Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The pharynx is the crossroads of respiration, speech, and swallowing. During respiration, the pharynx is an active conduit for the passage of air from the nasopharynx to the laryngeal aditus. During speech, the pharynx functions as a resonating chamber, changing size and shape to alter sounds. During swallowing, the pharynx directs the bolus into the esophagus and prevents the bolus from entering the tracheobronchial tree. Disorders of the pharynx may therefore be manifested by respiratory, speech, or swallowing dysfunction. Patients may complain of dysphagia, odynophagia, choking, or a feeling of a lump in the throat unassociated with swallowing (a globus sensation). Soft palate insufficiency may be suggested by nasal regurgitation or a nasal voice quality. Recurrent pneumonia, asthma, chronic bronchitis, or coughing may also indicate pharyngeal dysfunction.
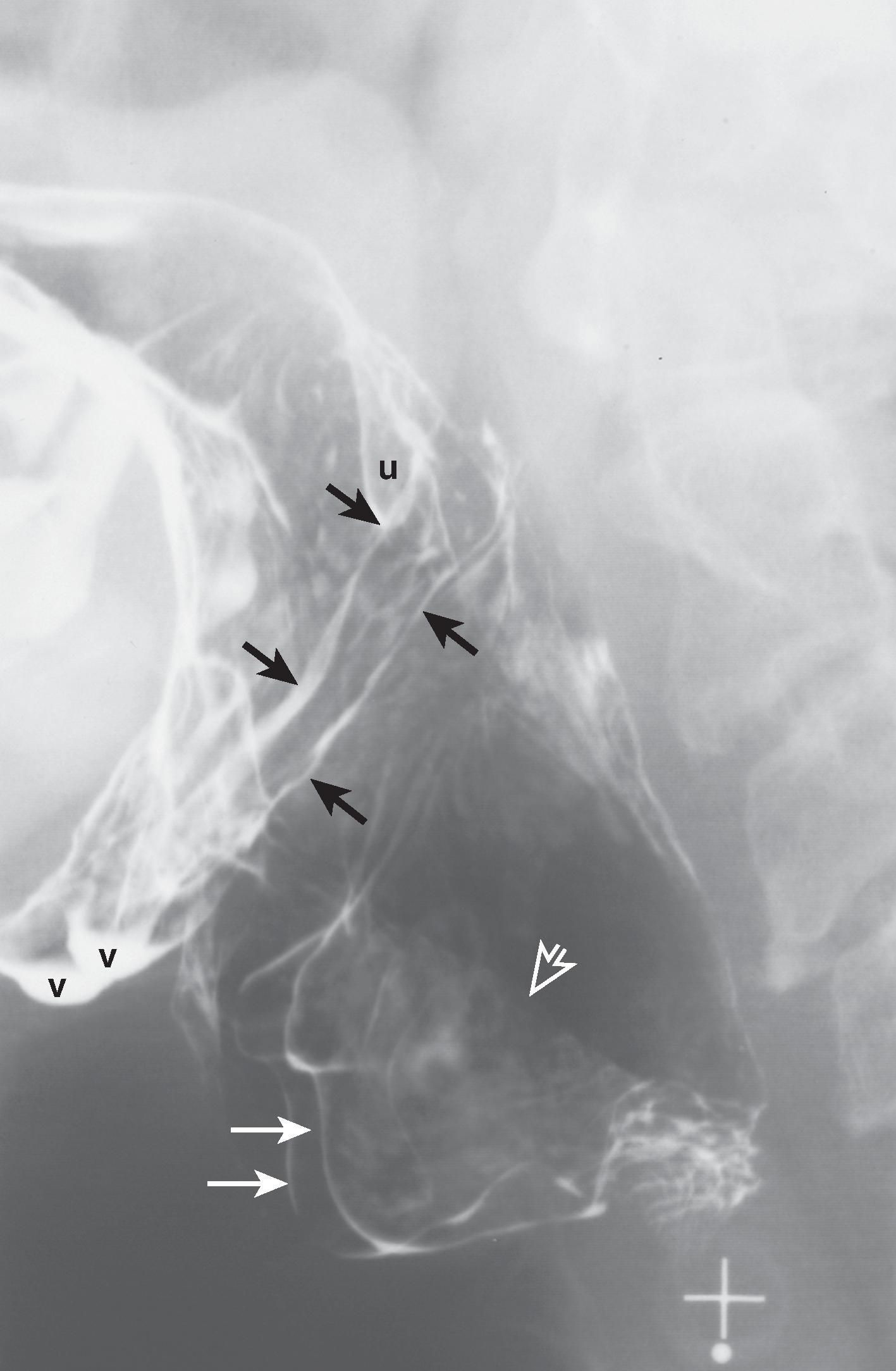
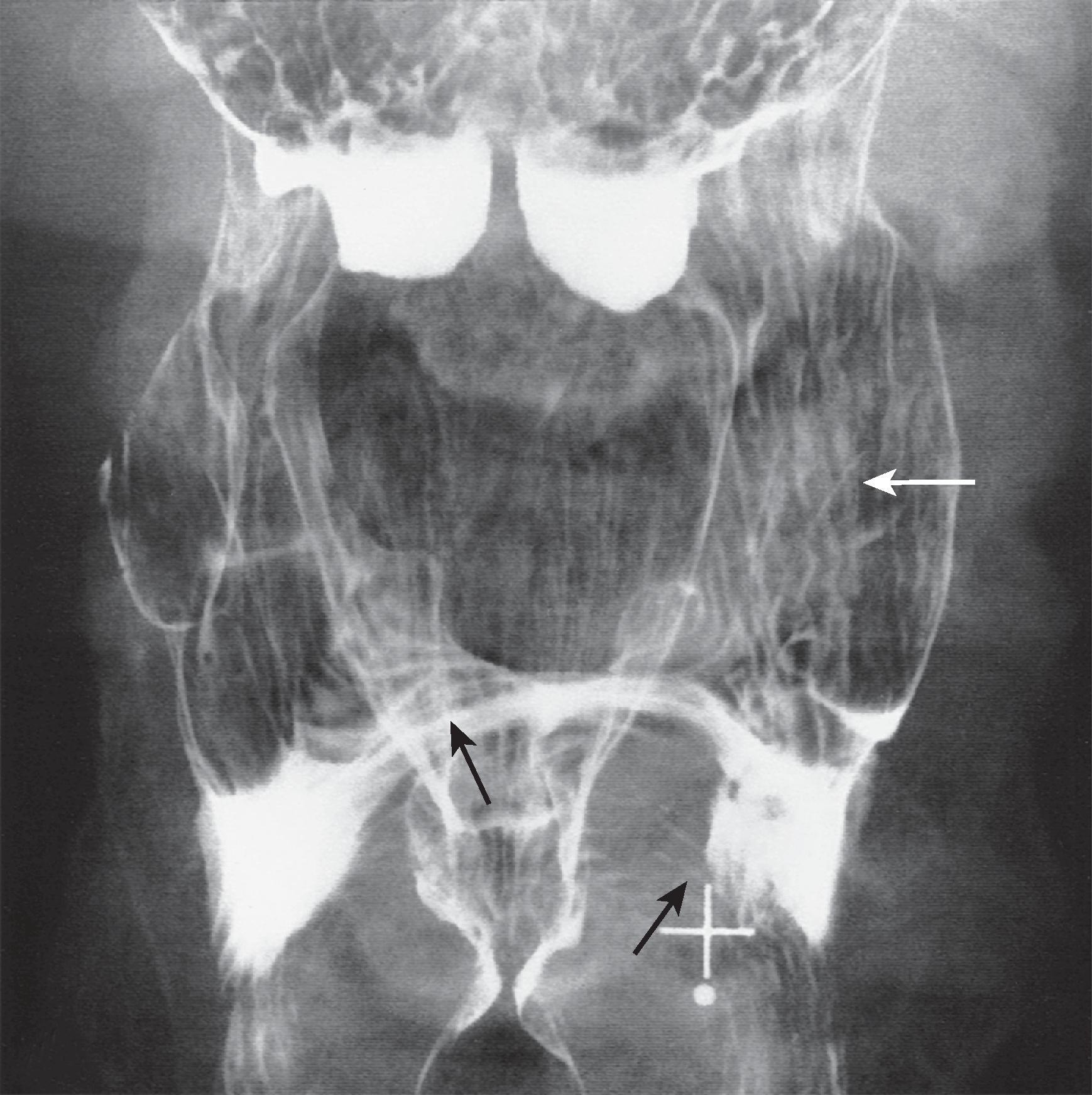
The pharynx is a funnel-shaped tube of skeletal muscle extending from the cranial base to the lower margin of the cricoid cartilage ( Fig. 4.1 ). The pharynx lies anterior to the cervical spine, prevertebral muscles, and loose connective tissue of the retropharyngeal space. The pharynx is confined laterally by the muscles of the neck, lateral portions of the hyoid bone and thyroid cartilage, and carotid sheath. The pharynx and larynx are intimately related ( Fig. 4.2 ) embryologically and anatomically.
![Fig. 4.1, Basic structures of the normal pharynx. (A) Double-contrast frontal view of the pharynx shows the contours of the superior surface of the tongue ( black arrow ), tonsillar fossa (right tonsillar fossa [ white arrow ]), valleculae (left vallecula [ v ]), and lateral wall ( open arrow ) of the piriform sinus (right piriform sinus [ p ]). The median glossoepiglottic fold ( arrowhead ) divides the space behind the tongue base into the two valleculae. The surface of the base of the tongue ( T ) has a reticular appearance en face because of the underlying lingual