Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Pediatrics is the only discipline dedicated to all aspects of the care and well-being of infants, children, and adolescents, including their health—their physical, mental, social, and psychological growth and development—and their ability to achieve full potential as adults. Pediatricians must be concerned not only with specific organ systems, genetics, and biologic processes, but also with environmental, psychosocial, cultural, and political influences, all of which may have major impacts on the health and well-being of children and their families.
Children cannot advocate wholly for themselves. As the professionals whose purpose is to advance the well-being of children, pediatricians must be advocates for the individual child and for all children, irrespective of culture, religion, gender, sexual orientation, race, or ethnicity or of local, state, or national boundaries. The more politically, economically, or socially disenfranchised a population is, the greater the need for advocacy for its children and for those who support children. Youth are often among the most vulnerable persons in society, and thus their needs require special attention. As segmentation between nations blur through advances in media, transportation, technology, communication, and economics, a global , rather than a national or local, perspective for the field of pediatrics becomes both a reality and a necessity. The interconnectedness of health issues across the world has achieved widespread recognition in the wake of the Zika, Ebola, SARS, and AIDS epidemics; war and bioterrorism; the tsunami of 2004; the earthquake in Haiti in 2010; the displacement of families during the Syrian refugee crisis in 2016–2018; and the growing severity of drought, hurricanes, and cyclones brought about by climate change.
More than a century ago, pediatrics emerged as a medical specialty in response to increasing awareness that the health problems of children differ from those of adults, and that a child's response to disease and stress varies with age and development. In 1959 the United Nations issued the Declaration of the Rights of the Child , articulating the universal presumption that children everywhere have fundamental needs and rights. Today, an affirmation of those rights and an effort to satisfy those needs are more important than ever.
From 1990 to 2010, the world population grew at an annual rate of 1.3% per year, down from 1.8% during the prior 20 yr. This rate continues to decline; in 2016 the growth rate was 1.13%. Worldwide, there are 2.34 billion children 18 yr and younger, which accounts for approximately one third (32%) of the world's population of 7.4 billion persons. In 2016 the average birthrate in the world was 18.5 births per 1,000 population, with a high of 44.8/1,000 in Niger to the lowest in Monaco at 6.6/1,000. The most populous countries—China, India, and the United States—have rates of 12.4, 19.3, and 12.5 per 1,000 population, respectively.
Despite global interconnectedness, the health of children and youth varies widely between and within regions and nations of the world, depending on several interrelated factors. These include (1) economic conditions; (2) educational, social, and cultural considerations; (3) health and social welfare infrastructure; (4) climate and geography; (5) agricultural resources and practices, which account for nutritional resources; (6) stage of industrialization and urbanization; (7) gene frequencies for certain disorders; (8) the ecology of infectious agents and their hosts; (9) social stability; and (10) political focus and stability. Although genetics, biology, and access to affordable and quality healthcare are important determinants, it has been shown that the social determinants of health—the physical environment, political and economic conditions, social and cultural considerations, and behavioral psychology—play as great a role, if not greater, in health outcomes.
To ensure that the needs of children and adults worldwide were not obscured by local needs, in 2000 the international community established 8 Millennium Development Goals (MDGs) to be achieved by 2015. Although all 8 MDGs impact child well-being, MDG 4 was exclusively focused on children: to reduce the under-five mortality rate (U5MR) by two-thirds between 1990 and 2015. It was estimated that poor nutrition contributed to more than one third of the deaths worldwide in children <5 yr old, so many of the efforts to reach this goal centered on increasing household food security. Increasing measles vaccination, particularly in sub-Saharan Africa, was another strategy to reduce the U5MR.
There was some progress in achieving MDG 4; the worldwideU5MR decreased by 50% between 1990 and 2015. Although the goal of a two-thirds reduction was not achieved, deaths in children under5 dropped from 12.7 million in 1990 to about 6 million in 2015, despite growth in world population during the same period.
