Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Ultrasound is the modality of choice for the initial imaging assessment of the female pelvis in most settings. This chapter focuses on the sonographic evaluation of the pelvis, with particular attention to the uterus. Chapter 24 covers the ultrasound examination of the ovaries and adnexa.
Transabdominal (TA) and transvaginal (TV) ultrasound are the most commonly used approaches for performing pelvic ultrasound. The TA and TV scanning approaches are complementary, each with distinct strengths and weaknesses. Either TA or TV sonography can be performed initially. The decision as to whether to use both scanning techniques will depend on the clinical setting and findings on the initial scan. Often both TA and TV evaluation are used, which is not surprising given that these studies are complementary. In many practices TV evaluation is not performed in patients who have never been sexually active.
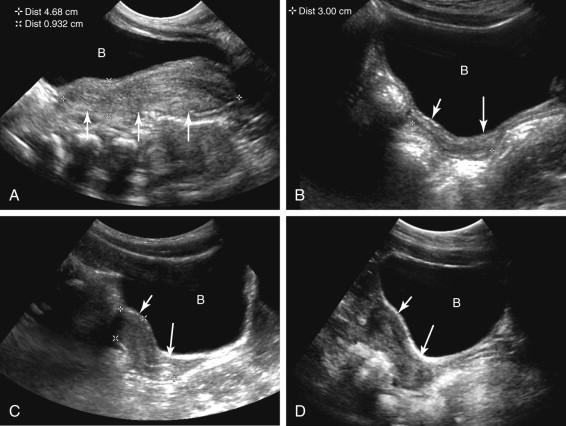
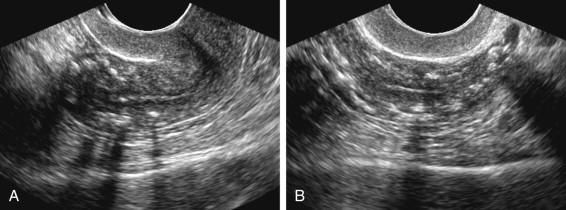
The TA examination is performed with the transducer on the anterior abdominal wall at the level of the pelvis. A distended urinary bladder aids in visualization of pelvic structures at TA ultrasound, displacing gas-filled bowel loops out of the field of view and providing a sonographic window for scanning. Depending on body habitus and distribution of bowel gas, a full bladder may not be necessary to adequately visualize pelvic structures transabdominally. TA images provide a more complete overview of the pelvis than TV ultrasound, facilitating visualization of anatomy and detection of pathology located beyond the field of view of the TV probe ( Fig. 23-1 ).
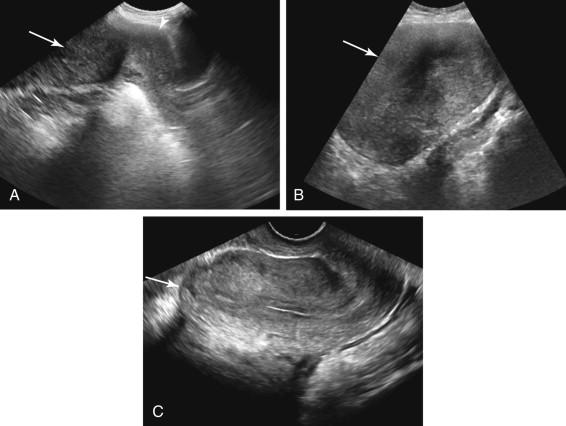
The TV examination is generally performed with the patient's bladder empty. Because the transducer is closer to the pelvic organs than at TA ultrasound, higher scanning frequencies are used. As a result, TV images generally provide superior resolution, improved characterization of pelvic structures, and detection of pathology too small to be seen at TA ultrasound ( Fig. 23-2 ). Despite this, one of the weaknesses of TV scanning is that the intracavitary position of the TV probe limits movement of the transducer. In addition, the higher transducer frequencies do not penetrate as far as the lower frequencies used during TA scanning, resulting in a smaller field of view. Findings farther away from the transducer may go undetected at TV ultrasound.