tonsil. (B) Double-contrast lateral view of the pharynx (during phonation) shows the contours of the soft palate ( s ), base of the tongue ( t ), epiglottis ( e ), valleculae ( v ), posterior pharyngeal wall ( open arrow ), lower piriform sinuses ( p ), and collapsed pharyngoesophageal segment ( arrowheads ). Note the height of the soft palate in relation to the C1 vertebral body and the thickness of the space behind the barium-coated pharyngeal mucosa, composed of pharyngeal musculature, fascial planes, prevertebral muscles, and anterior longitudinal ligament. (B, From Rubesin SE, Jones B, Donner MW. Contrast pharyngography: the importance of phonation. AJR. 1987;148:269–272.) Fig. 4.1, Basic structures of the normal pharynx. (A) Double-contrast frontal view of the pharynx shows the contours of the superior surface of the tongue ( black arrow ), tonsillar fossa (right tonsillar fossa [ white arrow ]), valleculae (left vallecula [ v ]), and lateral wall ( open arrow ) of the piriform sinus (right piriform sinus [ p ]). The median glossoepiglottic fold ( arrowhead ) divides the space behind the tongue base into the two valleculae. The surface of the base of the tongue ( T ) has a reticular appearance en face because of the underlying lingual tonsil. (B) Double-contrast lateral view of the pharynx (during phonation) shows the contours of the soft palate ( s ), base of the tongue ( t ), epiglottis ( e ), valleculae ( v ), posterior pharyngeal wall ( open arrow ), lower piriform sinuses ( p ), and collapsed pharyngoesophageal segment ( arrowheads ). Note the height of the soft palate in relation to the C1 vertebral body and the thickness of the space behind the barium-coated pharyngeal mucosa, composed of pharyngeal musculature, fascial planes, prevertebral muscles, and anterior longitudinal ligament. (B, From Rubesin SE, Jones B, Donner MW. Contrast pharyngography: the importance of phonation. AJR. 1987;148:269–272.)](https://storage.googleapis.com/dl.dentistrykey.com/clinical/PharynxNormalAnatomyandFunctionandExaminationTechniques/0_3s20B978032364082400004X.jpg)
