Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Approximately 1% to 10% of all births in the United States are complicated by chorioamnionitis, but the incidence varies significantly by study population, gestational age at presentation, and diagnostic criteria. Histologic chorioamnionitis is a pathologic term that refers to an influx of maternal inflammatory cells (neutrophils, macrophages, and T cells) into the placental membranes. The term clinical chorioamnionitis is used when overt signs of intraamniotic infection—such as maternal fever, leukocytosis, and uterine tenderness—are present. Although histologic and clinical chorioamnionitis frequently occur together in response to invading microorganisms, histologic chorioamnionitis is three times more common. It is therefore possible to have pathologically significant inflammatory lesions in the placenta with no intrapartum clinical signs and a negative amniotic fluid culture. Furthermore, only about two-thirds of women with suspected clinical chorioamnionitis have histologic evidence of placental inflammation. A recent update to clinical guidelines issued by the American College of Obstetrics and Gynecology acknowledges the potential gaps between isolated maternal fever, suspected intraamniotic infection (maternal fever with one or more additional signs of chorioamnionitis), and confirmed intraamniotic infection (confirmation is achieved by laboratory testing of the amniotic fluid). Invading pathogens differ in their ability to induce a host inflammatory response; some organisms cause a more chronic subclinical infection, whereas others induce a robust, clinically apparent inflammatory syndrome. Intrauterine infection and/or inflammation (III) is sometimes used as an alternative diagnostic term to more precisely describe the clinical spectrum of chorioamnionitis.
Intrauterine infections are almost always polymicrobial and often involve fastidious organisms, making culture-based identification unreliable. The use of molecular-based techniques for microbial detection, most notably broad-range16s rDNA polymerase chain reaction (PCR), has provided a more accurate estimate of the frequency of microbial invasion of the amniotic cavity and may explain some of the disparity in the reported frequencies of clinical infection versus histologic inflammation. Although the presence of microbial DNA in amniotic fluid has been associated with increased proinflammatory signaling and adverse pregnancy outcomes, data obtained using these highly sensitive detection methods raise the question of whether the presence of microbes in the intrauterine space is always pathogenic.
Invading pathogens most frequently access the intrauterine cavity by ascending through the cervix from the lower genital tract. Organisms may also gain entry via hematogenous transmission through the placenta, retrograde migration from the abdominal cavity through the fallopian tubes, and iatrogenic introduction during amniocentesis or chorionic villus sampling. This chapter reviews what is known about the anatomic and immunologic barriers that function to protect the developing fetus from intrauterine pathogens along each of these routes of infection and the microbial virulence mechanisms that have evolved to escape these host defenses. The specific fetal and maternal inflammatory responses to intrauterine infection are discussed in detail in Chapter 12.
The vast majority of intrauterine infections are caused by bacteria that first colonize or invade the vaginal epithelium and then ascend through the cervix into the upper genital tract. Therefore the epithelial cells of vaginal mucosa serve as the first line of defense, functioning as a physical barrier that inhibits the passage of pathogens to underlying tissues. In addition, the vaginal epithelium is coated with a thin layer of mucus that not only traps infectious agents but also contains immunoglobulin (Ig) and several antimicrobial peptides (AMPs), including defensins, secretory leukocyte protease inhibitor, calprotectin, lysozyme, and lacteroferrin. Finally, vaginal epithelial cells express several Toll-like receptors (TLRs) and therefore are capable of sensing and rapidly responding to a wide spectrum of pathogens.
