several proteins, including pleckstrin. PKC activation is considered to play a major role in platelet responses, including secretion and the activation of GPIIb-IIIa. Platelets possess several families of G-proteins that function as molecular switches in transmitting the signal from the surface receptors to the intracellular effectors. For example, phospholipase C (PLC) activation and calcium mobilization on activation by ADP (P2Y1), TXA2, or thrombin is mediated by Gαq, whereas signaling through the P2Y12 ADP receptor and inhibition of adenylyl cyclase is mediated by Gαi. Another well-recognized response of platelets to activation is synthesis of TXA2. The initial and rate-limiting step in TXA2 production is the mobilization of arachidonic acid (AA) from phospholipids (predominantly phosphatidylcholine) by phospholipase A2. Free AA is converted by cyclooxygenase to prostaglandins (PG) G2 and H2 (not shown), which are converted by thromboxane synthase to TXA2. Binding of fibrinogen to the GPIIb-IIIa complex results in the activation of tyrosine kinases and associated events (“outside-in signaling”) ( ). Numerous other mechanisms and events occur in platelets on activation involving small GTPases, tyrosine kinases, and phosphatases; these are beyond the scope of this chapter. While the agonists mentioned earlier activate platelets to function in hemostasis, there are other agonists—such as prostacyclin (PGI2), produced by endothelial cells—that inhibit platelet responses. PGI2 does this by increasing platelet cAMP levels through activation of adenylyl cyclase.
Platelets play a vital role in coagulation. Numerous proteins, including coagulation factor V and fibrinogen, are released from α-granules. ADP, ATP, serotonin, and the pro-hemostatic polyphosphates ( ) are released from dense granules. Importantly, several of the key enzymatic reactions leading to factor X and prothrombin activation, and to thrombin generation, require the platelet membrane surface to proceed at an optimum rate ( ). Platelet activation results in movement or “flip-flop” of PS and other phospholipids from the internal to the external surface of the membrane ( ). This is essential to the role of platelets in blood coagulation mechanisms.
The diagnostic process begins with a detailed clinical evaluation followed by laboratory studies ( ; ). Platelet disorders may occur in association with other inherited or acquired disorders or syndromes; thus, a detailed clinical evaluation is essential. To better assess the intensity of bleeding symptoms, a number of validated standardized bleeding assessment tools are available ( ). This evaluation should also include an assessment of ingestion of medications, herbal supplements, and over-the-counter substances. Many such compounds affect platelet number or function.
The initial laboratory evaluation of platelet disorders includes a complete blood count, including the platelet count. The normal platelet count is 150 to 400 × 10 9 /L. In severe thrombocytopenia, below the established linearity of a given automated instrument or in the presence of cellular fragments spuriously affecting the automated count, a manual phase contrast count with a hemocytometer chamber may be required. Many instruments also provide the mean platelet volume (MPV) and a histogram of MPV. Some automated instruments also assess platelet maturity, as reflected by the RNA content of “reticulated platelets”—analogous to reticulocyte measurements in the erythroid series ( ; ). Such measurements offer the opportunity to detect a thrombopoietic response from the bone marrow. Evaluation of the peripheral blood film provides valuable information regarding platelet count and size distribution, and on associated changes in other blood cells. A simple diagnostic approach that utilizes immunofluorescence labeling of peripheral blood smears using antibodies specific for proteins known to be affected has been proposed as a diagnostic tool for several inherited platelet disorders ( ).
No currently available laboratory test faithfully reflects the enormously complex platelet role in hemostasis. Several instruments and approaches have been developed to study platelet function ( ; ; ; ). A large number of biochemical and functional approaches, many in research laboratories, have been applied as a part of phenotype-driven and candidate gene approaches in unraveling the underlying mechanisms in patients identified ( ). These approaches have taken a major change in direction with the recent application of high-throughput deoxyribonucleic acid (DNA) sequencing methods to define the genetic basis in patients ( ; ; ; ).
For many years, the template bleeding time test was used as a “global” test for the adequacy of primary hemostasis. In such testing, a standardized cut was made on the volar surface of the forearm and the duration it took for the bleeding to stop constituted the bleeding time. The bleeding time has a relatively poor predictive value of clinical bleeding ( ), carries risk for scarring, and requires considerable technical expertise and time. It has been largely abandoned in most centers.
In the platelet function analyzer (PFA-100 and PFA-200) ( ; ), anticoagulated whole blood is flowed under high shear force through a narrow hole punched out of a membrane coated with collagen and either epinephrine or ADP. The time to full occlusion of the channel is recorded as “closure time.” This is dependent on plasma vWF, platelet count and function, and hematocrit. Whereas inhibition of the platelet cyclooxygenase by aspirin or other mild to moderate impairments of platelet function prolong closure times with the collagen/epinephrine membranes, only more profound impairment of platelet function or of vWF prolong closure times in the collagen/ADP cartridges. Although abnormal in some platelet disorders, this instrument does not have sufficient sensitivity or specificity to be relied on as a screening tool for platelet disorders ( ). Definitive identification of abnormalities of platelets or vWF requires more specific studies.
Several additional ex vivo systems to assess platelet function have been developed in which shear forces play a major role. Notable among these is the development of the Impact-R instrument based on the cone and plate method for generation of shear ( ). Limitations of this method both in the diagnosis of bleeding disorders ( ) and in monitoring antiplatelet therapy ( ) have been described. Several other methods aiming to detect inherited and acquired disorders relating both to platelets and to vWF have been developed, but their role in clinical practice remains to be defined ( ).
Platelet function can be evaluated in vitro through study of platelet aggregation and secretion in response to a battery of platelet-stimulating agents ( ; ; ; ). These studies are generally performed using platelet-rich plasma (PRP) harvested from blood collected using sodium citrate as the anticoagulant. Ethylenediaminetetraacetic acid (EDTA), routinely used to collect samples for blood counts, dissociates the platelet GPIIb-IIIa complexes; thus, aggregation studies cannot be performed using such a sample. When citrated PRP is continuously stirred in a platelet aggregometer and a light beam is passed through the suspension; platelet aggregation in response to an added agonist can be monitored by changes in light transmittance. Change in platelet shape from discoid to spheroid is seen as an initial decrease in transmittance, whereas the subsequent formation of platelet clumps allows more light to pass through the suspension to the photodetector and is recorded as an increase in light transmittance ( ). Recommendations have been published from the International Society on Thrombosis and Haemostasis (ISTH) ( ) and others ( ) for the standardization of light-transmission aggregometry. In instruments equipped with a second channel for monitoring secretion, the release of ATP from platelet-dense granules is simultaneously measured ( Fig. 41.3 ). This is accomplished by adding the firefly luminescence substrate and enzyme, luciferin and luciferase, to the PRP. Released ATP then functions as a cofactor in the light-producing luciferin-luciferase reaction, and light emission is recorded with a second photodetector. Thus, aggregation and secretion can be monitored simultaneously and independently ( ). In most cases, the release of ATP may be assumed to reflect the release of the other dense granule constituents, which are less easily measured (i.e., ADP, serotonin, calcium, polyphosphates). Direct biochemical measurements of serotonin, ATP, and ADP can also be performed ( ). Platelet-dense granule secretion may be studied in parallel with aggregation by labeling platelets with 14 C-serotonin and then measuring the release of radioactivity following platelet activation ( ). On platelet activation, contents of the α-granules, dense granules, and the lysosomal granules are released. These can monitored by different methods ( ).