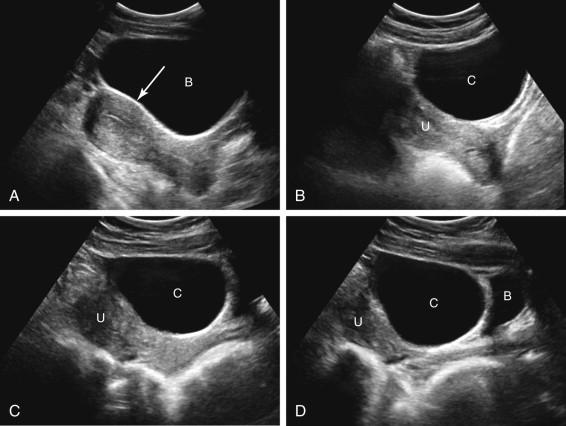
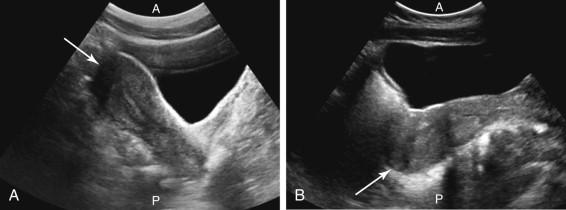
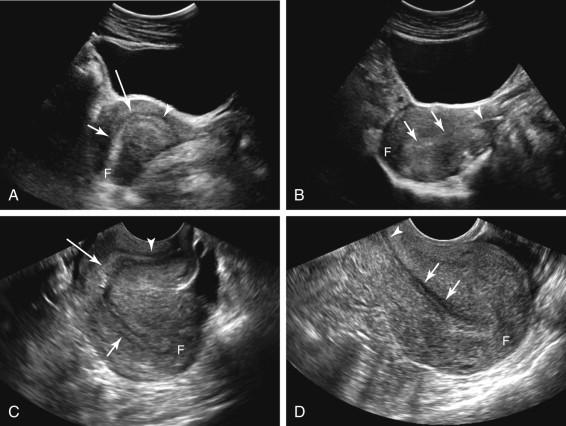
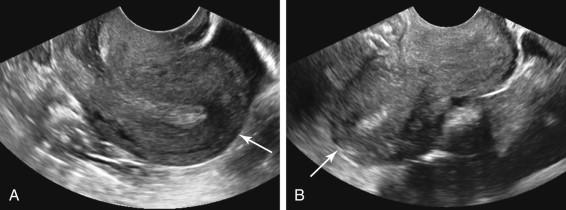
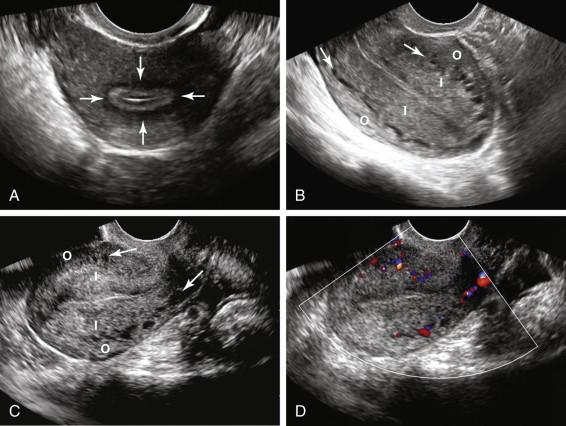
It is important to definitively identify the urinary bladder during TA scanning to avoid mistaking a midline cystic ovarian mass interposed between the uterus and abdominal wall for the bladder. Bladder shape can be helpful in distinguishing these possibilities. A distended urinary bladder typically has an elongated or pear-shaped configuration on midline sagittal scans, with a distinct posterior impression from the uterus, whereas a cystic ovarian mass exhibits a more rounded contour ( Fig. 23-3A and B ). If there is any question as to whether a cystic structure in the pelvis represents the urinary bladder, the identity of the bladder should be confirmed by emptying or filling it (see Fig. 23-3C and D ).