![Fig. 4.2, Relationship of larynx to pharynx. (A) In a patient with laryngeal penetration, frontal view of the pharynx shows barium coating the false vocal cords (right false vocal cord [ F ]), true vocal cords (right true vocal cord [ T ]), and laryngeal ventricle (right laryngeal ventricle, black arrow ). As the larynx protrudes into the midhypopharynx, arcuate lines ( white arrows ) are formed. (B) Lateral view of the pharynx shows the relationship of the barium-coated laryngeal vestibule ( small white arrows ) to the laryngeal ventricle ( small black arrows ). Note the angle of the laryngeal ventricle atop the true vocal cords and tilt of the true vocal cords. The anterior walls of the right piriform sinus ( large white arrows ) and left piriform sinus ( arge black arrows ) are seen as anteriorly convex lines. The mucosa ( m ) overlying the muscular process of the arytenoid cartilages lies below the aryepiglottic fold ( open arrow ). The lower hypopharynx ( arrowhead ) is closed at rest. E, epiglottis. (B, From Rubesin SE, Glick SN. The tailored double-contrast pharyngogram. Crit Rev Diagn Imaging. 1988;28:133–179.) Fig. 4.2, Relationship of larynx to pharynx. (A) In a patient with laryngeal penetration, frontal view of the pharynx shows barium coating the false vocal cords (right false vocal cord [ F ]), true vocal cords (right true vocal cord [ T ]), and laryngeal ventricle (right laryngeal ventricle, black arrow ). As the larynx protrudes into the midhypopharynx, arcuate lines ( white arrows ) are formed. (B) Lateral view of the pharynx shows the relationship of the barium-coated laryngeal vestibule ( small white arrows ) to the laryngeal ventricle ( small black arrows ). Note the angle of the laryngeal ventricle atop the true vocal cords and tilt of the true vocal cords. The anterior walls of the right piriform sinus ( large white arrows ) and left piriform sinus ( arge black arrows ) are seen as anteriorly convex lines. The mucosa ( m ) overlying the muscular process of the arytenoid cartilages lies below the aryepiglottic fold ( open arrow ). The lower hypopharynx ( arrowhead ) is closed at rest. E, epiglottis. (B, From Rubesin SE, Glick SN. The tailored double-contrast pharyngogram. Crit Rev Diagn Imaging. 1988;28:133–179.)](https://storage.googleapis.com/dl.dentistrykey.com/clinical/PharynxNormalAnatomyandFunctionandExaminationTechniques/1_3s20B978032364082400004X.jpg)
