Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The exocrine pancreas has been of considerable interest to physiologists and other scientists for quite some time; in fact, the first demonstration of a hormone action was in the pancreas around the turn of the 20th century. The pancreas has been the major organ used to demonstrate general mechanisms of synthesis and transport for exportable proteins, ion and water secretion, , and signaling pathways involved in these processes. This chapter presents a concise description of the current understanding of exocrine pancreatic physiology.
The functional unit of the exocrine pancreas is composed of an acinus and its draining ductule ( Fig. 56.1 ). The ductal epithelium extends to the lumen of the acinus, with the centroacinar cell situated as an extension of the ductal epithelium into the acinus (see Chapter 55 ). The centroacinar cell plays a key role in providing progenitor cells for pancreatic cell lineages. The ductule drains into interlobular (intercalated) ducts, which in turn drain into the main pancreatic ductal system.
![Fig. 56.1, Regulation of exocrine pancreatic secretion during the intestinal phase of digestion. Exocrine secretions are regulated by endocrine and neurocrine pathways. In addition, the endocrine and neurocrine mediators regulate secretion from the acinus and the duct differently. For the acinus, CCK , secretin, acetylcholine (ACh) , gastrin-releasing peptide (GRP) , vasoactive intestinal polypeptide (VIP) , and substance P regulate secretion. (Signaling mechanisms [second messengers] are shown in Fig. 56.6 .) Secretin and ACh are the major regulators of pancreatic bicarbonate secretion from the duct. (Transporters involved in ductal secretion are illustrated in Fig. 56.4 .) Fig. 56.1, Regulation of exocrine pancreatic secretion during the intestinal phase of digestion. Exocrine secretions are regulated by endocrine and neurocrine pathways. In addition, the endocrine and neurocrine mediators regulate secretion from the acinus and the duct differently. For the acinus, CCK , secretin, acetylcholine (ACh) , gastrin-releasing peptide (GRP) , vasoactive intestinal polypeptide (VIP) , and substance P regulate secretion. (Signaling mechanisms [second messengers] are shown in Fig. 56.6 .) Secretin and ACh are the major regulators of pancreatic bicarbonate secretion from the duct. (Transporters involved in ductal secretion are illustrated in Fig. 56.4 .)](https://storage.googleapis.com/dl.dentistrykey.com/clinical/PancreaticSecretion/0_3s20B9780323609623000564.jpg)