The ACR-ACOG-AIUM-SPR-SRU Practice Parameter for the Performance of Ultrasound of the Female Pelvis indicates that evaluation of the uterus should include the size, shape, and orientation of the uterus, as well as assessment of the endometrium, myometrium, and cervix. The uterus is divided into two main parts, the cervix and the body. The fundus is the portion of the uterine body located along the upper surface of the uterus, between the insertions of the fallopian tubes. The body of the uterus contains endometrium centrally, myometrium peripheral to the endometrium, and serosa along the outer surface of the uterus.
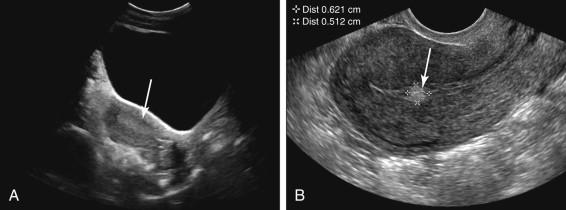
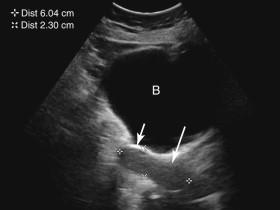
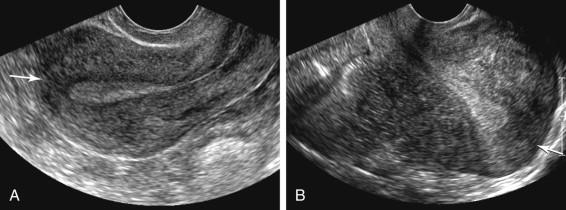
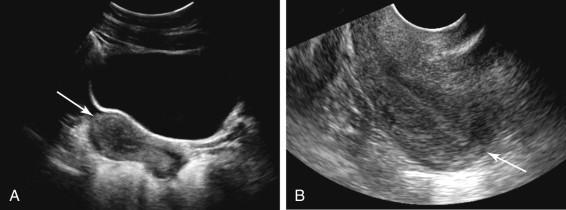
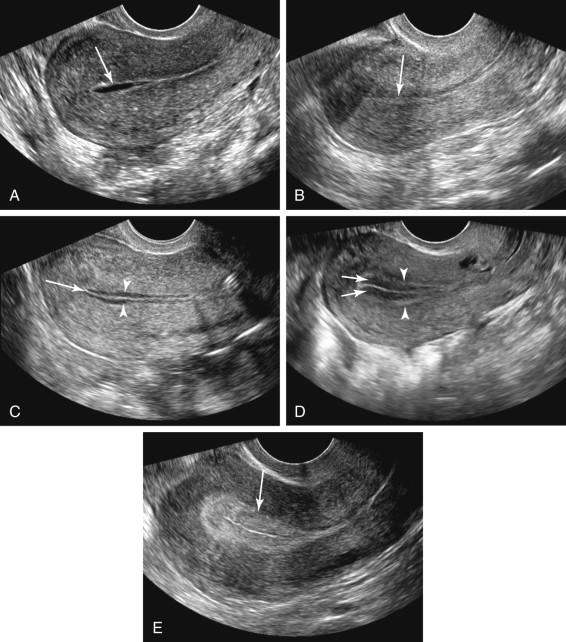
The vagina is identified on a midline sagittal TA scan as an echogenic line surrounded by hypoechoic tissue ( Fig. 23-4A ). A tampon in the vagina is depicted as a thick, linear, hyperechoic structure with dense shadowing due to air (see Fig. 23-4B ).
Uterine size and shape varies with patient age, menstrual status, and pregnancy history. The neonatal uterus is prominent for several weeks after birth, secondary to maternal hormones ( Fig. 23-5A ). After the hormonal effects subside, the uterus decreases in size. During the prepubertal years the cervix is similar in size or more prominent than the uterine body and fundus, resulting in an elongated or a tubular configuration of the uterus (see Fig. 23-5B ). The uterus remains small until the reproductive period approaches, beginning at approximately 8 years of age. At that time the uterus begins to enlarge and the body and fundus increase in prominence relative to the cervix (see Fig. 23-5C ). The uterus reaches its adult size and configuration several years following menarche (see Fig. 23-5D ).
