Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
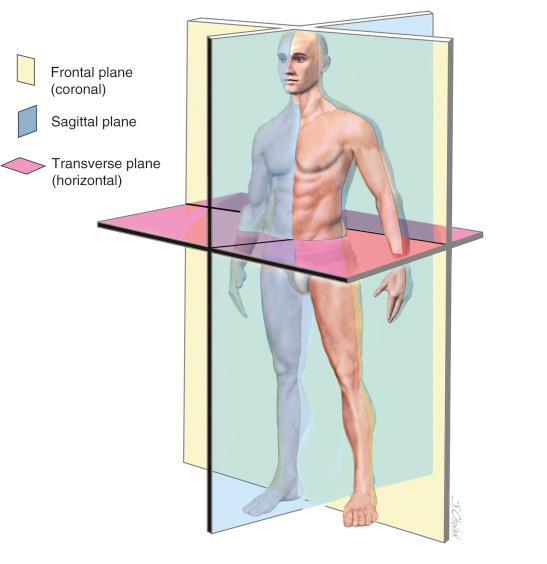
The geometry of bones is normally viewed in the three cardinal planes: frontal (coronal), sagittal, and transverse (horizontal, Fig. 36-1 ). The mechanical axis of the lower extremity from the femoral head center to the talus center (sometimes referred to as the hip-knee-ankle [HKA] axis) needs to be viewed in each of the three planes to define alignment. In the frontal plane, angular deviations from the normal straight line are referred to as varus-valgus, in the sagittal plane as flexion-extension, and in the horizontal plane as anteversion-retroversion (or antetorsion-retrotorsion). Just as varus or valgus deformity observed in the frontal plane causes abnormal joint loading, excess anteversion or retroversion observed in the horizontal plane causes abnormal joint loading.
Anterior knee pain, patellar instability, and patellar arthritis/chondromalacia are three different conditions that may be causally related to an abnormal limb alignment in the transverse plane. This chapter reviews the concept of torsional malalignment of the lower limb and its effect on the patellofemoral (PF) joint.
Limb alignment determines where and in what direction the tibiofemoral joint and patellofemoral joint (PFJ) are loaded. The geometry of the skeleton determines the direction of the load application on the PFJ. The PF ligaments acting against the patella in the trochlea are responsible for stability. Articular cartilage reduces friction to conserve energy and to transmit the force generated by a combination of body mass, momentum, gravity, and muscles. The musculotendinous units move the skeleton, stop it from moving, or hold it against gravity but are not normally responsible for preventing joint dislocation or subluxation. The total load depends on a variety of variables, including body mass, muscle activity, gravity, lever arm length, rate and direction of body motion, and so on. Femoral and tibial torsion both alter the position of the trochlea in space, thus where PF forces are centered. These forces may be changed by rotational osteotomy of the femur or tibia.
“Does Lower Limb Torsion Matter?” was the title of a keynote address at the 2012 European Society of Sports Traumatology, Knee Surgery and Arthroscopy (ESSKA) meeting. The question importantly opens the door to a multitude of related queries. What is torsion? What is rotation? How is torsion measured? Is there validity to the torsion measurement? What is normal torsion? What is the mechanical effect of altered torsion? Does abnormal torsion cause symptoms? Does abnormal torsion cause pathology? Where is abnormal torsion located? Are femoral and tibial torsions equally important? Are femoral and tibial torsions compensatory? Can abnormal torsion be corrected? Are femoral and tibial torsions the only causes of abnormal limb torsion? Is corrective osteotomy beneficial? There are an endless variety of additional questions, none of which has been adequately studied.
Maquet, in his masterpiece Biomechanics of the Knee , drew a strong relationship between the location of the resultant vector sum of all of the forces that produce knee joint loading and the location of the mechanical axis. Although he is often remembered for his anterior displacement osteotomy of the tibial tuberosity, Maquet emphasized an understanding of limb alignment in the coronal plan. Missing from the complete picture has been a similar analysis of the forces as seen in the transverse or horizontal plane.
The term miserable malalignment was apparently first introduced by Stan James. His classic description of limb maltorsion is highly recommended reading.