The U5MR can be further divided into neonatal (<1 mo of age), infant (<1 yr of age), and after infancy (1-5 yr of age) ( Fig. 1.1 ). The leading causes of worldwide U5MR are preterm birth complications, pneumonia, perinatal asphyxia, diarrheal diseases, and malaria. Many of these causes are linked to malnutrition . Children in sub-Saharan Africa are 14 times more likely to die before age 5 yr than children in the developed areas of the world.
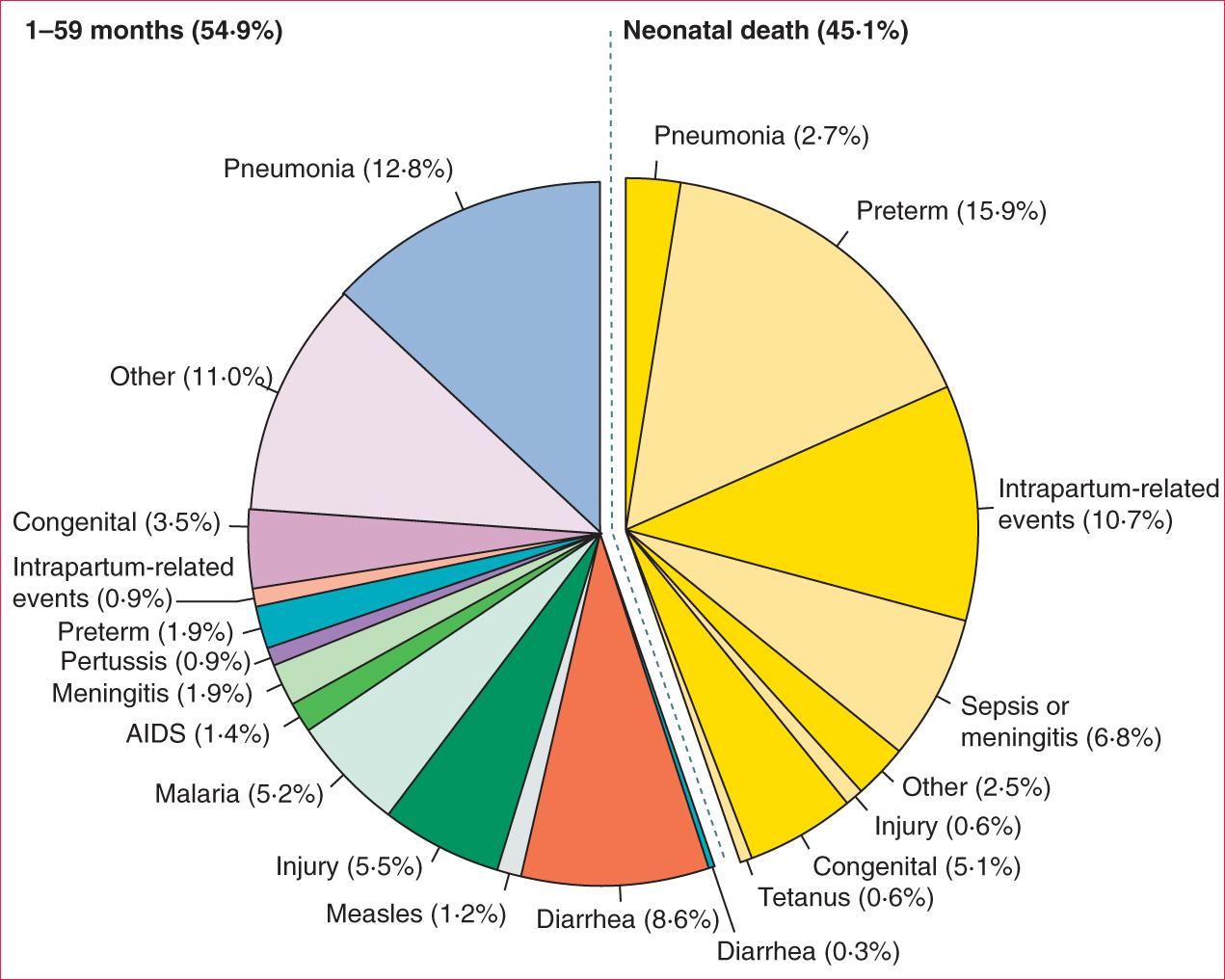
Causes of under-5 mortality differ greatly between developed and developing nations. In developing countries, 66% of deaths in children <5 yr old resulted from infectious and parasitic diseases. Among the 42 countries having 90% of childhood deaths, diarrheal disease accounted for 22% of deaths, pneumonia 21%, malaria 9%, AIDS 3%, and measles 1%. Neonatal causes contributed 33%. In the United States, pneumonia (and influenza) accounted for only 2% of under-5 deaths, with only negligible contributions from diarrheal diseases and malaria. Unintentional injury is the most common cause of death among U.S. children age 1-4 yr, accounting for approximately 33% of deaths, followed by congenital anomalies (11%), homicides (9%), and malignant neoplasms (8%). Other causes accounted for <5% of total mortality within this age-group ( Table 1.1 ). Violence is a significant contributor to injury-related mortality in all child age-groups ( Tables 1.2 and 1.3 ). Although unintentional injuries in developing countries are proportionately less important causes of mortality than in developed countries, the absolute rates and contributions of these injuries to morbidity are substantially greater.