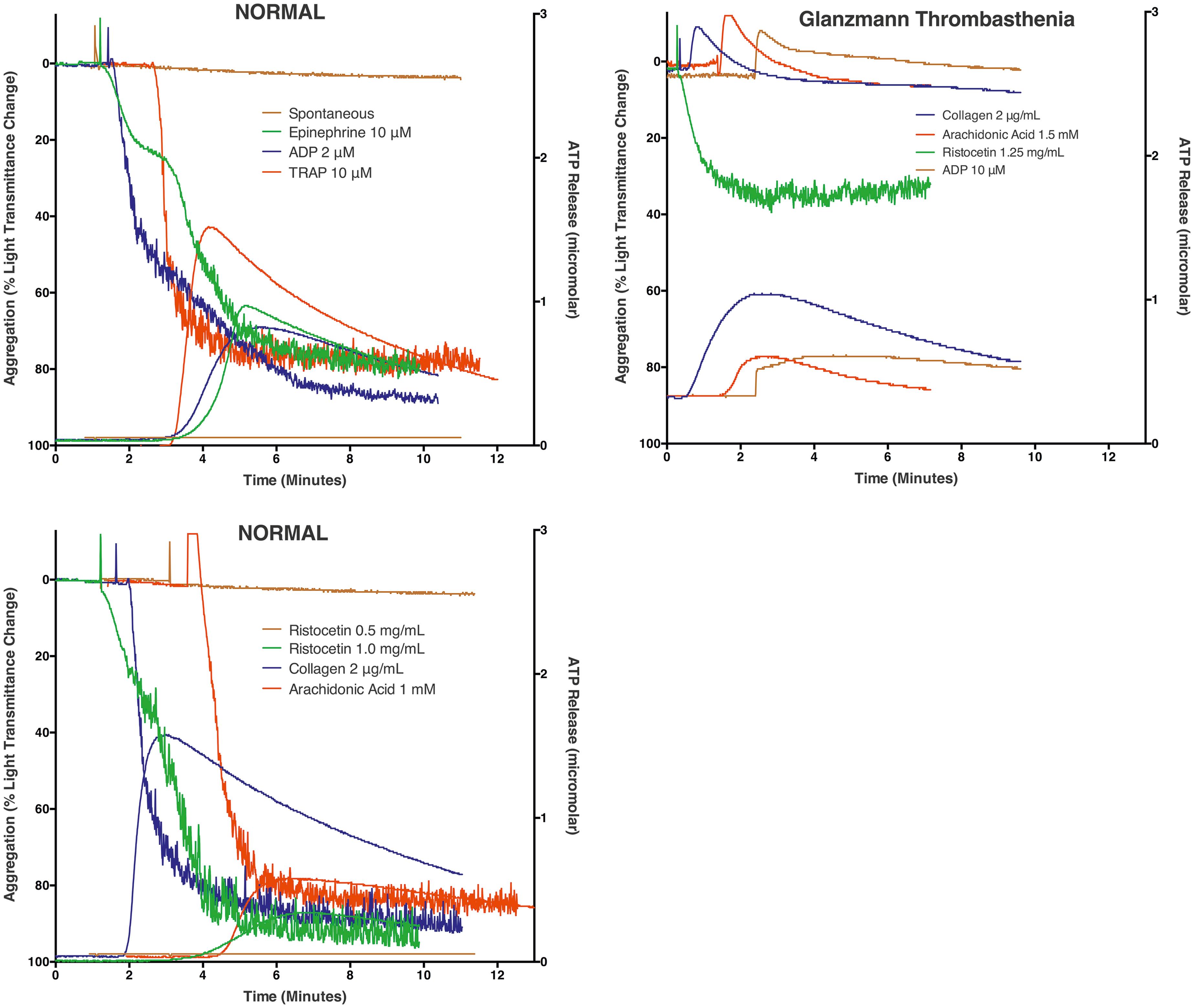
Platelets have surface receptors for several agonists (see Fig. 41.2 ). Frequently employed agonists in the laboratory include collagen, epinephrine, ADP, U46619 (a TXA2 analog), AA, ristocetin, PAR-1 agonist (SFLLRN), and the calcium ionophore A23187. Platelet responses to these stimuli, with the exception of ristocetin, are dependent on active metabolic processes. In contrast, ristocetin-induced clumping of platelets occurs to a large degree even in the presence of metabolic inhibitors and in formalin-fixed platelets; therefore, it is often referred as agglutination .
Although of paramount importance in vivo, thrombin is difficult to employ as an agonist with PRP because of interference from fibrin formation. The partially trypsinized γ-thrombin, however, retains platelet-stimulating activity but largely lacks clotting activity and can be useful. Thrombin cleaves the G-protein–coupled transmembrane platelet PAR1 receptor. Thus, thrombin receptor–activating peptide (TRAP), consisting of amino acid sequence SFLLRN, derived from the extracellular “tethered ligand” region of the thrombin receptor, activates platelets and is useful in platelet function testing. Strong agonists such as collagen and thrombin are capable of directly inducing secretion and TXA2 synthesis in addition to inducing aggregation. In contrast, secretion and TXA2 synthesis following platelet stimulation with weaker agonists such as ADP or epinephrine may be considered secondary responses following attainment of a threshold level of aggregation ( ). The potential diagnostic yields and limitations of aggregation and secretion studies in patients have been reviewed ( ; ).