The essence of this chapter is that during normal gait, the knee joint axis moves forward in the direction the body is moving. When the knee joint axis is twisted away from the direction the body is moving, the loading vectors are directed obliquely, resulting in abnormal PFJ shear forces. This is common with abnormal torsion of either the femur or the tibia. For example, a patella dislocates when the combined stabilizing elements of trochlear geometry and PF ligaments are overcome by an excessive dislocating force. The excessive dislocating force is often caused by a knee joint pointing inward because of abnormal femoral anteversion or abnormal increase in external tibial torsion. Corrective osteotomy has no effect on the trochlear geometry or the integrity of the PF ligaments, but it does change the displacement force.
Normal alignment is presumed to be normal because it is the optimal limb geometry for the transfer of the body mass to the ground. Abnormal geometry results in unusual force transmissions through the PF joint during gait. It is rare to see published PF clinical studies that have reviewed limb alignment adequately. The precise variation from the normal skeleton is generally not specified, ranges of motion of all joints in all planes of the lower extremity have not been adequately recorded, and ligamentous stability is not measured.
The literature on patellar malalignment is quite confusing because many terms are commonly interchanged and not precisely defined. John Insall in 1976 defined patellar malalignment as being either an increased Q-angle or a high-riding patella. No other options were considered. In addition, he observed that “an increased Q-angle is usually associated with increased femoral anteversion and external tibial torsion. In the presence of these abnormalities, when the hip and ankle joints are normally aligned, the patella faces inward and motion of the knee occurs about an axis that is rotated medially compared with the axes of the hip and ankle joints.” He then recommended a medial tibial tubercle transfer or “patellar realignment” to treat this torsional malalignment, and it is no surprise that he reported that 61% of the patients remained symptomatic. Clearly the underlying pathoanatomy had not been measured nor addressed. Subsequent biomechanic studies suggest the recommended treatment is inappropriate. Tibial tubercle transfer has been shown to cause external rotation of the tibia on the femur rather than pull the patella medially into the trochlea and has been shown to increase medial compartment loading and medial facet loading. I believe the terms patellar malalignment and patellar realignment lack precise definition and therefore should never be used. The term malalignment should refer only to a limb that deviates from a neutral (normal) mechanical axis, and the deviation must be defined in each plane. Skeletal alignment is a direct result of the shape of the bones in the limb, but limb malalignment may also be caused by a joint with acquired cartilage or ligament loss.
More than 50 different factors have been associated with anterior knee pain, chondromalacia patellae, patellar instability, or patellar malalignment ( Table 36-1 ). Although these factors may be very important, objective measurement tools are lacking. No study has ever tried to assess all of these variables in a single cohort of patients, and even if this were undertaken, the lack of objective measurement techniques would make the study invalid. If these variables are indeed important, then any study would need to incorporate accurate measurements of each. The relative importance of each needs to be developed. Without this, clinicians are left with a realization that data do not exist to guide in the knowledge of pathomechanics, diagnosis, and treatment and that we depend only on unrelated clinical observations and some very basic laboratory studies. Thus, the complete validation of the importance of limb torsion in contributing to PF pain and dysfunction may always be challenged.
| Genu valgum | Genu varum |
| Femoral anteversion | Femoral retroversion |
| Excess external tibial torsion | Excessive internal tibial torsion |
| Outerbridge ridge | Trochlear dysplasia |
| Shallow trochlea | Short lateral trochlea |
| Increased Q-angle | Decreased Q-angle |
| Excessive lateral quadriceps pull | Insufficient vastus medialis obliquus |
| Decreased patellar surface contact area | Abnormal patellar spin |
| Patellar dysplasia | Patella alta |
| Patella baja (infera) | Meniscectomy |
| Laxity of ACL, PCL, MCL, or FCL | Rotatory instability |
| Iliotibial band contracture | Quadriceps contracture |
| Achilles contracture | Retinacular contracture |
| Retinacular laxity | Hyperpronation |
| Pes planus | Tibial tubercle–trochlear groove distance (TT/TG) |
| Patellar malalignment | Patellar instability |
| Patellar subluxation | Medial patellar dislocation |
| Lateral patellar dislocation | Chondral softening |
| Genu recurvatum | Patellar tilt |
| Patellar shift | Abnormal (mal) tracking |
| VMO dysplasia | J sign |
| A sign | Bayonet sign |
| Crossing sign | Trochlear bump |
| Patellar thickness | Knee flexion contracture |
| Infrapatellar contracture | VMO/VLO ratio |
| Rearfoot varus | Patellar glide |
| Quadriceps tendon width | Flexor hallucis longus tendon entrapment |
| Flexor hallucis dysfunction | Increased lumbosacral instability |
| Hip flexion contracture | Abdominal oblique: rectus femoris + psoas imbalance |
| Quadriceps atrophy | Pelvic abductor weakness |
| Increased thoracolumbar extension | Inward pointing knee |
| Female gender |
All three of these disorders are often the result of excessive mechanical force. This excessive force is often the result of a twisting of the knee out of normal alignment. These three disorders may or may not be related and may coexist. It is useful in the evaluation of PF symptoms to consider each independently.