The shape of the pharynx is determined by the underlying musculature, laryngeal cartilages, and supporting skeleton. Although the nasopharynx is primarily a respiratory tract structure, portions of the nasopharynx participate in the act of swallowing. The eustachian tube connects the middle ear with the nasopharynx, allowing equilibration of air pressures on the internal and external aspects of the tympanic membrane during swallowing. The salpingopharyngeal fold overlying the salpingopharyngeal muscle courses inferiorly from the torus tubarius down the lateral pharyngeal wall to the level of the soft palate, creating the fossa of Rosenmüller. During breathing, the eustachian tube is closed. When swallowing occurs, the salpingopharyngeal muscle attached to the lateral wall of the eustachian tube contracts, pulling the eustachian tube open.
The vertical (pharyngeal) surface of the base of the tongue is variably nodular because of underlying lymphoid tissue of the lingual tonsil (see Fig. 4.1A ). The median glossoepiglottic fold overlies the glossoepiglottic ligament, which courses from the base of the tongue to the epiglottis. The median glossoepiglottic fold divides the space between the tongue and the epiglottis into two sacs, also known as the valleculae ( Fig. 4.3 ). The lateral glossoepiglottic folds form the lateral walls of the valleculae. The pharyngoepiglottic folds course from the posterolateral portion of the valleculae into the lateral pharyngeal wall ( Fig. 4.4 ). These folds overlie the paired stylopharyngeal muscles, forming the posterolateral walls of the valleculae. The valleculae are spaces at rest but disappear during swallowing when the epiglottis inverts and the space behind the base of the tongue communicates freely with the remaining oropharynx.