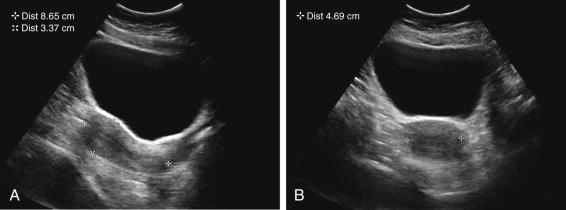
During the reproductive years the uterine body and fundus are considerably larger than the cervix. Uterine length is measured from the top of the fundus to the bottom of the cervix (optimally to the external cervical os) in the sagittal scan plane. The anteroposterior (AP) measurement is obtained perpendicular to the longitudinal plane, usually on the same image as the longitudinal measurement ( Fig. 23-6 ). Width can be obtained on either a coronal or transverse view. The normal nulliparous adult uterus measures up to 8 cm × 4 cm × 5 cm in length, AP dimension, and width, respectively. Uterine size is often larger in patients with a history of pregnancy, increasing approximately 1 cm following the first pregnancy and measuring up to 2 cm larger than a nulliparous uterus in a multiparous woman.
Menopause is defined as beginning 1 year after cessation of menses. The uterus atrophies following menopause, progressively decreasing in size, particularly during the first decade after menopause. The disproportion in size of the uterine body relative to the cervix typical of the reproductive years also diminishes ( Fig. 23-7 ).
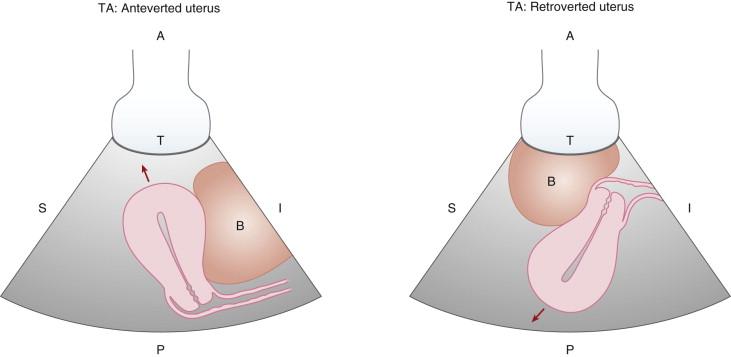
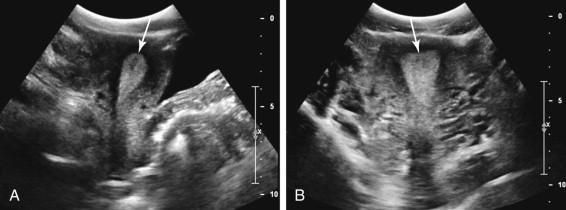
The practice parameter for pelvic ultrasound indicates that uterine orientation should be documented. Orientation can be important when procedures such as intrauterine device (IUD) placement or dilatation and curettage are performed. The terms anteverted, anteflexed, retroverted, and retroflexed are commonly used to describe uterine orientation. On TA ultrasound, the fundus of an ante verted or ante flexed uterus points toward the ante rior portion of the pelvis (the top of the image on a TA scan), whereas the fundus of a retroverted or retroflexed uterus points toward the posterior portion of the pelvis (the bottom of the image on a TA scan) ( Figs. 23-8 and 23-9 ).