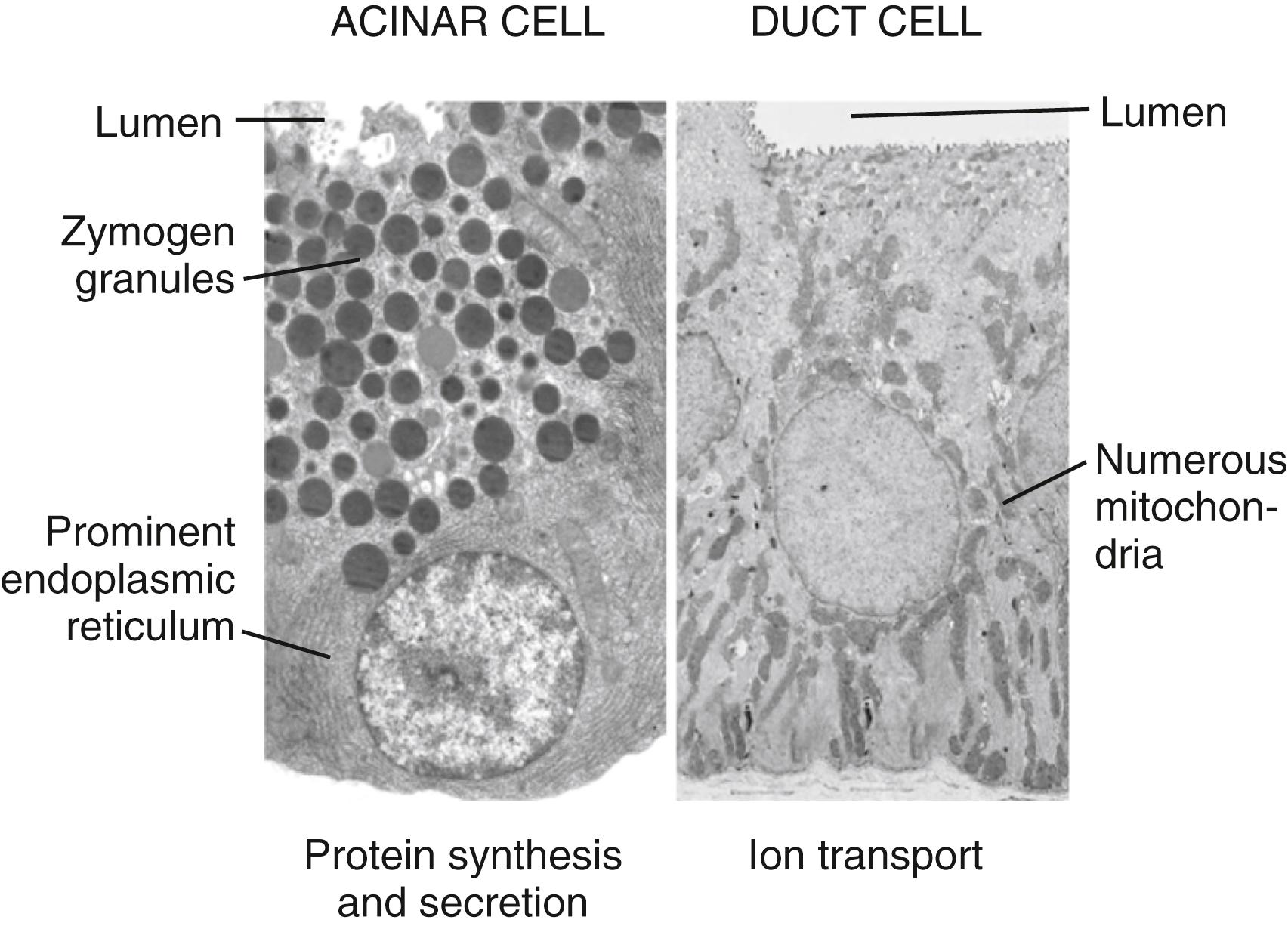
The acinus (from the Latin term meaning “berry in a cluster”) can be spherical or tubular, as shown in Figure 56.1 , or can have some other irregular form. The acinar cells are specialized to synthesize, store, and secrete digestive enzymes. Receptors for hormones and neurotransmitters that stimulate enzyme secretion are located on their basolateral membrane. The basal aspect of the cell contains the nucleus as well as abundant rough endoplasmic reticulum (RER) for protein synthesis ( Fig. 56.2 , left ). The apical region of the cell contains zymogen granules, which store digestive enzymes. The apical surface of the acinar cell also possesses microvilli. Within the microvilli and in the cytoplasm underlying the apical plasma membrane is a filamentous actin meshwork that is involved in exocytosis of the contents of the zymogen granules. Secretion is into the lumen of the acinus. Tight junctions between acinar cells form a band around the apical aspects of the cells and act as a barrier to prevent passage of large molecules such as the digestive enzymes. The junctional complexes also provide for the paracellular passage of water and ions.
Another intercellular connection between acinar cells is the gap junction. This specialized area of the plasma membrane between adjacent cells acts as a pore to allow small molecules (molecular weight 500 to 1000 Da) to pass between cells. The gap junction allows chemical and electrical communication between cells. For example, calcium signaling is coordinated between the cells of an acinus with effects on digestive enzyme secretion. ,
The duct epithelium consists of cells that are cuboidal to pyramidal and contain the abundant mitochondria necessary for energy products needed for ion transport (see Fig. 56.2 , right ). The duct cells as well as the centroacinar cells contain carbonic anhydrase, which is important for their ability to secrete bicarbonate.
