Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Multiple antenatal exposures exert effects on the fetal lung—some adverse and other beneficial for postnatal survival.
Antenatal exposures can alter lung development and interact with postnatal exposures.
Early gestational lung maturation is common and promoted by both antenatal steroids and fetal exposure to inflammation.
Antenatal steroid is a common exposure that may interact with postnatal care practices in presently unknown ways.
Sepsis with chorioamnionitis is an infrequent event in term and near-term infants.
Fetal exposure to inflammation/chorioamnionitis results in complex immunomodulation which may alter postnatal exposures.
Growth restriction, tobacco and alcohol alter fetal lung development with effects on post-delivery outcomes.
Lung growth and development are the substrates on which all lung outcomes ultimately depend. This chapter emphasizes four categories of events that can modulate fetal and subsequent postnatal lung development and thus alter lung outcomes for a lifetime ( Fig. 1.1 ). Antenatal corticosteroids as a potent antenatal intervention demonstrated to mature fetal lung are discussed elsewhere in this book. McElrath and colleagues propose that there are two pathologic pathways that result in deliveries at very early gestational age (GA): intrauterine inflammation that is often chronic and aberrations of placentation/vascular development. Other examples of clinically relevant modulators of lung development are small for gestational age/intrauterine growth restriction (SGA/IUGR) and environmental exposures such as maternal tobacco and alcohol use. Lung maturation is a late phase of lung development that can be accelerated by antenatal corticosteroids and by fetal exposure to inflammation. Although infection can induce lung maturation, fetal exposures to acute or chronic chorioamnionitis also can injure the lung. There are two “elephants in the room” for this discussion of events that influence lung development. The first is the concept of what is “normal.” Any discussion of premature lungs is complicated by the lack of a normal comparison group with which to evaluate the impact of the perinatal event of interest. Although the words all or never should be sparingly used in biology and medicine, all very low-birth-weight (VLBW) deliveries must be regarded as adverse pregnancy outcomes. The 24-week GA newborn who does not have respiratory distress syndrome (RDS) is a true wonder of nature.
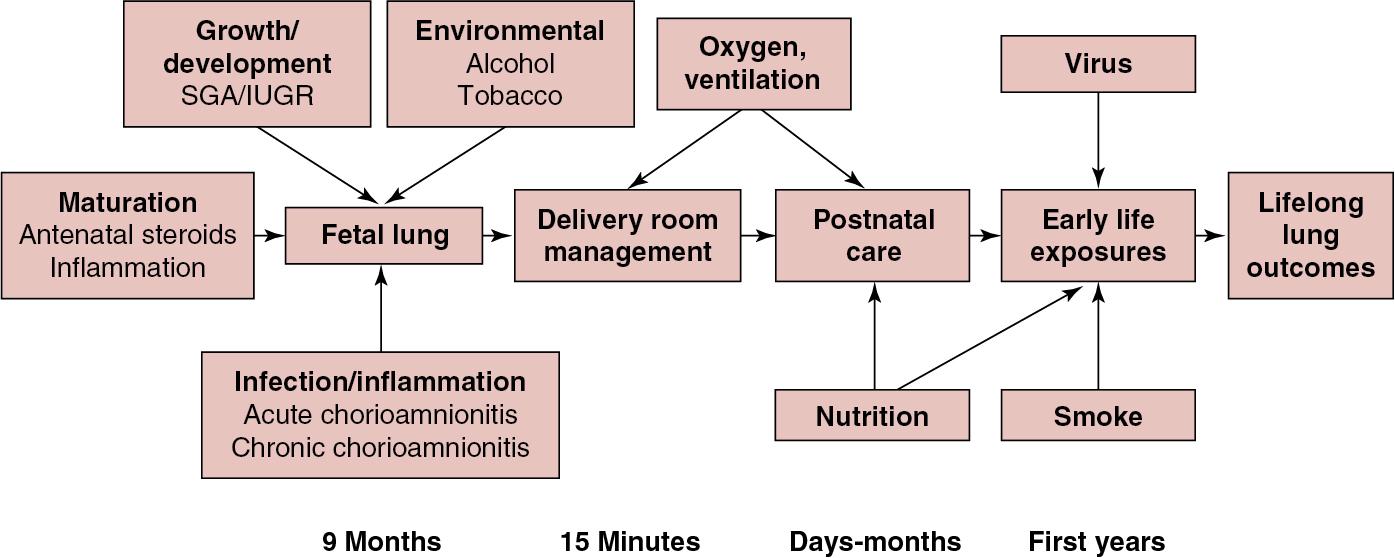
The second “elephant” is the complexity of the entangled pathways that regulate lung development, injury, and repair for any perinatal event that affects the lung. These three cellular and molecular response programs share signaling pathways that are superimposed simultaneously or sequentially on the immature lung. This complexity confounds simple interpretations about what mediator is causing which outcome. Finally, outcomes such as bronchopulmonary dysplasia (BPD) and asthma/airway disease in childhood and later life may be initiated by fetal events that then are modulated by postnatal responses of the lungs. An example is early life exposures to viral infections. This biologic complexity generates inconsistencies in clinical data and controversies. In this chapter, we provide our current understanding of how prenatal exposure to various conditions can change postnatal lung function based on both clinical information and animal models.