Other methods have also been developed to test platelet function ( ). Electrical impedance measurements, as opposed to monitoring light transmission, have been used to study platelet aggregation not only in PRP but also in whole blood ( ). The resulting curves of electrical impedance over time share many similarities to those of light transmittance recordings, although there are characteristic differences between these two approaches ( ; ). When impedance aggregometry is combined with ATP secretion measurement on whole-blood samples ( ), relatively rapid evaluation of platelet function, requiring only a small volume of blood, may be performed ( ). Additionally, platelet aggregation in whole blood may be monitored optically by means of the coaggregation of fibrinogen-coated beads ( Verify Now ) impregnated with a dye that absorbs light in the infrared region of the electromagnetic spectrum ( ). This approach has been applied for assessing the effect of treatment with platelet inhibitors (GPIIb-IIIa inhibitors, aspirin, and clopidogrel).
The contractile abilities of activated platelets also result in contraction (or “retraction”) of formed clots. In the test tube, clot retraction may be quantitatively assessed. In thrombocytopenia or Glanzmann thrombasthenia, clot retraction is delayed or incomplete. GPIIb-IIIa ( ) as well as a number of additional platelet cytoskeletal and contractile proteins ( ) are required for effective clot retraction.
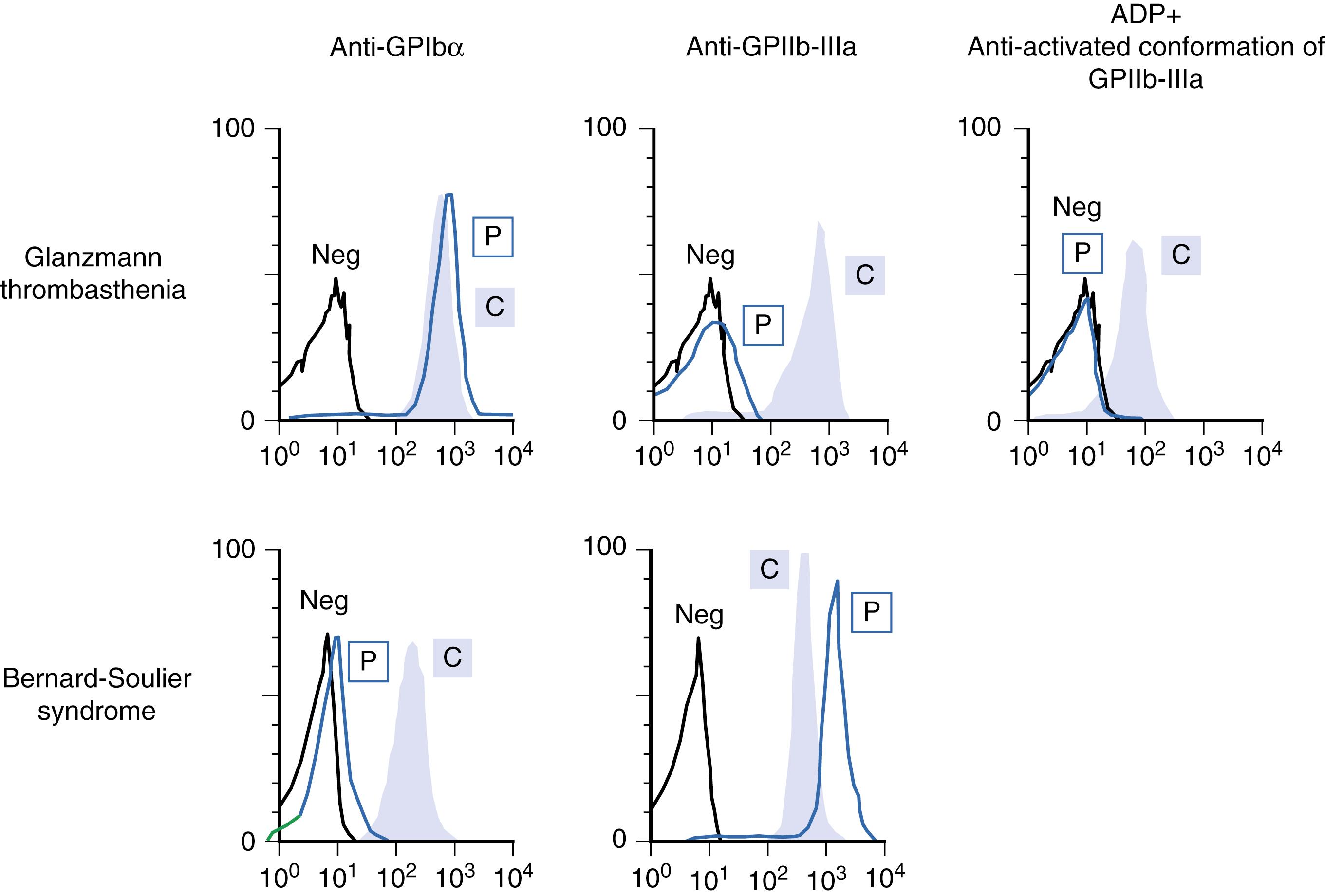
Flow cytometry has proved useful for assessing the expression of specific platelet surface glycoprotein receptors and for assessing platelet activation, including ability of GPIIb-IIIa to undergo conformational change, and expression of markers of platelet secretion (e.g., P-selectin from α-granules; Fig. 41.4 ) ( ). Flow cytometry has been used to assess platelet expression of annexin V, dense granules, and release of microparticles. Due to the small volumes of blood required, flow cytometry can be particularly valuable in diagnostic evaluations of children and neonates. Recently, mass cytometry using multiple metal conjugated antibodies has been applied to document heterogeneity of normal platelets in circulation and novel alterations in platelet glycoproteins in Glanzmann thrombasthenia ( ).
The advent of high-throughput DNA sequencing (HTS) is a major advance in the diagnostic approach to patients with inherited platelet disorders ( ; ; ; ). This has transformed the diagnostic landscape from a phenotype-based, laboratory-based, and candidate-gene approach to one that is genotype based. It has provided new insights into genotype-phenotype correlations, discovery of novel genes causing inherited platelet disorders, and the unraveling of unknown molecular pathways regulating megakaryocyte-platelet biology. The application of HTS to patients by different groups has been based on targeted gene panels and whole-exome sequencing (WES) ( ; ; ; ; , ), with whole-genome sequencing being tested. Overall, these approaches provide a genetic diagnosis in about 40% to 50% of patients with inherited platelet disorders, combining those with defects in platelet number and function ( ; ). However, in a large fraction of such patients, the genetic diagnosis remains elusive despite state-of-the art studies. They may have abnormalities in unknown genes or in noncoding regions of the genome. Moreover, a substantial number of variants detected in known genes remain as variants of unknown significance. The advantages of a genetic diagnosis are clear and include a predictive value beyond bleeding (such as predisposition to leukemia or renal failure). As of now, access to these HTS approaches and the required expertise is limiting.