![Fig. 4.3, Folds of the valleculae. Frontal view of the pharynx shows how the folds of the epiglottis and valleculae are accentuated by edema in a patient with chronic radiation change. The median glossoepiglottic fold ( black arrowhead ) divides the retroglottic space into the two valleculae (right vallecula [ V ]). The pharyngoepiglottic folds ( white arrow identifies the left pharyngoepiglottic fold) overlie the paired stylopharyngeal muscles and form part of the posterior wall of the valleculae. The epiglottic tip ( E ) and left aryepiglottic fold ( black arrow ) are also seen. Barium coats the laryngeal surface of the epiglottis because of laryngeal penetration. The interarytenoid notch ( white arrowhead ) lies between the swollen mucosa overlying the muscular processes of the arytenoid cartilages. Fig. 4.3, Folds of the valleculae. Frontal view of the pharynx shows how the folds of the epiglottis and valleculae are accentuated by edema in a patient with chronic radiation change. The median glossoepiglottic fold ( black arrowhead ) divides the retroglottic space into the two valleculae (right vallecula [ V ]). The pharyngoepiglottic folds ( white arrow identifies the left pharyngoepiglottic fold) overlie the paired stylopharyngeal muscles and form part of the posterior wall of the valleculae. The epiglottic tip ( E ) and left aryepiglottic fold ( black arrow ) are also seen. Barium coats the laryngeal surface of the epiglottis because of laryngeal penetration. The interarytenoid notch ( white arrowhead ) lies between the swollen mucosa overlying the muscular processes of the arytenoid cartilages.](https://storage.googleapis.com/dl.dentistrykey.com/clinical/PharynxNormalAnatomyandFunctionandExaminationTechniques/2_3s20B978032364082400004X.jpg)
The tonsillar fossa forms part of the lateral oropharyngeal walls. Each tonsillar fossa is bounded anteriorly by a palatoglossal fold (the anterior tonsillar pillar) and posteriorly by a palatopharyngeal fold (the posterior tonsillar pillar) overlying the palatopharyngeal muscle.
The rounded epiglottic tip rises above the level of the valleculae (see Figs. 4.1B and 4.3 ). The aryepiglottic folds connect the epiglottis with the mucosa overlying the muscular processes of the arytenoid cartilages (see Fig. 4.3 ). Occasionally, round bulges are seen in the lower aryepiglottic folds, reflecting the small cuneiform and corniculate cartilages embedded in these folds.
The shape of the hypopharynx is created primarily by its relationship to the posteriorly protruding larynx (see Figs. 4.1 and 4.2 ). Protrusion of the larynx into the pharynx creates two grooves in the anterolateral hypopharynx, also known as the piriform sinuses (recesses), which are pear-shaped structures that open posteriorly into the hypopharynx. Each piriform sinus is bounded medially by the aryepiglottic fold and mucosa overlying the muscular process of the arytenoid cartilage and laterally by the hyoid bone, thyrohyoid membrane, and thyroid cartilage. ,
The lower end of the hypopharynx is collapsed, except during the passage of a bolus. The posterior portion of the larynx (including the arytenoid cartilages, arytenoid muscles, and cricoid cartilage) protrudes deeply into the lower hypopharynx (see Fig. 4.2 ). The upper esophageal sphincter (formed predominantly by the cricopharyngeal muscle) is tonically contracted at rest, closing the pharyngoesophageal segment (see Fig. 4.2 ). As a result, the lower hypopharynx is markedly constricted in an anteroposterior direction and may not be appreciated on a frontal radiograph. The arcuate lower border of the hypopharynx seen on the frontal view reflects only the protrusion of the larynx into the hypopharynx (see Fig. 4.2A ).
The squamous mucosa of the lateral and posterior pharyngeal walls is closely apposed to the longitudinally striated inner longitudinal muscle layer and its aponeurosis. Only a thin tunica propria separates the epithelium from the muscle or elastic tissue of the aponeurosis. On double-contrast views, longitudinally oriented lines may, therefore, be seen on the lateral and posterior pharyngeal walls, reflecting apposition of the epithelium to the muscle ( Fig. 4.5 ).