Anterior knee pain may have many causes as suggested in Table 36-1 . Abnormal soft tissue strain caused by twisting of the knee out of normal plane is a likely contributing cause. No studies linking the prevalence of abnormal femoral or tibial torsion with anterior knee pain have been published.
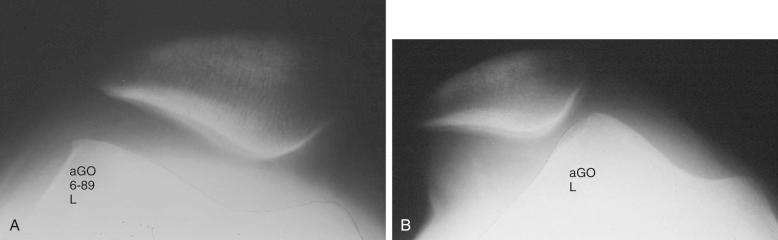
Patellar instability results from a loss of the patellar stabilizers when subjected to an excess of displacement forces. The patellar stabilizers are the trochlear groove and both the medial and lateral PF ligaments and the medial and lateral meniscopatellar ligaments. As early as 1964, Brattström demonstrated that in recurrent dislocation of the patella, a flattening or dysplasia of the trochlear groove is nearly always present. Dejour and colleagues demonstrated that this dysplasia is often in the proximal portion of the trochlea not seen on an axial PF radiograph but measureable on a true lateral knee radiograph by recognizing the floor of the groove and the anterior projections of the medial and lateral condyles. For lateral patellar dislocation to occur, the medial patellofemoral ligaments (MPFLs) must have been injured. A number of authors, including Christoforakis and colleagues and Desio and associates, have demonstrated in the laboratory that the lateral retinaculum provides up to 19% of the resistance against lateral displacement; thus the patella is usually more unstable after lateral retinacular release. Medial dislocation is a distinct possibility, and I reported 70 cases confirmed with stress radiography at the annual meeting of the American Association of Orthopaedic Surgeons in 1990. The diagnosis of instability requires a force and displacement examination, and stress radiography may provide documentation as shown in Figures 36-2 and 36-3 , in which unstressed radiographs were normal but stress application demonstrates obvious excessive displacement.
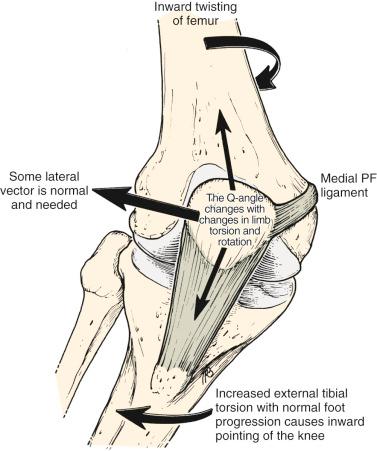
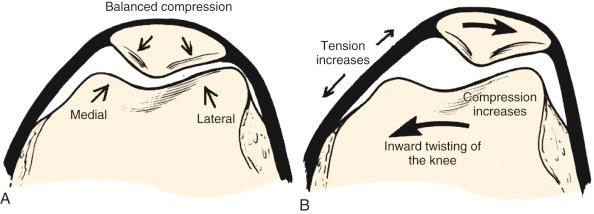
A necessary contributing cause of patellar dislocation is the existence of an abnormally high displacement force. This most often occurs when the direction of the lateral quadriceps vector is increased and commonly occurs when the femur twists medially out from under the patella. This is usually caused by some torsional abnormality of the lower limb ( Fig. 36-4 ). In the face of such excess displacement forces, a PF ligament reconstruction may fail. No studies accurately correlating femoral and tibial torsion with the incidence of patellar instability have been published.