Decreased platelet production and increased platelet destruction ( Table 41.2 ) constitute two of the major causes of thrombocytopenia. Additionally, thrombocytopenia may be seen with splenomegaly of any cause because of increased splenic sequestration of platelets.
| Type of Thrombocytopenia | Specific Example(s) |
|---|---|
| Immune Mediated | |
| Autoantibody-mediated platelet destruction by reticuloendothelial system (RES) | Primary immune thrombocytopenic purpura; secondary immune thrombocytopenia associated with lymphoproliferative disease; collagen vascular disease; infections such as infectious mononucleosis; human immunodeficiency virus syndrome |
| Alloantibody-mediated platelet destruction by RES | Neonatal alloimmune thrombocytopenia; posttransfusion purpura; passive alloimmune thrombocytopenia; alloimmune platelet transfusion refractoriness |
| Drug-dependent, antibody-mediated platelet destruction by RES | Drug-induced immune thrombocytopenic purpura (e.g., quinine) |
| Platelet activation by binding of immunoglobulin G (IgG) Fc of drug-dependent IgG to platelet FcγIIa receptors | Heparin-induced thrombocytopenia |
| Non–Immune Mediated | |
| Platelet activation by thrombin or proinflammatory cytokines | Disseminated intravascular coagulation; septicemia/systemic inflammatory response syndromes |
| Platelet destruction via ingestion by macrophages (hemophagocytosis) | Infections; certain malignant lymphoproliferative disorders |
| Platelet destruction through platelet interactions with altered von Willebrand factor | Thrombotic thrombocytopenic purpura; hemolytic-uremic syndrome; aortic stenosis |
| Platelet losses on artificial surfaces | Cardiopulmonary bypass surgery; use of intravascular catheters |
| Decreased platelet survival associated with cardiovascular disease | Inherited and acquired heart disease; cardiomyopathy; pulmonary embolism |
Inherited thrombocytopenias are being recognized with increasing frequency; several distinct genetic abnormalities have been documented in such patients ( ; , ; ; ; ) ( Fig. 41.5 ). These patients may present with isolated thrombocytopenia or in conjunction with characteristic syndromes. In some patients, the platelets have defects in function as well. These entities are discussed further in the section on Inherited Disorders of Platelet Function.
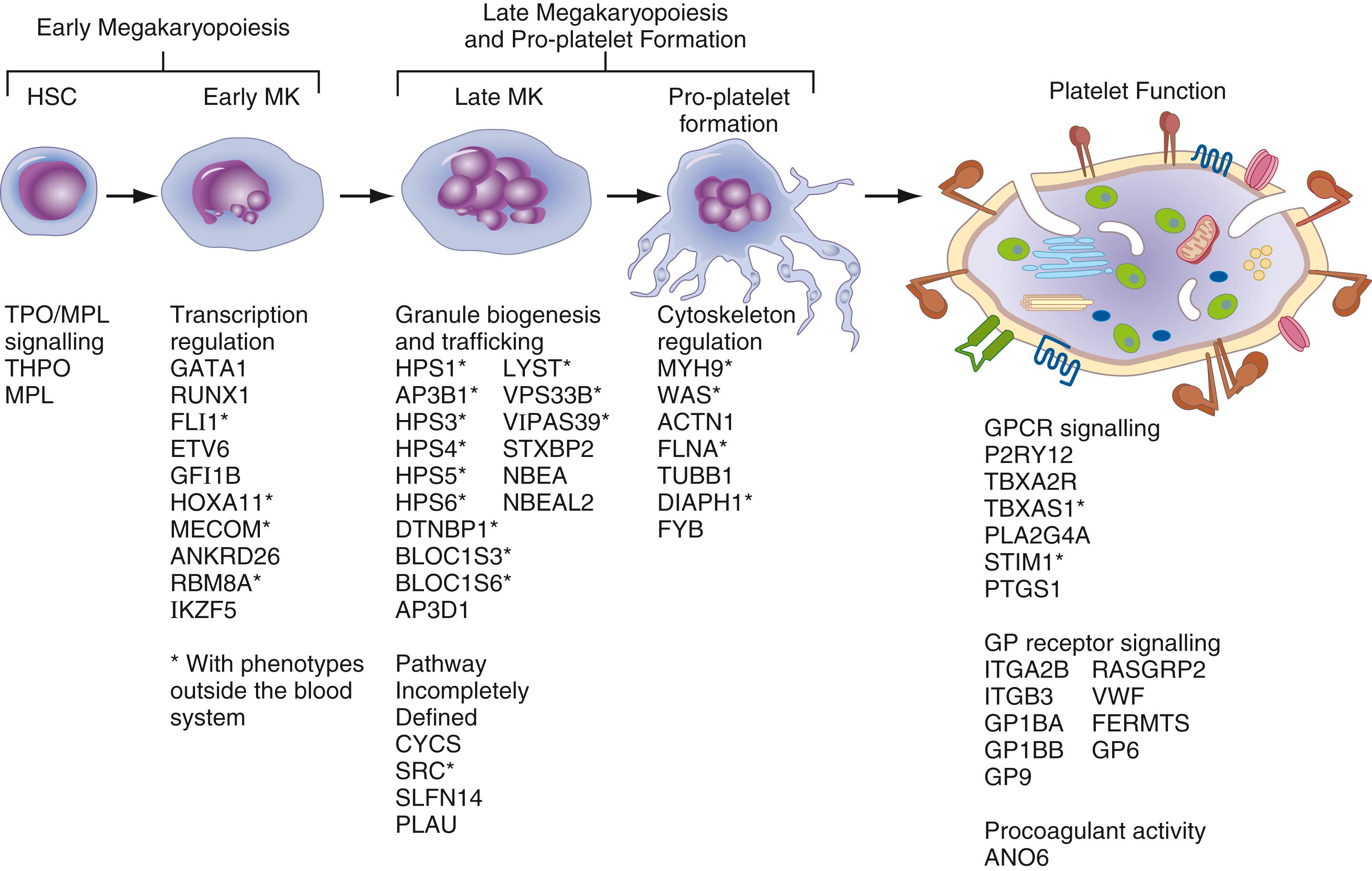
From a mechanistic perspective, inherited thrombocytopenias are associated with mutations in genes with diverse function. However, for some, the specific function in megakaryocytes/platelets is unclear. In the last 2 decades, there has been an explosive increase in our knowledge of gene mutations linked to inherited thrombocytopenias; over 20 genes are implicated ( ; ,; ; ) (see Fig. 41.5 ). These genes include transcription factors ( RUNX1 , FLI1 , GATA1, GFI1b , HOXA11 , ETV6 , MECOM/EVI1 , IKZF5 ), thrombopoietin receptor c- MpL , cytoskeletal proteins and related signaling ( MYH9 , TUBB1 , ACTN1 , FLNA , WASP , DIAPH1 , PTPRJ , SRC ), surface membrane glycoproteins and related signaling (GPIBA , GPIBB , GPIX , ITGA2B , ITGB3 ), proteins involved in vesicle transport ( NBEAL2 ), exon-junction complex involved in RNA processing ( RBM8A ), and cAMP-dependent protein kinase ( PRKACG ). Mutations in the ANKRD26 5′ untranslated region result in loss of RUNX1 and FLI1 binding, and ANKRD26 silencing ( ; ; ; ). The application of high-throughput sequencing permits identification of the gene abnormality in ∼50% of patients with inherited thrombocytopenias.