Transversely oriented lines are seen on the anterior hypopharyngeal wall, where redundant squamous mucosa and submucosa overlie the muscular processes of the arytenoid cartilages and cricoid cartilage. Transverse lines and tissue bulging from the anterior wall of the pharyngoesophageal segment are caused by redundant mucosa and submucosa on the anterior hypopharyngeal wall, producing a normal finding known as the “postcricoid defect” ( Fig. 4.6 ). Demonstration of this redundant postcricoid mucosa on pharyngograms helps identify the location of the cricopharyngeal muscle.

The pharynx is arbitrarily divided into three parts—the nasopharynx (epipharynx), oropharynx (mesopharynx), and laryngopharynx (hypopharynx). The nasopharynx is primarily a respiratory tract structure continuous anteriorly with the nasal cavity. The superior and posterior walls of the nasopharynx abut the basisphenoid and basilar part of the occipital bone. The nasopharynx is separated inferiorly from the oropharynx by the soft palate (see Fig. 4.1 ). The velopharyngeal portal is the opening between the nasopharynx and oropharynx.
The oropharynx and hypopharynx are the divisions of the pharynx that participate in swallowing. The oral cavity opens into the oropharynx at the palatoglossal isthmus at the level of the anterior tonsillar pillars. The oropharynx lies posterior to the oral cavity, extending craniocaudally from the soft palate to the pharyngoepiglottic fold (see Fig. 4.4 ), a mucosal fold overlying the stylopharyngeal muscle. , The base of the tongue (see Fig. 4.1B ) forms the lower anterior wall of the oropharynx.
The hypopharynx lies behind and lateral to the larynx, extending from the level of the pharyngoepiglottic fold to the lower border of the cricopharyngeal muscle at the level of the inferior margin of the cricoid cartilage. The hypopharynx communicates with the larynx at the laryngeal aditus, formed by the epiglottis, aryepiglottic folds, and mucosa overlying the muscular process of the paired arytenoid cartilages (see Figs. 4.2 and 4.3 ). The hypopharynx communicates with the cervical esophagus at the pharyngoesophageal segment, whose walls are surrounded by the posterior lamina of the cricoid cartilage and cricopharyngeal muscle.
Pharyngeal function depends on coordinated, sequential contraction of the extrinsic muscles of the pharynx, which arise from the skull base, neck, tongue, mandible, and hyoid bone, and the intrinsic skeletal muscles of the pharynx and larynx ( Table 4.1 ). The pharynx and larynx are suspended as a unit from the skull base, tongue, mandible, and hyoid bone. The suspensory muscles of the hyoid bone (the suprahyoid muscles) include the following (with their cranial nerve innervations in parentheses): from the tongue, mandible, or both, the anterior belly of the digastric muscle (V3), geniohyoid muscle (XII, via C1-2), hyoglossal muscle (XII), and mylohyoid muscle (V3); and from the skull base, the posterior belly of the digastric muscle (VII) and stylohyoid muscle (VII). The major function of the suprahyoid muscle group related to swallowing is to elevate and fix the hyoid bone, a motion that contributes to elevating and widening the pharynx, tilting the epiglottis, and opening the pharyngoesophageal segment during the passage of a bolus.