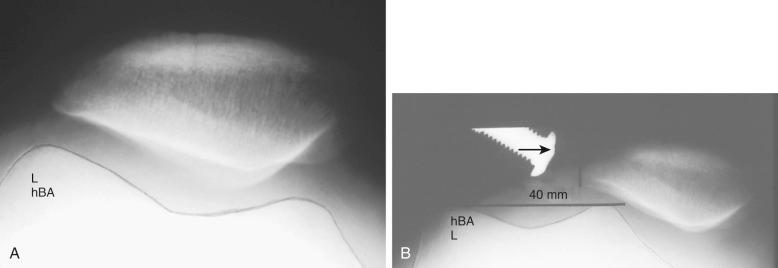
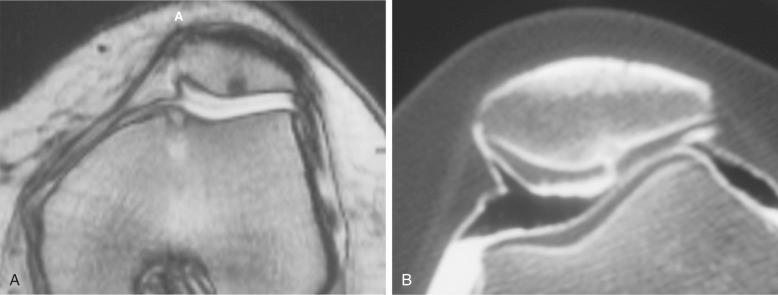
Arthrosis or chondromalacia exists when articular cartilage fails as the force per unit area exceeds biological tolerance. For acute fractures of articular cartilage, this may be in the range of 20 MPa. Chronic overload caused by a too small articular surface area or too much body weight, muscle loading, or long lever arms with chronic pressure exceeding 5 MPa may lead to arthrosis. Articular cartilage fractures exist nearly 100% of the time after acute patellar dislocation. Although magnetic resonance imaging (MRI) is often used to demonstrate articular cartilage lesions, its sensitivity is still limited. Double-contrast computed tomography (CT) arthrography is seldom used but may offer increased resolution as seen in Figure 36-5 . No studies correlating specific articular cartilage lesions with limb torsion have been completed.
The knee joint axis moves straight forward during gait with a small (<10 degrees) turning inward and outward. The foot also tends to move in a fairly constant direction (foot progression angle). The geometry of the lower extremity skeleton largely determines the direction of load application at the PF joint, with the amount of load depending on the body mass, the length of the lever arms, the surface area of the PFJ, and the velocity of the moving system. If the knee joint axis is twisted out of its normal plane of flexion and extension while the quadriceps is contracting, a side-directed force is created that acts on the patella, attempting to displace it. This causes an increased strain on the PF ligaments and retinaculum and an imbalanced direction of force on the PF articular surface.
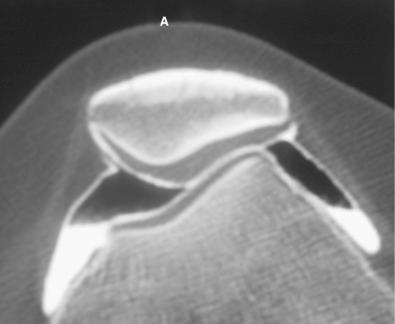
If these side-directed vectors exceed biological tolerance, either instability or arthrosis may result. For example, an inward pointing of the knee increases the lateral direction of pull of the quadriceps. Therefore the pull on the MPFL (and medial retinaculum and medial meniscopatellar ligament) is increased and the direction of pressure on the patella is altered, creating an increase on the lateral facet and a decrease on the medial facet ( Fig. 36-6 ). The radiographic appearance of subchondral density under the patellar facets is a useful clue to the mechanical environment ( Fig. 36-7 ).