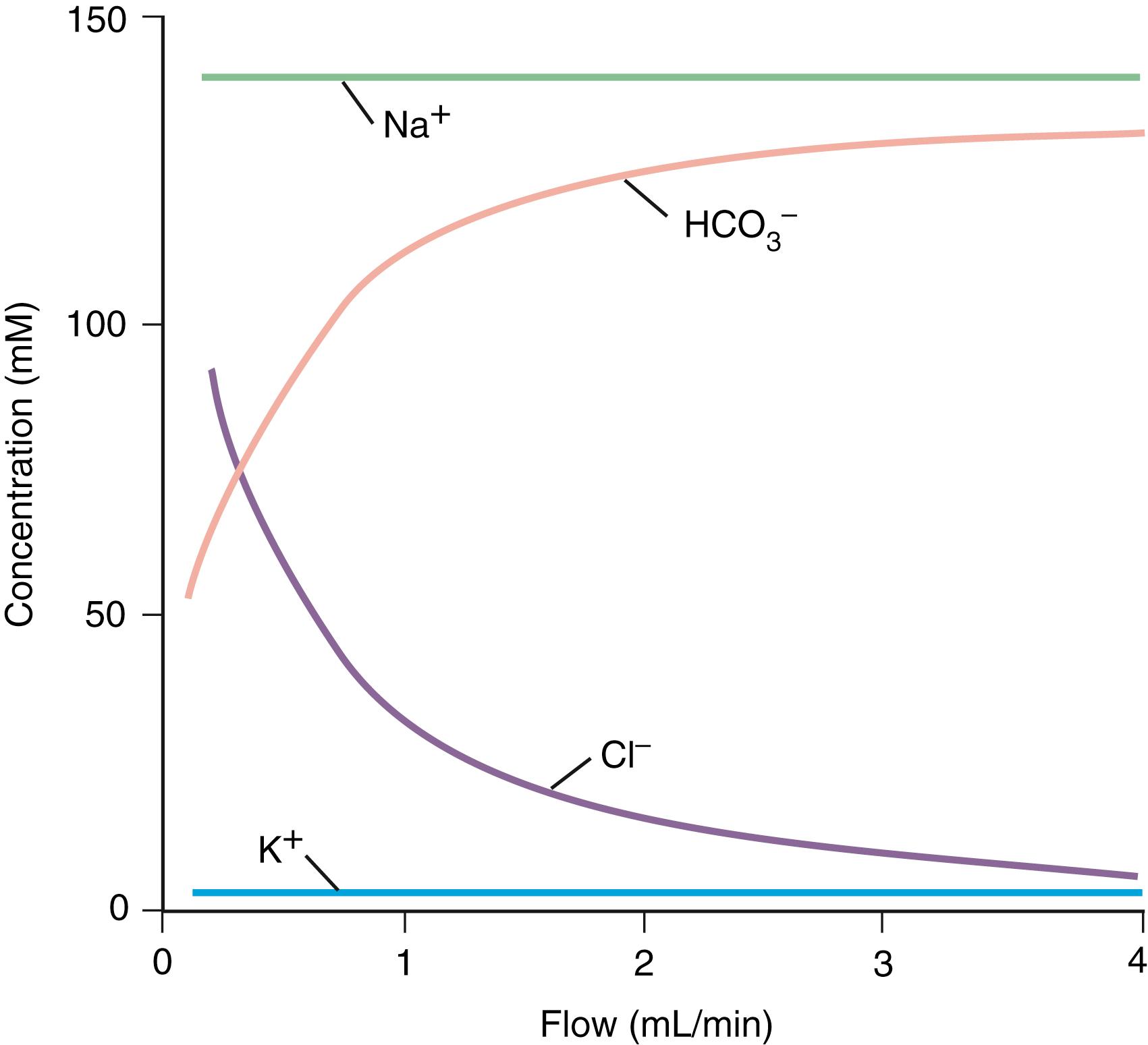
The principal inorganic components of exocrine pancreatic secretions are water, sodium, potassium, chloride, and bicarbonate ( Fig. 56.3 ). The purposes of the water and ion secretions are to deliver digestive enzymes to the intestinal lumen and to help neutralize gastric acid emptied into the duodenum. Pancreatic juice secreted during stimulation with secretin is clear, colorless, alkaline, and isotonic with plasma. The flow rate increases from an average rate of 0.2 or 0.3 mL/min in the resting (interdigestive) state to 4.0 mL/min during postprandial stimulation. The total daily volume of secretion is 2.5 L. The osmolality of pancreatic juice is independent of flow rate. However, when the pancreas is stimulated by secretin (the major mediator of the greater volume output), bicarbonate and chloride concentrations change reciprocally (see Fig. 56.3 ).