The infant mortality rate (deaths of children <1 yr old) accounts for 85% of the U5MR in industrialized countries, but only 70% in the least developed nations. Neonatal (<1 mo) death contributes substantially as well, growing in proportion as the U5MR decreases. Globally, the neonatal mortality rate of 19/1,000 live births represents 60% of the infant mortality rate and 45% of the U5MR. The neonatal mortality rate is responsible for 56% of the U5MR in industrialized nations, 45% in developing countries, but only 38% in the least-developed countries. More children <5 yr old in developing countries die from non–birth-related causes.
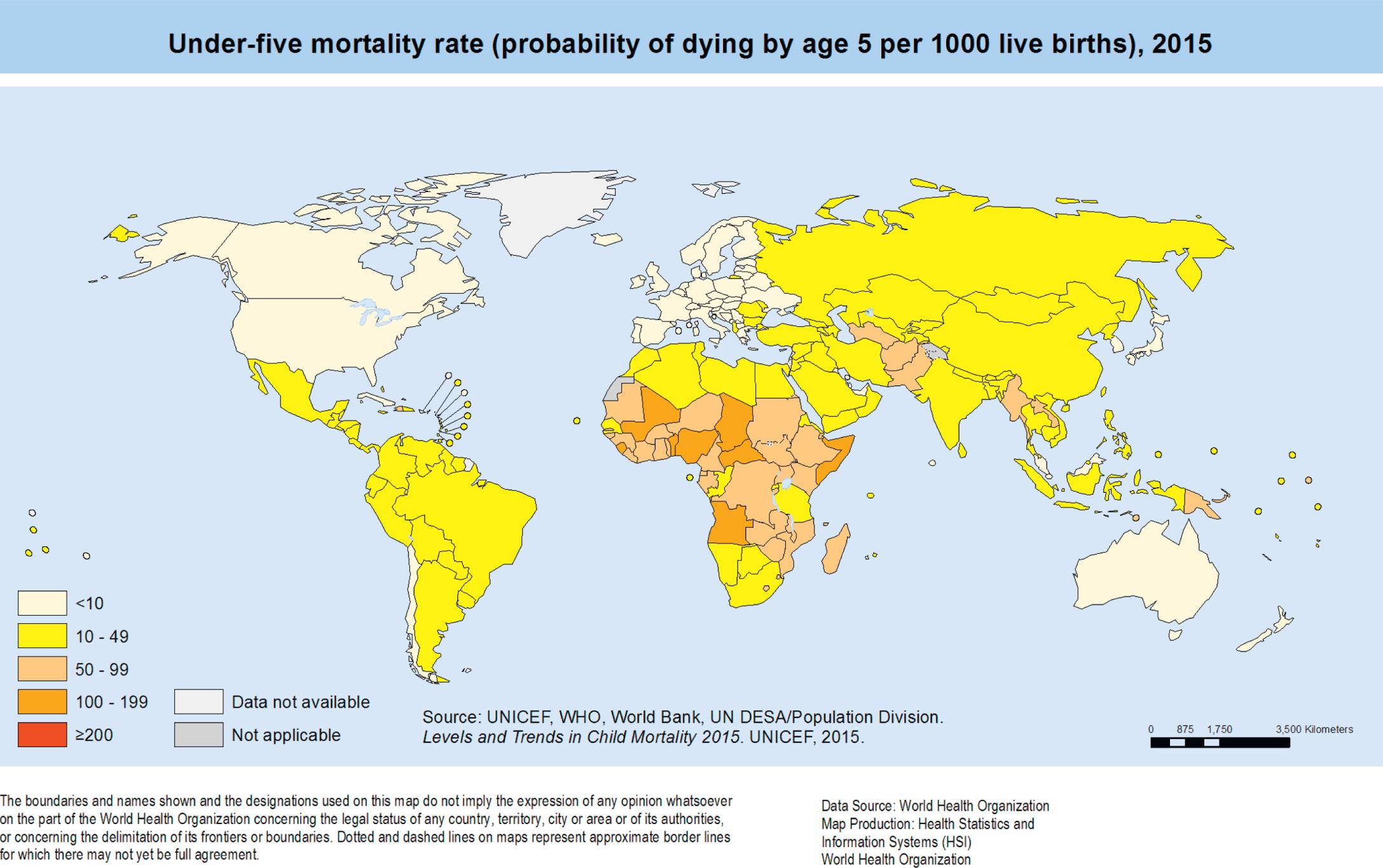
Across the globe, there are significant variations in child mortality rates by nation, by region, by economic status, and by level of industrial development, the categorizations employed by the World Bank ( http://wdi.worldbank.org/table/2.18 ). As of 2015, 8 nations have a U5MR of ≥100 per 1,000 live births (all in the WHO African region) ( Fig. 1.2 ). The average U5MR in low-income countries was 76/1,000 live births, and in high-income countries, 6/1,000. Income and wealth, however, are not the only determinants of mortality. For example, the United States has the 10th highest gross national income per capita, but ranked 57th in lowest infant mortality rate in 2016.