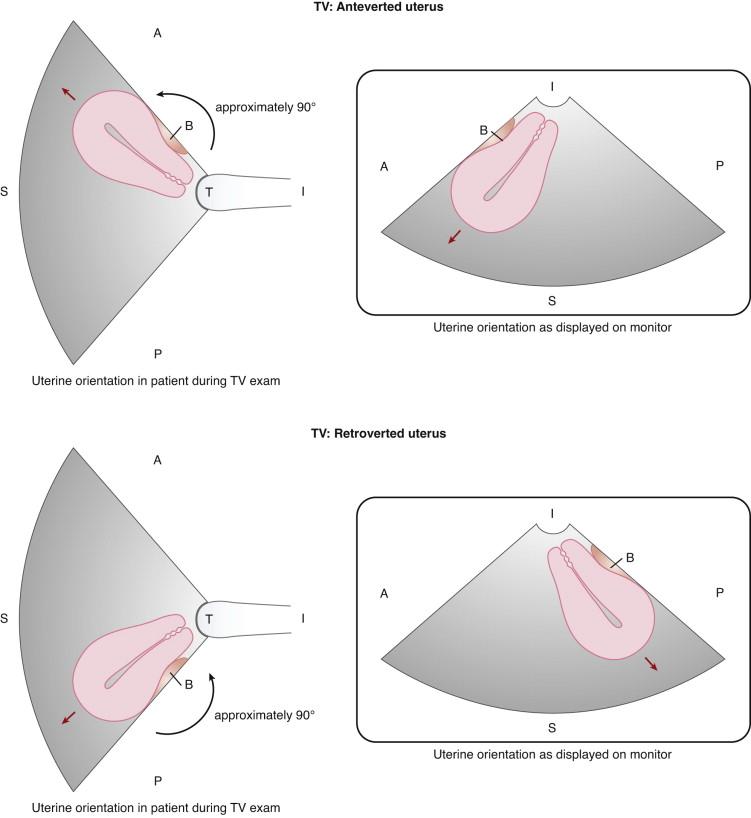
Depiction of uterine orientation is different on TV and TA scans because the TV transducer is positioned in the vagina rather than on the surface of the abdominal wall. By convention the portion of the ultrasound image located closest to the transducer is displayed at the top of the image; therefore when the TV image is viewed on the ultrasound monitor it has been rotated approximately 90 degrees from the TA orientation. As a result, the fundus of an anteverted or anteflexed uterus points toward the left side of the image and the fundus of a retro verted or retro flexed uterus points toward the r ight side of the image (remember: r etropositioned uterus points to the r ight on TV ultrasound) ( Figs. 23-10 and 23-11 ). Occasionally the uterine fundus is horizontal in orientation on TA images (not pointing significantly anteriorly or posteriorly) and vertical in orientation on TV images (not pointing significantly to the left or right). This orientation has been termed neutral , axial , or midpositioned.
The suffix v erted describes the orientation of the cervix relative to the axis of the v agina and flexed describes the orientation of the uterine body relative to the cervix ( Fig. 23-12 ). An easy way to remember this is that flex ed describes the presence of a flex ion, bend, or curve between the cervix and uterine body (see Fig. 23-12A and C ). In contrast, when the retropositioned uterine orientation is entirely due to a retroverted uterus, there is no flexion, bend, or curve between the cervix and uterine body (see Fig. 23-12B and D ). The difference between a retroflexed and retroverted uterus tends to be easiest to recognize at TA ultrasound due to the overview of the pelvis provided by the TA approach, often demonstrating the entire uterus including the fundus and the cervix on a single field of view. Despite this, a retroflexed uterus can be diagnosed on TV ultrasound when the fundus points to the right side of the image and the uterine body is folded up (flexed) against the cervix (see Fig. 23-12C ). If instead there is no significant flexion, bend, or curve between the uterine cervix and body, the orientation of the uterus is attributable to the angle of the cervix relative to the vagina and the suffix verted is applied (see Fig. 23-12B and D ). If the uterus is not seen adequately enough to distinguish whether it is retroverted or retroflexed, uterine orientation may be described as retropositioned. In most cases a single term is sufficient to describe uterine orientation, but occasionally it may be helpful to use a combination of terms (e.g., anteverted and retroflexed); ( Fig. 23-13 ).

In the majority of patients the orientation of the uterus is consistent on TA and TV imaging. Occasionally, however, uterine orientation is different on the TA and TV examination ( Fig. 23-14 ). Less commonly, uterine orientation changes during the course of a single TV examination ( Fig. 23-15 ). These variations are attributable to the effects of bladder distention and transducer pressure on uterine orientation.