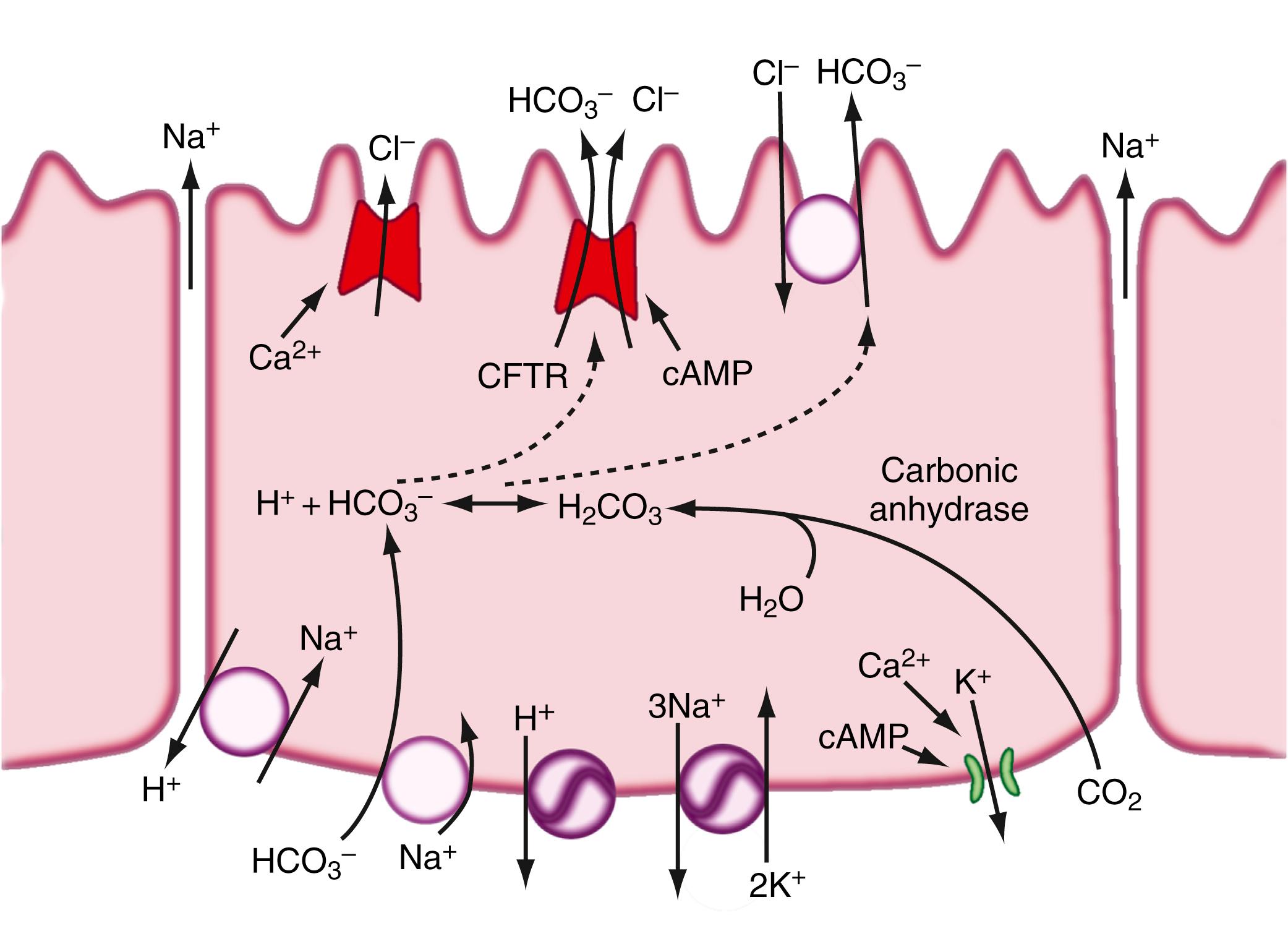
Secretin stimulates secretion by binding to its receptor on the basolateral membrane of the duct cell, thus activating adenylate cyclase and increasing cyclic adenosine monophosphate (cAMP); acetylcholine does so by binding to its receptor and raising intracellular calcium concentrations. The initial events with secretin stimulation involve cAMP-dependent and Ca 2+ -dependent chloride (Cl − ) channel activation on the luminal membrane as well as K + channel activation on the basolateral membrane ( Fig. 56.4 ). , The cAMP-dependent luminal Cl − channel is the CFTR. , Activation of this channel by cAMP leads to Cl − secretion into the lumen, where it is coupled to a Cl − -HCO 3 − antiport, resulting in an exchange of Cl − for HCO 3 − in the lumen. Evidence suggests that CFTR is also directly involved in HCO 3 − secretion. , , , On the basolateral surface of the duct cell are a Na + ,H + antiport, a Na + ,HCO 3 − cotransport, 2 ATPases (H + -ATPase and Na + ,K + -ATPase), and a K + channel. In combination, these various transporters facilitate HCO 3 − secretion at the apical surface as well as maintain a neutral pH within the duct cell. Na + and