In addition to mortality rates, causes of death vary by developmental status of the nation. In the United States the 3 leading causes of death among children <5 yr old were congenital anomalies, disorders related to gestation and low birthweight, and unintentional injuries. By contrast, in developing countries, most infant deaths are caused by pneumonia, diarrheal disease, and malaria.
A profound improvement in child health within industrialized nations occurred in the 20th century with the introduction of vaccines, antibiotic agents, and improved hygienic practices. Efforts to control infectious diseases were complemented by better understanding of the role of nutrition in preventing illness and maintaining health. In the United States, Canada, and parts of Europe, new and continuing discoveries in these areas led to establishment of publicly funded well-child clinics for low-income families. Although the timing of infectious disease control was uneven around the globe, this focus on control was accompanied by significant decreases in morbidity and mortality in all countries.
In the later 20th century, with improved control of infectious diseases through more effective prevention and treatment (including the eradication of polio in the Western hemisphere), pediatric medicine in industrialized nations increasingly turned its attention to a broad spectrum of noninfectious acute and chronic conditions. These included potentially lethal conditions as well as temporarily or permanently handicapping conditions. Advances occurred in the diagnosis, care, and treatment of leukemia and other neoplasms, cystic fibrosis, sickle cell disease, diseases of the newborn infant, congenital heart disease, genetic defects, rheumatic diseases, renal diseases, and metabolic and endocrine disorders.