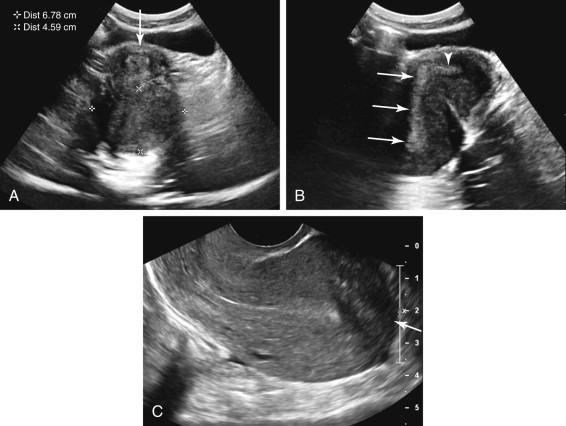
The endometrium of a retroflexed uterus may be difficult to image at TA ultrasound because it is oriented approximately parallel to the ultrasound beam. Failure to visualize the endometrium can result in the spurious impression of a posterior fibroid ( Fig. 23-16 ). By adjusting the orientation of the transducer, the normal endometrium can frequently be better appreciated, distinguishing a retroflexed uterus from a fibroid. TV ultrasound also can resolve this pitfall, confirming both the retroflexed orientation of the uterus and the absence of a corresponding fibroid.
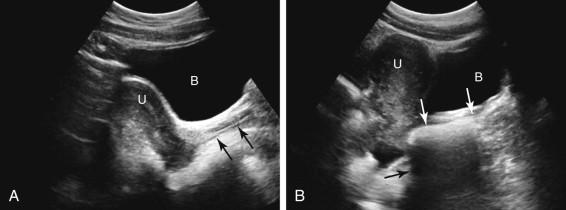
Endometrial thickness is measured in AP diameter on a midline sagittal image, perpendicular to the long axis of the endometrium ( Fig. 23-17 ). The thickest portion of the endometrium should be measured. When both TA and TV ultrasound are performed, TV measurements should be used. Care should be taken to ensure that the true AP dimension of the endometrium is measured, because the endometrium is considerably thicker in width than in AP dimension. Coronal or oblique measurements may give the spurious impression of a thick endometrium ( Fig. 23-18 ). Although fluid within the endometrial canal should be described, it should not be included in the measurement of endometrial thickness. Instead, the endometrial thickness reported should include both layers of endometrium on either side of the fluid, excluding the fluid in the endometrial cavity ( Fig. 23-19 ).


The endometrium is the inner layer of the uterus and is composed of a central functional layer, which is shed monthly during menses, and a peripheral basal layer. The sonographic appearance and thickness of the endometrium vary with the menstrual cycle ( Fig. 23-20 ). A small amount of fluid in the endometrium is considered a normal finding during menstruation. Near the end of menstruation, the endometrium is depicted as a discrete, thin, hyperechoic line measuring up to approximately 4 mm. During the proliferative phase of the menstrual cycle, between cessation of menstruation and ovulation, the endometrium thickens, measuring up to approximately 8 mm, and the functional layer becomes hypoechoic due to the effects of estrogen. In the late proliferative/periovulatory period, the endometrium measures up to approximately 11 mm and exhibits a multilayered appearance composed of a thin, central echogenic line corresponding to the interface of tissue on either side of the endometrial cavity, surrounded by a hypoechoic functional layer, and a hyperechoic outer layer corresponding to the basal layer of endometrium. The secretory phase of the cycle occurs following ovulation and is associated with further thickening and increased echogenicity of the functional layer of the endometrium due to the effects of progesterone. This results in a homogeneously echogenic endometrium measuring up to 15 to 16 mm. As menses begins, the functional layer of the endometrium sloughs, the endometrium thins, and the cycle starts again.
The myometrium is composed of three layers ( Fig. 23-21 ). A compact hypoechoic central layer that has been termed the subendometrial halo surrounds the endometrium and corresponds to the junctional zone on magnetic resonance imaging (MRI). This layer is inconsistently visualized at ultrasound, and when seen, should not be included in measurements of endometrial thickness. The intermediate layer is located between the junctional zone centrally and the arcuate blood vessels peripherally and is the thickest component of the myometrium, largely accounting for the shape of the uterus. The arcuate blood vessels are located just inside the thin outer layer of myometrium in a circumferential distribution. Arcuate artery calcifications are frequently seen in older and diabetic women, and can be distinguished from calcified fibroids by their characteristic circumferential distribution immediately inside the outer layer of myometrium ( Fig. 23-22 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here