A better understanding of inherited thrombocytopenias is important beyond the predisposition to bleeding, which is variable and often mild. First, many patients are initially recognized in their adulthood ( ). In the absence of a family history, there is the risk for misdiagnosis as immune thrombocytopenia and the potential for unnecessary therapy, such as with steroids or splenectomy. Second, some gene mutations have prognostic implications, such as the predisposition to myeloid or lymphoid malignancies with RUNX1 , ANKRD26 , and ETV6 mutations ( ; ); or worsening renal function or hearing loss, as with MYH9 mutations . Further, there may be therapeutic implications, as in the potential role of eltrombopag in patients with MYH9 mutations ( ). Moreover, some reports have documented recurrence of leukemia following hematopoietic stem cell transplantation of the patient from an undiagnosed sibling donor with an unrecognized RUNX1 mutation ( ; ). Lastly, several entities are associated with platelet function abnormalities as well, as in patients with RUNX1 and other transcription factor mutations ( ) (see later discussion).
From a clinical perspective, patients with inherited thrombocytopenias may be characterized based on inheritance patterns or platelet size ( Table 41.3 ) or diameter ( , ; ; , ).
| Small Platelets (MPV <7 fL) | Normal-Sized Platelets (MPV 7–11 fL) | Large Platelets (MPV>11 fL) |
|---|---|---|
| Wiskott-Aldrich syndrome | Inherited amegakaryocytic thrombocytopenia | MYH9- related disorders |
| X-linked thrombocytopenia | Thrombocytopenia absent radius syndrome | Bernard-Soulier syndrome |
| FYB -related thrombocytopenia | Radioulnar synostosis with amegakaryocytic thrombocytopenia | ITGA2B/ITGB3 -related thrombocytopenia |
| PTPRJ -related thrombocytopenia | RUNX1 mutations (FPD/AML) | Gray platelet syndrome |
| Jacobsen/Paris-Trousseau syndrome | Velocardiofacial syndrome | |
| ANKRD26- related thrombocytopenia | GATA1 –related thrombocytopenia | |
| ETV6 -related thrombocytopenia IKZF5 -related thrombocytopenia | Type 2B von Willebrand disease/Platelet-type von Willebrand disease | |
| CYCS -related thrombocytopenia | ACTN1 -related thrombocytopenia | |
| TUBB1 -related macrothrombocytopenia | ||
| FLNA -related macrothrombocytopenia | ||
| DIAPH1 -related macrothrombocytopenia | ||
| PRKACG -related macrothrombocytopenia | ||
| GNE -related macrothrombocytopenia | ||
| SLFN14 -related macrothrombocytopenia | ||
| TPM4 -related macrothrombocytopenia | ||
| GALE -related macrothrombocytopenia | ||
| Thrombocytopenia associated with sitosterolemia |
The best recognized and most common of the inherited thrombocytopenias are the diverse group of autosomal-dominant syndromes, referred to as MYH9-related disorder ( MYH9-RD ) ( ; ). These include the May-Hegglin anomaly, Fechtner syndrome, Epstein syndrome, and Sebastian syndrome and share features of increased platelet size, cytoplasmic inclusions in leukocytes (Döhle bodies), and premature release of platelets. They arise from mutations in MYH9 encoding the nonmuscle myosin heavy chain IIA, a contractile cytoskeletal protein. All MYH9 syndromes have macrothrombocytopenia; other features such as nephritis, sensorineural deafness, and cataracts serve to distinguish them ( ; ). In patients having familial platelet disorder with predisposition to acute myeloid leukemia (FPD/AML), autosomal-dominant thrombocytopenia is secondary to mutations in the RUNX1 gene ( ; ). In these patients, platelet size is normal and their function is abnormal ( , ; ) (see later discussion). Patients with platelet-type von Willebrand disease (VWD) are characterized by thrombocytopenia, gain-of-function mutations in GPIBA , and enhanced responsiveness to ristocetin on platelet aggregation ( ). Other thrombocytopenias inherited in an autosomal-dominant manner include velocardiofacial syndrome and DiGeorge syndrome, which arise due to deletions within chromosome 22q11 and are associated with cardiac abnormalities, parathyroid and thymus insufficiencies, cognitive impairment, and facial dysmorphology (velocardiofacial only); and the Paris-Trousseau/Jacobsen syndrome, which is characterized by psychomotor retardation and facial and cardiac abnormalities, and arises due to deletion of a portion of chromosome 11,11q23-24, which encompasses the transcription factor FLI1 gene. Platelets in the latter disorder are increased in size and have giant α-granules. A dominant form of macrothrombocytopenia (Mediterranean macrothrombocytopenia, Bolzano variant) has been described in southern Europe; this has been associated with mutations in GPIbα and considered a heterozygous form of Bernard-Soulier syndrome (BSS) ( ). Autosomal-dominant BSS resulting from a point mutation in a leucine tandem repeat of GPIbα has been described in the American population ( ). Autosomal-dominant thrombocytopenias have been reported in association with mutations in the genes encoding cytoskeletal protein β-1 tubulin TUBB1 ( TUBB1 ) and α actinin-1 ( ACTN1 ), cytochrome c ( CYCS ), ANKRD26 , and PRKACG ( ; , ; ; ). ANKRD26 mutations are associated with increased risk of hematologic myeloid malignancies ( ). Autosomal-dominant inherited macrothrombocytopenia has been linked to DIAPH1 , which, like MYH9-RD, is associated with hearing loss ( ), and to mutations in genes encoding GPIIb (ITGA2B) or GPIIIa (ITGB3) ; these lead to constitutive activation of the GPIIb-IIIa integrin complex ( , ). Other gene mutations that have been linked to autosomal-dominant inherited thrombocytopenia include SFLN4 , TPM4 , and SRC ( ). SRC mutations have also been associated with α-granule deficiency and myelofibrosis (MF) ( ). Most recently, mutations in another TF, IKZF5, have also been linked to autosomal-dominant thrombocytopenia ( ).