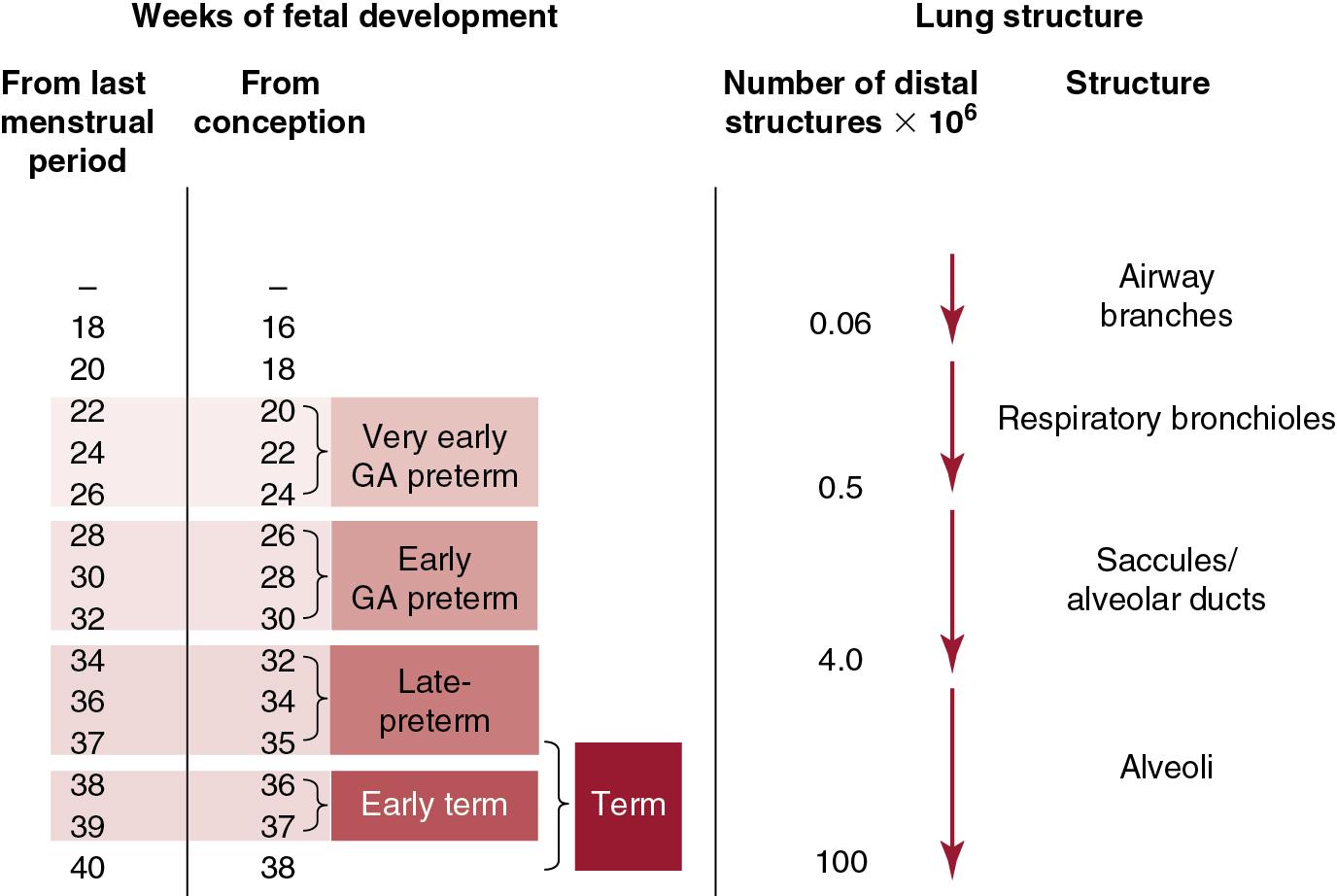
Lung development is programmed by the fetus to be sufficiently mature to adapt rapidly to air breathing at birth. The timing of the structural development of the lung in Fig. 1.2 is given as weeks from last menstrual period and from conception to emphasize the 2-week difference. Infants born by elective cesarean section as early term infants (38 weeks postmenstrual age) have more problems with pulmonary adaptation than infants born at 40 weeks postmenstrual age. Late preterm infants have more lung adaptation problems and more RDS for each week of birth prior to 37 weeks. Finally, lung adaptation abnormalities, RDS, and subsequently BPD become increasingly frequent as GA decreases into the early GA and very early GA categories of preterm infants. Lung development includes development of the structural elements as well as functional maturation of fluid clearance pathways and the surfactant system. The major structural events are the completion of airway branching by about 18 weeks of gestation, followed by three generations of airway divisions to form respiratory bronchioles, and three more divisions to form alveolar ducts to about 32 to 36 weeks. Subsequently, secondary septation or alveolarization occurs to term and for several years after birth. Septation events are dynamic with about 0.06 × 10 distal structures at 18 to 20 weeks that increase to about 100 × 10 alveoli at term—a 1700-fold increase. Alveolar numbers increase only about fivefold from the term birth lung to the adult lung. There is essentially no information about the variability of the timing of normal septation in the human lung. It is also not known whether very early lung maturation changes the timing of the later gestational septation events that generate respiratory bronchioles and alveolar ducts. Some forms of pulmonary hypoplasia may result from altered septation and airway development. The injury and repair associated with BPD do inhibit and delay alveolarization of the developing lung.