Maximum energy conservation during gait is caused by precise anatomy and joint kinematics. Abnormalities in normal bony anatomy or joint motions distort the normal force vectors needed to transfer the body mass to the ground. Deviations in normal limb alignment may result in the knee joint flexion-extension axis advancing sideways while the body moves forward. Causes of a knee joint axis pointing out of the direction include weakness of hip musculature, femoral anteversion or retroversion, excess internal or external tibial torsion, genu valgum or varus, foot hyperpronation, and Achilles contracture.
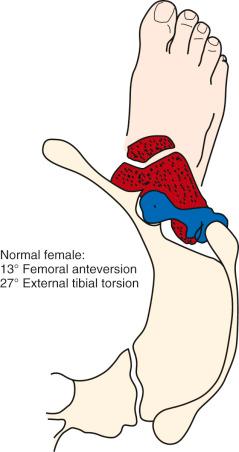
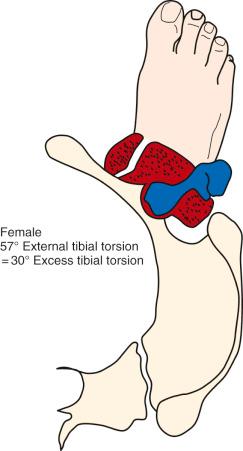
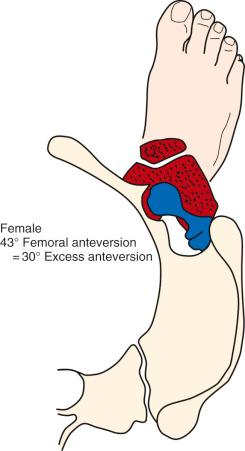
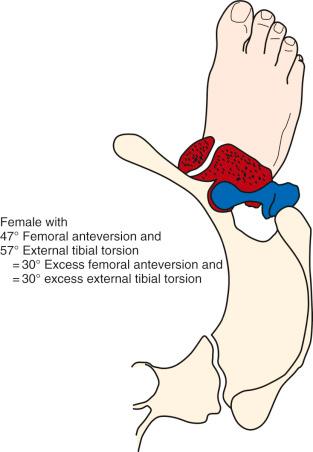
The foot progression angle (FPA) is generally defined as the angle between the long axis of the foot and the direction of body progression and averages between 10 to 15 degrees. It has been shown that the FPA remains similar despite differences in the torsion of the tibia or femur. It is likely that this is because proper ankle dorsiflexion cannot occur during gait if the ankle joint axis is not aligned with the direction of forward movement or because this presents the most stable position of the foot on the ground. Hip rotation must vary if there are changes in the torsion of the long bones and the FPA stays constant. Alterations in both femoral and tibial torsion changes the effective lever arm of the hip stabilizers and may account for the frequency of soft tissue complaints around the hip and pelvis, as well as the increased pelvic tilt and lumbar lordosis seen in these patients. Examples of the change in the position of the hip and knee with a constant foot progression angle and changes in femoral and tibial torsion are seen in Figures 36-8 to 36-12 .
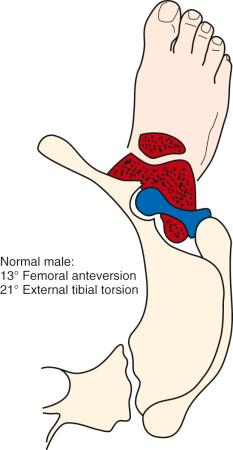
Figures 36-8 to 36-12 are drawn with a foot progression angle of 13 degrees (Seber average) for a normal male torsional alignment ( Fig. 36-8 ), a normal female torsional alignment ( Fig. 36-9 ), a female with 30 degrees of excess external tibial torsion ( Fig. 36-10 ), a female with 30 degrees of excess femoral anteversion ( Fig. 36-11 ), and a female with both 30 degrees of excess tibial external torsion and 30 degrees of excess femoral anteversion ( Fig. 36-12 ). One may study the variations in knee joint progression with these common abnormal patterns. Yoshioka and associates found identical femoral anteversion and genu valgus in both males and females but an increase in external tibial torsion and an increase in foot external rotation in females over males. This increase in external foot rotation may account for the apparent increased genu valgus in females, for the increased incidence in PF symptoms in females, and even for the increased incidence of anterior cruciate ligament (ACL) tears in females.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here