| Visualized Motion | Cranial Nerve | Muscle(S) |
|---|---|---|
| Lip closure | VII | Orbicularis oris m., four others |
| Mastication | V3 | Masseter m. |
| Temporalis m., lateral and medial pterygoid m. | ||
| VII | Buccinator m. | |
| Bolus holding posteriorly | IX V3 VII XII |
Palatoglossus Tensor veli palatini Lingualis (Sensory) |
| Tongue protrusion | XII | Genioglossus |
| Tongue tip elevation | XII | Genioglossus |
| Tongue forming inclined plane | XII | Genioglossus, lingualis |
| Tongue base retraction | XII | Styloglossus, hyoglossus |
| Velopharyngeal portal closure | ||
| Soft palate elevation | X | Levator veli palatini m. |
| Lateral portal closure | X | Superior constrictor m. |
| Hyoid elevation (suprahyoid group) | V3 | Anterior belly digastric m., mylohyoid m. |
| VII | Stylohyoid m., posterior belly digastric m. | |
| XII (via C1, C2) | Geniohyoid m. | |
| Thyrohyoid apposition | XII (via C1, C2) | Thyrohyoid m. |
| Pharyngeal elevation | ||
| Suprahyoid group | See hyoid elevation. | |
| Intrinsic elevators | IX | Stylopharyngeus |
| IX, X | Palatopharyngeus | |
| IX, X | Salpingopharyngeus | |
| Epiglottic tilt | ||
| Extrinsic muscles | V3, VII, XII, | Suprahyoid group |
| XII (C1, C2) | Thyrohyoid m. | |
| Intrinsic muscles | X | Aryepiglottic m.,thyroepiglottic m |
| X | Oblique arytenoid m. | |
| Laryngeal vestibule closure | X | Thyroarytenoid m., vocal cord muscles |
| Pharyngeal clearance | X | Superior, middle,inferior constrictor m. |
| XII | Hyoglossus,styloglossus | |
| Upper esophageal sphincter opening | V3, VII, XII IX, X X |
Suprahyoid group Intrinsic elevators Constrictor muscles |
| Hyoid depression after swallow | C1, C2 | Sternohyoid, omohyoid, sternothyroid m. |
The soft palate is formed by an interweaving of muscles from the skull base (tensor veli palatini and levator veli palatini), tongue (palatoglossus muscle), and pharynx (palatopharyngeal muscle). The musculus uvulae is the only intrinsic muscle of the soft palate.
The tendon of the tensor veli palatini (V) forms the fibrous skeleton of the anterior portion of the soft palate. This muscle depresses the anterior soft palate during swallowing. The levator veli palatini (X) suspends the midportion of the soft palate. During swallowing, the levator veli palatini pulls the mid–soft palate superiorly and posteriorly. , The palatopharyngeal muscle (X) depresses the posterolateral soft palate, elevates the pharynx, and constricts the faucial isthmus. The palatoglossus muscle (X) pulls the soft palate and tongue toward each other. The musculus uvulae (X) shortens, thickens, and elevates the uvula.
The thyrohyoid muscle (XII, via C1-2) courses from the hyoid bone to the thyroid cartilage. Its major function is approximation of the hyoid bone and thyroid cartilage, an action that is partly responsible for closing the laryngeal vestibule. The infrahyoid depressors include the sternohyoid (C1-3), sternothyroid (C1-3), and omohyoid (C1-3) muscles.
Epiglottic tilt is accomplished by contraction of the suprahyoid muscles, thyrohyoid muscle, and intrinsic epiglottic musculature. , Contraction of the suprahyoid group pulls the hyoid bone superiorly and anteriorly beneath the mandible. Hyoid motion pulls on the hyoepiglottic ligament that courses from the inferior anterior hyoid bone to the petiole (lower tip) of the epiglottis. Hyoid motion, therefore, pulls the lower epiglottis anteriorly and superiorly, tilting the epiglottis toward a horizontal position as if the epiglottis were on a fulcrum. Contraction of the paired aryepiglottic and oblique arytenoid muscles pulls the epiglottic tip inferiorly. Contraction of the thyroepiglottic muscles pulls the sides of the epiglottis and aryepiglottic folds laterally. ,
Closure of the laryngeal aditus is not accomplished by epiglottic inversion alone. Thyrohyoid muscle contraction pulls the hyoid and thyroid cartilage together. Closure of the vocal cords and thyroarytenoid muscles helps close the laryngeal vestibule. Contraction of the transverse arytenoid muscle and aryepiglottic-oblique arytenoids pulls together and elevates the mucosa overlying the muscular processes of the arytenoid cartilages.