Recent human anatomic and experimental data demonstrate that the healthy lung probably grows new alveoli and loses old alveoli continuously at a very slow rate. , Empirically, very preterm infants with a BPD-associated “arrest” in alveolar septation must be able to grow alveoli or they could not grow and survive. These lungs may “catch up” to have lung volumes or alveolar numbers equivalent to normal lungs. The questions for the future include how alveoli grow after very preterm birth and how lung injury can be prevented.
From the clinical perspective, questions about lung maturation have focused on RDS and the surfactant system since the seminal report from Avery and Mead in 1959 that the lungs of infants who died of RDS had less surfactant. Lung maturation also includes epithelial development of ion/water regulation, thinning of the alveolar capillary barrier, and microvascular development. The first challenge is to define the timing of normal lung maturation, which is not an easy task if one assumes that most preterm infants are abnormal. In the 1970s, amniotic fluid was sampled from women with relatively normal gestations to test for lung maturation using surfactant components. The lecithin/sphingomyelin (L/S) ratio was less than 2 until after 34 to 35 weeks of gestation, and phosphatidylglycerol was seldom detected prior to 34 weeks of gestation in normal pregnancies. The true time course and the variability for the timing for normal lung maturation are not known with any precision for the human. However, lung maturity testing and inadvertent experiences with nonindicated cesarean sections prior to 37 weeks demonstrate that lung maturation, defined as absence of RDS, normally occurs after about 34 to 36 weeks in normal pregnancies.