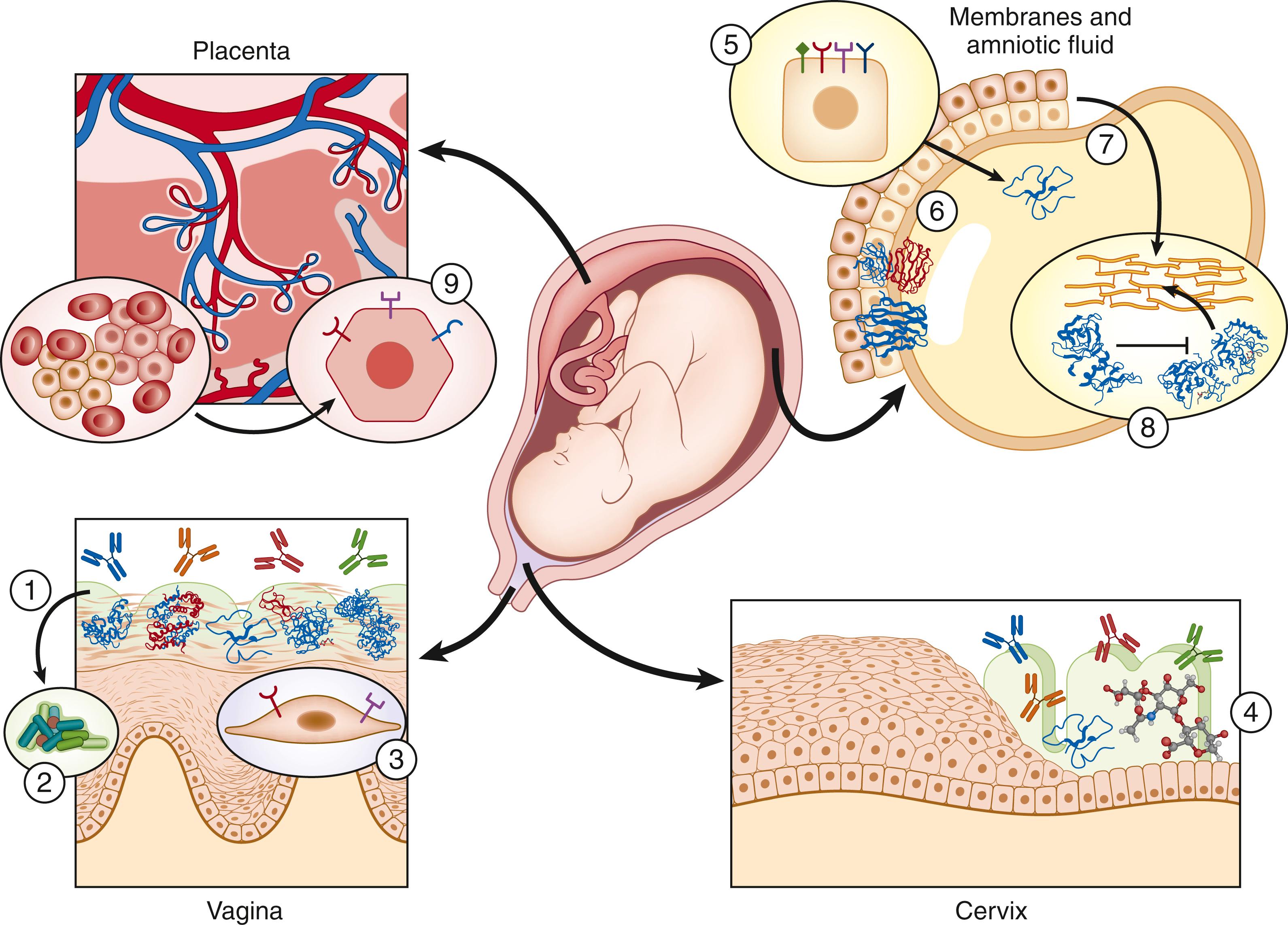
The microbial inhabitants of the female genital tract play a critical role in maintaining reproductive health. It has long been recognized that Lactobacillus spp. are the dominant members of the vaginal microbiota ; when these organisms are diminished in number or absent, the risk of acquiring urogenital infections increases. Lactobacilli protect against colonization and overgrowth of potentially pathogenic organisms through numerous mechanisms. They compete for nutrients and receptors at the epithelial surface and produce a variety of antimicrobial substances, including lactic acid (which maintains the vaginal tract at an acidic pH), bacteriocins, and hydrogen peroxide. In addition, vaginal lactobacilli are capable of modulating innate immune responses in the female genital tract via the production of TLR ligands and short-chain fatty acids. , For example, exposure of a multilayer vaginal epithelial cell culture to lactobacilli significantly reduced proinflammatory cytokine secretion in an isolate-specific fashion following TLR stimulation. Although there are ample in vitro data supporting the role of Lactobacillus spp. in maintaining vaginal health, there are conflicting data as to which of these antimicrobial mechanisms are most relevant in vivo. ,
Although both the composition and stability of the vaginal microbiota is altered during pregnancy, Lactobacillus species remain the dominant constituents. A Lactobacillus -dominant vaginal microbiota is associated with a reduced incidence of miscarriage, chorioamnionitis, and preterm delivery. These observations have prompted numerous clinical trials investigating the potential preventative and/or therapeutic effects of administering lactobacilli-containing probiotics during pregnancy. However, the data thus far are insufficient to incorporate this into clinical practice. Of note, not all Lactobacillus spp. may be regarded as beneficial; L . iners , in particular, may destabilize the microbiota, predisposing to colonization with potentially pathogenic organisms during pregnancy and may be an independent risk factor for preterm birth.