In classical BSS, macrothrombocytopenia results from biallelic mutations involving the GPIb-IX-V complex (see later discussion). Congenital amegakaryocytic thrombocytopenia (CAMT) is an autosomal-recessive disorder associated with mutations in the thrombopoietin receptor MPL . It is characterized by severe thrombocytopenia and absence of megakaryocytes in the bone marrow. Other causes of recessive thrombocytopenia include the gray platelet syndrome (see later discussion) linked to mutations in the NBEAL2 gene, which encodes a BEACH protein involved in vesicular trafficking ( ; ; ). Thrombocytopenia with absent radii (TAR) syndrome is associated with skeletal abnormalities and inherited in an autosomal-recessive manner. Other genes that cause an autosomal-recessive thrombocytopenia involve mutations in FYB , GNE , and GALE , each with distinct features or mechanisms. Small platelets are present in patients with FYB mutation, GNE mutations increase platelet clearance, and mutations in GALE have effects on galactose metabolism and glycosylation ( ). Recently, biallelic loss-of-function variants in PTPRJ , which encodes for a receptor-like protein tyrosine phosphatase, have also been associated with microthrombocytopenia, with spontaneous bleeding and impaired platelet responses to collagen ( ).
Patients with Wiskott-Aldrich syndrome (WAS) and the related X-linked thrombocytopenia have mutations in the WAS gene ( ; ). These patients characteristically have small platelets and the thrombocytopenia may occur in the absence of other immunologic features of the syndrome. Mutations in transcription factor GATA1 are associated with thrombocytopenia, anemia, and alteration in red cell morphology ( ). Mutations in the FLNA gene, which encodes filamin A, are associated with the X-linked dominant syndromes encompassing periventricular nodular heterotopia and otopalatodigital spectrum of disorders ( ); they have macrothrombocytopenia. The FLNA mutation has been also identified as a cause of nonsyndromic isolated thrombocytopenia.
Immune thrombocytopenias (ITPs) are a heterogeneous group of disorders characterized by autoimmune-mediated platelet destruction ( ; ). These disorders are also associated with impaired platelet production ( ). Primary ITP is a diagnosis of exclusion, made in the absence of other causes or disorders associated with thrombocytopenia ( Table 41.4 ). Secondary ITP (see Table 41.4 ) consists of all forms of immune-mediated thrombocytopenia except primary ITP. The clinical history is usually helpful in arriving at a tentative diagnosis, in particular in distinguishing between the newly diagnosed, persistent, chronic, and severe forms of secondary ITP, as defined in Table 41.4 . A platelet count of <100,000 platelets/μL has been recommended as a threshold for diagnosis of ITP ( ). This threshold seeks to avoid overdiagnosis of disease in apparently healthy people with platelet counts of 100 to 150,000/μL and to avoid inclusion of many women with pregnancy-related thrombocytopenia. Several expert panels ( ; ; ) have addressed critical issues concerning the diagnosis and management of ITP. No single laboratory test for the diagnosis of ITP constitutes a gold standard status. Several laboratory approaches were deemed to be either of “potential utility” or of “unproven or uncertain benefit,” as shown in Table 41.4 .
Modified with permission from Rodeghiero F, Stasi R, Gernsheimer T: Standardization of terminology, definitions and outcome criteria in immune thrombocytopenic purpura of adults and children: report from an international working group, Blood 113:2386–2393, 2009.
Modified with permission from Provan D, Stasi R, Newland AC: International consensus report on the investigation and management of primary immune thrombocytopenia, Blood 115:168–186, 2010.
| PROPOSED DEFINITIONS OF DISEASE | ||
| Primary ITP | Secondary ITP: All Forms of Immune-Mediated Thrombocytopenia Except Primary ITP ∗ | |
|
|
|
| RECOMMENDATIONS FOR THE DIAGNOSIS OF ITP IN CHILDREN AND ADULTS | ||
| Basic Evaluation | Tests of Potential Utility in the Management of an ITP Patient | Tests of Unproven or Uncertain Benefit |
|
|
|
∗ The acronym ITP should be followed by the name of the associated disease (for thrombocytopenia after exposure to drugs, the term drug-induced should be used) in parentheses, for example, “secondary ITP (lupus-associated),” “secondary ITP (HIV-associated),” and “secondary ITP (drug-induced).”
∗∗ Quantitative immunoglobulin level measurement should be considered in children with ITP and is recommended in children with persistent or chronic ITP as part of the reassessment evaluation.
† Recommended by the majority of international consensus panel members for adult patients regardless of geographic locale.
Antiplatelet antibodies, many targeted against specific platelet glycoproteins (see later discussion), can be detected only in approximately 60% of patients with ITP, which may be because of unrecognized platelet antigens, limited test sensitivity, or other platelet loss mechanisms ( , ). Of particular interest, antecedent infectious diseases are present in approximately 60% of pediatric ITP patients. Molecular mimicry, in which immune responses initially directed against an infectious organism cross-react with platelet antigens in both children and adults, appears likely in a number of instances, including infection with human immunodeficiency virus and hepatitis C virus ( ; ; ; ; ). There is an association between Helicobacter pylori infection and ITP ( ; ; ). In addition to the accelerated platelet destruction in ITP, there is also defective platelet production ( ; , ). The observations that thrombopoietin mimetic agents are effective in increasing the platelet counts in these patients add further support for impaired platelet production in ITP ( ).
In both children and adults, there is insufficient evidence to recommend or suggest the routine use of antiplatelet, antiphospholipid and antinuclear antibodies, thrombopoietin levels, or platelet parameters obtained on automated analyzers in the evaluation of patients with suspected ITP ( ; ). A bone marrow examination is not necessary irrespective of age in patients presenting with typical ITP.
General treatment principles in primary ITP include immunosuppression, increasing platelet production, or decreasing platelet clearance, alone or in combination ( ; ). First-line treatment includes short-duration corticosteroids and/or intravenous immunoglobulin; second-line therapies include thrombopoietin receptor agonists, rituximab (a chimeric antibody against CD20 on B cells) and splenectomy. For refractory patients, other treatment strategies may be employed ( ; ).