The muscular tube of the pharynx is formed by two layers, the inner longitudinal layer and outer circular (constrictor) layer. The constrictor muscle layer (X) forms a ring that is incomplete anteriorly. During swallowing, the constrictor muscles contract sequentially to help propel the bolus into the esophagus. Contraction of the superior constrictor muscles also apposes the lateral pharyngeal wall to the soft palate, closing the lateral portion of the velopharyngeal portal. On a lateral view of the pharynx, the location of each paired constrictor muscle can be approximated by visible structures. The superior constrictor extends from the level of the soft palate toward the mid and lower base of the tongue. The lower portion of the middle constrictor angles superiorly from the level of the hyoid bone; the upper portion of the middle constrictor is about 1.5 vertebral bodies above the level of the hyoid bone. The upper border of the thyropharyngeal muscle is just above the continuation of a line of the hyoid bone posteriorly; the lowermost fibers extend to the level of redundant mucosa behind the cricoid cartilage. Redundant mucosa posterior to the posterior lamina of the cricoid cartilage identifies the location of the unpaired cricopharyngeal muscle (see Fig. 4.6 ).
The inner longitudinal muscle layer includes the stylopharyngeal muscle (IX), salpingopharyngeal muscle (X), and palatopharyngeal muscle (X). , During swallowing, contraction of the inner longitudinal muscles helps pull the pharynx up and over the descending food bolus. The palatopharyngeal muscle also constricts the posterior portion of the pharynx, channeling the bolus into the hypopharynx and helping prevent nasal regurgitation. Transfer of the bolus through the pharynx results from the pressure of the bolus itself (gravity); closure of the palatoglossal isthmus, velopharyngeal portal, and laryngeal aditus; tongue base retraction; elevation of the pharynx up over the bolus; and contraction of the constrictor muscles.
The pharyngoesophageal segment is tonically contracted at rest. Signals via the recurrent laryngeal nerve cause the cricopharyngeal muscle to relax. Elevation of the pharynx and larynx by the suprahyoid musculature, intrinsic pharyngeal elevators, and thyrohyoid muscle pull the anterior wall of the pharyngoesophageal segment (the postcricoid mucosa) superiorly and anteriorly. The weight of the bolus, tongue base retraction, and constrictor muscle contraction help open the pharyngoesophageal segment.
Swallowing begins with central nervous system (CNS) recognition of thirst or hunger and CNS-controlled movement of a bolus to the lips. The nerves of the mouth, tongue, pharynx, and larynx coordinate breathing and swallowing and adapt to the size and viscosity of the bolus. Swallowing itself occurs as a sequential contraction of skeletal muscles, preprogrammed in the brainstem swallowing centers and altered by sensory feedback from the oral cavity and pharynx. Portions of the trigeminal (V), facial (VII), glossopharyngeal (IX), vagus (X), accessory (XI), hypoglossal (XII), and first through third cervical nerves (via the ansa cervicalis) all participate in swallowing (see Table 4.1 ). Branches from the glossopharyngeal nerve and vagus nerve and branches from the sympathetic trunk and cervical ganglion form a plexus of nerves outside the constrictor muscle layer. The pharyngeal plexus has sympathetic and parasympathetic fibers intermingling with afferent and efferent branchial fibers that branch into the pharyngeal musculature. Pharyngeal sensation is mediated primarily by the glossopharyngeal (IX) cranial nerve.
Swallowing is divided into several phases: feeding followed by the oral, pharyngeal, and esophageal phases. This division is arbitrary as oral, pharyngeal, and esophageal motions occur simultaneously or overlap in a preprogrammed sequence of the brainstem swallowing centers. Nevertheless, compartmentalization of “phases” aids in radiographic analysis.
Swallowing begins with the urge to eat or drink. Food is carried by the hand or a utensil to the lips, and a beverage is swallowed directly or through a straw. Impairment of these swallowing acts accounts for the vast number of people who are unable to self-feed.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here