Bacterial vaginosis (BV) is a dysbiosis characterized by a loss of lactobacilli and overgrowth of other anaerobic microbes including Gardnerella vaginalis , Bacteroides spp., Mobiluncus spp., Peptostreptococcus spp., and Mycoplasma hominis . BV is a known risk factor for preterm delivery and miscarriage. , However, the physiologic mechanisms by which BV leads to adverse pregnancy outcomes remain poorly understood. It is possible that replacement of the Lactobacillus -dominated microbial community with an overgrowth of BV-associated organisms stimulates a local or systemic inflammatory response that ultimately reaches the intrauterine environment. Although increases in local cytokine concentrations have been documented during BV, several studies have shown that circulating levels of serum cytokines remain unchanged. BV has been associated with endometritis, , which may in itself predispose to early pregnancy loss or subsequent intrauterine infection. It is plausible that the direct ascension of BV-associated bacteria into the intrauterine space may be responsible for observed pregnancy complications. , A 2015 study of otherwise healthy nonpregnant women (without BV) undergoing hysterectomy demonstrated that the upper genital tract is routinely colonized with vaginal species that generally do not elicit a strong proinflammatory response. , Hillier and colleagues reported that BV was significantly associated with the isolation of microorganisms from the chorioamnion. DiGiulio and colleagues, using both standard culture and broad-range PCR to analyze the amniotic fluid of women in spontaneous preterm labor with intact membranes, documented the presence of G . vaginalis and other BV-associated organisms.
Aerobic vaginitis (AV) is another type of vaginal dysbiosis in which there is a decreased abundance of lactobacilli and a predominance of aerobic microflora composed largely of enteric commensals or pathogens (e.g., Escherichia coli , Staphylococcus aureus , and group B Streptococcus [GBS]). In contrast to BV, AV is characterized by the presence of toxic-appearing leukocytes and parabasal cells, which are considered to be indicative of severe epithelial inflammation. This robust local inflammatory response is associated with significantly increased interleukin (IL)-6 and IL-1β concentrations in vaginal fluid. Given that many of these enteric organisms are often associated with chorioamnionitis, it is not surprising that some investigators have demonstrated an association between a diagnosis of AV during the first trimester of pregnancy and an increased risk of preterm birth, chorioamnionitis, and fetal funisitis. ,
Because of the consistent association of these vaginal dysbioses (BV and AV) with adverse pregnancy outcomes, some hypothesize that the risk of ascending infection and preterm birth is secondary to the absence of lactobacilli rather than to the presence of other potentially pathogenic microorganisms. , However, investigations using non–culture based methodologies are not supportive of this hypothesis. Romero and colleagues demonstrated that there were no differences in the relative abundance of microbial phylotypes between women who had a spontaneous preterm delivery and those who delivered at term. Furthermore, in both of these patient groups, the composition of the vaginal microbiota during pregnancy changes as a function of gestational age, with an increase in the relative abundance of Lactobacillus species as gestation advances. Data from another study suggest that the composition of intestinal, rather than vaginal, microbiota is associated with the likelihood for preterm delivery. This is an interesting finding, given the extensive remodeling of the intestinal microbiota that is reported to occur during the course of pregnancy. Our overall understanding of the impact of the human microbiota on pregnancy outcome is clearly in its infancy, and this topic represents fertile ground for future research.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here