Thrombocytopenia can be caused by a large number of drugs. DITP may be induced by classic drug-dependent antibodies (e.g., quinine), haptens (e.g., penicillin), fiban-dependent antibodies (e.g., tirofiban, integrilin), monoclonal antibodies (abciximab), autoantibodies (e.g., gold), and immune-complex formation (e.g., heparin, protamine) ( ; ; ; ; ). Most commonly implicated drugs include quinine, quinidine, trimethoprim-sulfamethoxazole, vancomycin, and piperacillin/tazobactam ( ; , ). Recently, oxaliplatin has been implicated to cause thrombocytopenia due to drug-dependent antibodies ( ). Other chemotherapy agents implicated in DITP include cyclophosphamide, irinotecan, dactinomycin, fludarabine, and cisplatin. A list of drugs implicated in DITP is provided in several publications ( ; ; ). Information is available at www.uptodate.com/contents/drug-induced-thrombocytopenia .
The clinical features of DITP include a platelet count less than 20,000/μL and bleeding symptoms that typically begin 5 to 10 days after starting the drug. Interestingly, with GPIIb-IIIa antagonist drugs (“fibans”) eptifibatide and tirofiban, acute severe thrombocytopenia may occur, even following the first exposure to the drug ( ). This acute thrombocytopenia results from preexisting antibodies in the patients binding to novel epitopes exposed in the drug-bound GPIIb-IIIa complex. With abciximab, which is a chimeric human-mouse Fab fragment specific for GPIIIa, preexisting antibodies against murine determinants on the chimeric antibody cause acute thromocytopenia ( ). The targets of drug-dependent antibodies in patients with DITP due to quinine, sulfonamides, and others are often epitopes on platelet GPIIb-IIIa or GPIb-IX ( ). In the case of gold and procainamide, autoantibodies are induced that have specificity for platelet GP. Heparins (see later discussion) and protamine ( ; ; ) induce thrombocytopenia by formation of immune complexes that bind and activate platelets.
Laboratory assessment for DITP employs normal test platelets as the target for antibody binding in the presence, but not the absence, of added drug. Recommendations regarding such testing and the appropriate controls have been advanced ( ). While a positive test generally carries high specificity for DITP, a negative test result does not necessarily exclude DITP due to the low sensitivity that has been observed with such testing ( ).
The laboratory approach to heparin-induced thrombocytopenia is discussed in Chapter 43 .
In most patients, thrombocytosis is acquired. In the rare patients with inherited thrombocytosis, this results from gain-of-function mutations in either thrombopoietin or its receptor (MPL) ( ; ). Acquired thrombocytosis may be primary, related to autonomous clonal bone marrow disorders, such as the myeloproliferative neoplasms (MPNs) and myelodysplastic syndromes, or reactive and secondary to conditions such as infections, chronic inflammation, malignancy, hemolysis, iron-deficiency anemia, or splenectomy ( Box 41.1 ) ( ; ; ; ) (see later discussion). The blood film should be reviewed to confirm the increase in platelets and exclude spurious thrombocytosis due to red cell abnormalities (microspherocytes and fragments). A number of clinical and laboratory findings may provide clues as to whether one is dealing with an autonomous clonal process or a reactive process ( Table 41.5 ). This distinction is important because of the implications regarding the potential for thrombohemorrhagic complications and disease transformation in MPN, and regarding treatment strategies (cytoreduction). The platelet counts do not provide a reliable clue in this distinction. Extreme thrombocytosis (platelet counts greater than 1000 × 10 9 /L), may occur in patients with either process; surgical complications and hematologic malignancies were the two dominant causes in one series with a substantial difference in etiology between inpatients and outpatients ( ). Patients with MPN may have abnormalities in platelet and megakaryocyte structure and platelet function (see later discussion). The presence of cytogenetic abnormalities, such as in JAK2V617F and calreticulin, are strongly associated with primary thrombocytosis ( ; ; ; ). Lastly, studies utilizing platelet transcript profiling of patients with thrombocytosis have shown that specific biomarker gene subsets may predict their thrombocytosis class ( ; ).
Acute blood loss
Recovery (rebound) from thrombocytopenia
Acute infection or inflammation
Response to exercise
Iron deficiency
Hemolytic anemia
Asplenia (e.g., after splenectomy)
Cancer
Chronic inflammatory or infectious diseases
Connective tissue disorders
Temporal arteritis
Inflammatory bowel disease
Tuberculosis
Chronic pneumonitis
Drug reactions
Vincristine
All- trans -retinoic acid
Cytokines
Growth factors
| Finding | Clonal Thrombocytosis ∗ | Secondary (Reactive) Thrombocytosis |
|---|---|---|
| Underlying systemic disease | No | Often clinically apparent |
| Digital or cerebrovascular ischemia | Characteristic | No |
| Large-vessel arterial or venous thrombosis | Increased risk | No |
| Bleeding complications | Increased risk | No |
| Splenomegaly | Yes, in about 40% of patients | No |
| Peripheral blood smear | Variable, may include giant platelets | Normal platelets |
| Platelet function | May be abnormal | Normal |
| Bone marrow megakaryocytes | ||
|
Increased | Increased |
|
Giant, dysplastic forms with increased ploidy; associated with large masses of platelet debris | Normal |
| Presence of cytogenetic abnormalities (mutations in JAK2 , MPL , CALR , BCR-ABL1 ) | Present | Absent |
∗ Clonal thrombocytosis includes essential thrombocythemia and other myeloproliferative disorders.
Patients with MPN may develop bleeding or thrombotic events. Unless additional associated risk factors, such as malignancy, are present, thrombotic events are unlikely in reactive thrombocytosis ( ). However, in one study ( ), reactive thrombocytosis occurred in about 10% of patients in the recovery phase after an admission to the intensive care unit and was associated with an increase in venous thromboembolism.