water are secreted into the ductal system to counter the electrical and osmotic forces resulting from the HCO 3 − secretion. Of importance, mutational alterations with complete lack of CFTR function result in destruction of the exocrine pancreas in childhood, whereas mutations with partial function can lead to pancreatitis later in life. Also, recent studies show that alcoholism and smoking causes inhibition of CFTR function which could play a role in causing pancreatitis. ,
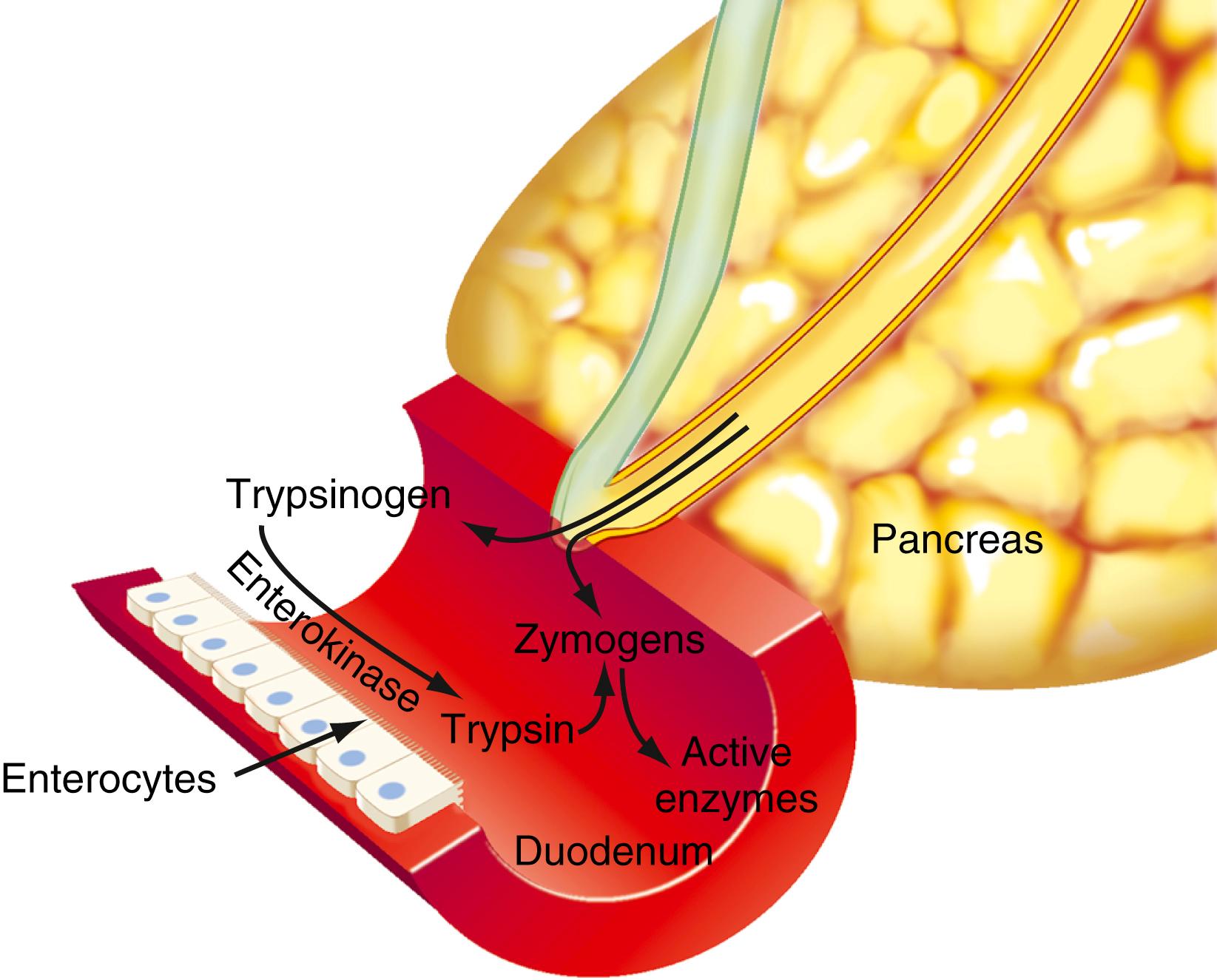
The human pancreas has a large capacity for synthesizing protein (mostly digestive enzymes). Box 56.1 lists the major proteolytic, amylolytic, lipolytic, and nuclease digestive enzymes. Some of the enzymes are present in more than one form (e.g., cationic trypsinogen, anionic trypsinogen, and mesotrypsinogen). Enzymes that could digest the pancreas are stored in the pancreas and secreted into the pancreatic duct as inactive precursor forms. As illustrated in Figure 56.5 , activation of these enzymes takes place in the intestinal lumen, where a brush-border glycoprotein peptidase, enterokinase, activates trypsinogen by removing (by hydrolysis) an N -terminal hexapeptide fragment of the molecule (Val-Asp-Asp-Asp-Asp-Lys). The active form, trypsin, then catalyzes the activation of the other inactive proenzymes.
∗ Proenzymes listed are stored in the pancreas and secreted into the duodenal lumen as inactive proenzyme forms. If these enzymes were active in the pancreas, they would digest the pancreatic gland. Other enzymes, such as amylase and lipase, are stored and secreted in their active forms.
Anionic trypsinogen
Cationic trypsinogen
Chymotrypsinogen (A, B)
Kallireinogen
Mesotrypsinogen
Procarboxypeptidase A (1, 2)
Procarboxypeptidase B (1, 2)
Proelastase
Prophospholipase A 2
Amylase
Carboxylesterase
DNase
Lipase (TG lipase)
RNase
Sterol esterase
In addition to the digestive enzymes, the acinar cell secretes a trypsin inhibitor, pancreatic secretory trypsin inhibitor. This 56–amino acid peptide inactivates trypsin by forming a relatively stable complex with the enzyme near its catalytic site. The function of the inhibitor is to inactivate and promote degradation of trypsins that are formed autocatalytically in the pancreas or pancreatic juice, thus preventing disorders such as pancreatitis.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here