The diagnosis of RDS for very early GA preterm infants has been confounded in clinical series and epidemiologic studies by intubation and ventilation with or without surfactant treatment shortly after birth. These intubated and ventilated infants likely carry the diagnosis RDS even if they are not receiving supplemental oxygen. Furthermore, if these infants have infection, transient tachypnea of the newborn, a degree of pulmonary hypoplasia, or apnea requiring ventilatory support, they likely will be said to have RDS. The successful use of continuous positive airway pressure (CPAP) to minimize lung injury in very early GA infants demonstrates that many very preterm infants do not have enough RDS to need surfactant or mechanical ventilation. Infants born at 24 to 25 weeks of GA without RDS are surprisingly common. Because lung maturation (and RDS) is a continuum from severe immaturity to sufficient maturation to avoid RDS, we think that most very preterm infants have some degree of induced lung maturation. The infant born at 24 to 26 weeks of gestation with severe respiratory failure and a poor response to surfactant and who dies soon after birth is an infant with “normal” 25-week lungs or an infant with RDS-plus (RDS plus infection or pulmonary hypoplasia, for example). Very few infants die of RDS in the United States unless they are of extremely low GA.
At the margin of lung maturity in preterm sheep, a surfactant pool size of about 4 mg/kg is sufficient to support normal gas exchange with CPAP, demonstrating that a small amount of surfactant is sufficient to protect the preterm lung from RDS. We have no good tests to quantify the lung maturation status prior to or soon after delivery. The L/S ratio or phosphatidylglycerol measurements in amniotic fluid are no longer commonly available, and other tests such as lamellar body number in amniotic fluid are imprecise. Samples of fetal lung fluid (intubated infants) or gastric aspirates soon after birth could provide information about surfactant and inflammation, but they are not used routinely. An evaluation of the messenger RNA (mRNA) in amniotic fluid may provide a maturation profile for multiple fetal organs in the future. A clinical controversy is: Which very preterm infant should receive surfactant/ventilation or CPAP after birth? The controversy is based on the perceived risk for RDS and the ability of these infants to transition if treated by CPAP. The clinical trials demonstrate that the two approaches yield similar outcomes that marginally favor an initial trial of CPAP. However, individualized treatments could be given if the functional potential of the very preterm lung could be assessed prior to delivery. Clearly, very preterm delivery is an event that profoundly changes the developing lung. However, there is no good information about how preterm delivery and breathing, independent of oxygen exposure and injury, change the trajectory of subsequent lung development. Lung stretch from breathing and the striking changes in hormone milieu alter lung development in experimental models. , The implication is that independent of injury, lung structure at 40 weeks will be different for infants born at 25 weeks or 35 weeks from those for infants born at 40 weeks.
The human fetus is normally considered to be in an environment protected from infection. However, the human fetus can be exposed to a variety of pathogens, which may initiate an inflammatory process in the placenta, chorioamnion, or fetus. For example, human fetuses are exposed to viral pathogens as a consequence of maternal viremia. The patterns of injury to agents such as varicella and cytomegalovirus depend on the period of gestation during which the infection occurs. Similarly, the fetus can acquire a spirochete infection with syphilis or a parasitic infection with toxoplasmosis secondary to maternal infection, and each causes characteristic syndromes depending on the gestational timing of exposure. These infections are not generally viewed as predominantly inflammatory, although the fetal injury and immune responses have inflammatory characteristics. Asphyxia with injury to fetal tissue also causes inflammation as part of the injury and the repair process. Similarly, normal labor is associated with an increase in proinflammatory mediators. Both innate and acquired inflammatory responses of the fetus are generally considered to be less robust than those in the child or adult because the response systems in the fetus are immature and pregnancy is an immune-suppressive environment. For example, fetal inflammatory responses to pathogens such as group B streptococcus and Listeria monocytogenes are blunted, resulting in severe infection and often death of the fetus or newborn. The most common fetal infectious exposure is to chorioamnionitis, which is associated with preterm labor and delivery. In this section, we identify the questions and controversies about the associations of chorioamnionitis with a range of effects on the fetal and newborn lung.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here