Box 41.2 provides a list of inherited platelet disorders associated with impaired platelet function ( Fig. 41.6 ). Figure 41.5 shows the genes underlying inherited platelet disorders, including those of function and number. Although rare, these disorders provide enormous insights into platelet physiology. In most patients with inherited abnormalities of platelet aggregation and secretion, the underlying molecular-genetic mechanisms remain unknown. Not all disorders resulting in an impaired platelet role in hemostasis are due to a defect in the platelets per se. Examples are patients with VWD and afibrinogenemia, with deficiencies of specific plasma proteins essential for normal platelet function. In VWD, platelet adhesion to subendothelium is abnormal, which is also the case in patients with BSS, in whom platelets are deficient in the GPIb-IX-V complex, the receptor for VWF on platelets (see Fig. 41.6 ). Binding of fibrinogen to the GPIIb-IIIa complex is a prerequisite for platelet aggregation. Thus, platelet aggregation on activation is impaired in both inherited afibrinogenemia and in Glanzmann thrombasthenia, in which platelets are deficient in platelet membrane GPIIb-IIIa complex. Platelet aggregation and secretion are the end result of numerous processes that follow the initial interaction of an agonist with the platelet (see Figs. 41.2 and 41.6 ). Thus, abnormalities in many platelet events may lead to a decrease in these responses. Patients with defects in “platelet secretion and signal transduction” are a heterogeneous group considered together for convenience rather than based on an understanding of the molecular abnormality. The common characteristics in these patients are abnormal aggregation responses and an inability to release dense granule contents upon activation of platelet-rich plasma with agonists such as ADP, epinephrine, and collagen ( ). In aggregation studies, the second wave of aggregation is blunted or absent. The platelet dysfunction in such patients arises from diverse mechanisms. A small proportion of these patients have a deficiency of dense granule stores (storage pool deficiency). In some of the others, impaired platelet function arises due to aberrations in signal transduction events that lead to secretion and aggregation. Another group consists of patients who have an abnormality in platelet interactions with coagulation proteins; the best described is Scott syndrome, characterized by impaired expression of surface PS on activation ( , ; ). Defects related to platelet cytoskeleton or structural proteins may also be associated with platelet dysfunction, as in WAS or in patients with abnormalities related to kindlin-3. Several reports document impaired platelet function associated with mutations in transcription factors (RUNX1, GATA1, FLI1, GFI1b, and others) that regulate gene expression in megakaryocytes and platelets. As a group, they may be more common than appreciated. In addition to the patients described earlier, there are patients who have abnormal platelet function associated with systemic disorders or are syndromic, such as Hermansky-Pudlak syndrome or Chédiak-Higashi syndrome ( ; ). These and other entities are described in the following sections. The gene symbols, where relevant, are shown in italics.
Abnormalities of glycoprotein adhesion receptors
Integrin α IIb β 3 (glycoprotein IIb/IIIa; CD41/CD61): Glanzmann thrombasthenia
Glycoproteins Ib (CD42b,c)/IX (CD42a)/V: Bernard-Soulier syndrome
Glycoprotein Ib α (CD42b,c): Platelet-type (pseudo-) von Willebrand disease
Integrin α 2 β 1 (glycoprotein Ia/IIa; VLA-2; CD49b/CD29)
CD36 (glycoprotein IV)
Glycoprotein VI
Abnormalities of platelet granules
δ -Storage pool deficiency
Gray platelet syndrome ( α -storage pool deficiency)
α , δ -Storage pool deficiency
Quebec platelet disorder
Abnormalities of platelet receptors, signaling and secretion
Defects in platelet agonist receptors or agonist-specific signal transduction
Adenosine diphosphate (ADP) receptor defects (P2Y 12 , P2X 1 ),
Thromboxane A 2 receptor defect
Collagen receptor defect
Epinephrine receptor defect
Defects in guanosine triphosphate (GTP)–binding proteins
G α q deficiency
G α s hyperfunction and genetic variation in extra-large G α s
G α i1 deficiency
CaLDAG-GEFI deficiency ( RASGRP2 )
Phospholipase C (PLC)- β 2 deficiency and defects in PLC activation
Calcium mobilization
Defects in protein phosphorylation protein kinase C (PKC)- θ deficiency
Defects in arachidonic acid metabolism and thromboxane production
Phospholipase A 2 deficiency
Cyclooxygenase [prostaglandin H 2 synthase-1 deficiency],
Thromboxane synthase deficiency
Abnormalities of platelet coagulant activity (Scott syndrome)
Abnormalities of a cytoskeletal structural protein
β 1 -tubulin
Filamin A
Abnormalities in cytoskeletal linking proteins
Wiskott-Aldrich syndrome protein (WASP)
Kindlin-3: Leukocyte adhesion defect (LAD)-III; LAD-1 variant; integrin activation deficiency disease defect (IADD)
Abnormalities of transcription factors leading to functional defects
RUNX1 (familial platelet dysfunction with predisposition to acute myelogenous leukemia)
GATA-1
FLI1 (Paris-Trousseau/Jacobsen syndrome)
GFI1B
ETV6
Other Disorders
Arthrogryposis renal dysfunction-cholestasis syndrome (ARC) ( VPS33B , VPS16B )
Glanzmann thrombasthenia is a rare autosomal-recessive disorder characterized by markedly impaired platelet aggregation in response to activation with all physiologic agonists, a prolonged bleeding time, and relatively more severe mucocutaneous bleeding manifestations than most inherited platelet function disorders ( ; ; ; ). It has been reported in clusters in populations where consanguinity is common. The primary abnormality in thrombasthenia is a quantitative or qualitative defect in the GPIIb-IIIa complex, a heterodimer consisting of GPIIb ( ITGA2B ) and GPIIIa ( ITGB3 ) whose synthesis is governed by two distinct genes located on chromosome 17. Thus, thrombasthenia may arise due to a mutation in either gene, leading to decreased platelet surface expression of the complex. Because of this, fibrinogen binding to platelets on activation and aggregation is impaired. Numerous distinct mutations involving ITGA2B and ITGB3 have been described in thrombasthenia ( ; ) and included in the database for this entity ( https://glanzmann.mcw.edu/ ). Clot retraction, a function of the interaction of GPIIb-IIIa with the platelet cytoskeleton, is also impaired. Investigation of Glanzmann thrombasthenia has advanced the understanding of platelet pathophysiology and development of major antiplatelet agents ( ).
The diagnostic hallmark of thrombasthenia is absence or marked decrease of platelet aggregation (see Fig. 41.3 ) in response to virtually all platelet agonists (except ristocetin), with absence of both the primary and secondary wave of aggregation; the shape change response is preserved. Platelet dense granule secretion may be decreased with weak agonists (e.g., ADP) but normal on activation with thrombin. Heterozygotes have approximately half the number of platelet GPIIb-IIIa complexes, the platelet aggregation responses are normal, and these individuals do not have a bleeding disorder.
Because the platelet antigen Pl A1 is associated with glycoprotein IIIa, this antigen is typically decreased in patients with Glanzmann thrombasthenia ( ; ). The diagnosis of Glanzmann thrombasthenia can be established by demonstrating a marked decrease in platelet GPIIb-IIIa using flow cytometry ( ; ), as illustrated in Figure 41.4 . Definitive characterization of the mutations in ITGA2B and ITGB3 may be undertaken by molecular techniques ( ; ; ). Although inherited afibrinogenemia is also characterized by a similar absence of platelet aggregation, in this disorder prothrombin time (PT), activated partial thromboplastin time (APTT), and thrombin time are markedly prolonged, whereas they are normal in thrombasthenia.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here