Until the 1970s and early 1980s, children affected with sickle cell disease often died within the 1st 3 yr of life often from overwhelming sepsis caused by encapsulated bacteria. In the 1980s a multicenter study showed that early initiation of penicillin prophylaxis led to an 84% risk reduction for pneumococcal sepsis. Life expectancy for those with sickle cell disease increased when penicillin prophylaxis was initiated early in life. The use of prophylactic penicillin became the standard of care, increasing the importance of early detection of sickle cell disease (which led to expanding universal newborn screening ) and paving the way for advances in the chronic management of the disease, including transfusion therapy, radiographic screening for silent cerebral infarctions, and hydroxyurea as a disease-modifying therapy. The success of penicillin prophylaxis likely led to a more rapid rate of innovation in the diagnosis and management of the disease, since children with the condition now had increased life expectancy. Whereas in the preprophylaxis era children often died by age 3, now 95% of individuals born with sickle cell disease will live to their 18th birthday, and most will survive until their 5th decade.
The treatment of acute lymphoblastic leukemia (ALL), the most common pediatric malignancy, has also shown amazing advances. Five-year survival rates have increased from <10% in the 1960s to >90% in 2000–2005. Cystic fibrosis has shown improvements in survival as well. In the 1960s, most children with cystic fibrosis did not live until school age. With advances in pulmonary and nutritional therapies, as well as earlier initiation of these therapies secondary to earlier identification through newborn screening, a child born with cystic fibrosis in 2010 has a projected life expectancy of 39-56 yr.
These major advances in the management of chronic diseases of childhood were accomplished when significant improvement occurred in the prevention and treatment of acute infectious diseases, at least in industrial countries. This allowed human and economic resources to shift toward addressing chronic disease.
Given the advances in public health aimed at decreasing morbidity and mortality in infectious diseases (immunization, hygiene, antibiotics), along with the rise of technologic advances in clinical care, attention was given to the new morbidities —behavioral, developmental, and psychosocial conditions and problems shown to be increasingly associated with suboptimal health outcomes and quality of life. The American Academy of Pediatrics (AAP) Committee on Psychosocial Aspects of Child and Family Health asserted that the prevention, early detection, and management of these types of child health problems should be a central focus of the field of pediatrics, and that it would require an expansion in the knowledge base regarding (1) physical and environmental factors affecting behavior, (2) normal child behavior and development, (3) health behaviors as they pertain to child health, and (4) mild, moderate, and severe behavioral and developmental disorders. Accomplishing this would require reconceptualizing professional training, improving clinical communication and interviewing skills, expanding mental health resources for children, and shifting time allocation during child health supervision visits to address these concerns. In 2001 the Committee revisited this issue and reemphasized the need to address environmental and social aspects in addition to developmental and behavioral issues ( Table 1.4 ). These included violence, firearms, substance use, and school problems, as well as poverty, homelessness, single-parent families, divorce, media, and childcare. Although this expanding list seems daunting and beyond the scope of what pediatricians typically addressed (i.e., physical health and development), many of these behavioral, environmental, and psychosocial issues (which fall under the category of social determinants of health) account for a large proportion of variance in health outcomes in children and youth. The role of pediatrics and the boundaries of clinical practice needed to change in order to address these salient contributors to child health and well-being. Newer models of clinical care that rely on close collaboration and coordination with other professionals committed to child welfare (e.g., social workers, psychologists, mental health providers, educators) were developed. As this model expanded, so did the role of the family, in particular the child's caregiver, from a passive recipient of professional services to a more equitable and inclusive partner in identifying the issues that needed to be addressed, as well as helping decide which therapeutic options had the “best fit” with the child, the family, and the condition.
| THE NEW MORBIDITIES (1982–1993) | THE NEW MORBIDITIES REVISITED (2001) | THE “NEW” NEW MORBIDITIES (2010 to Present) |
|---|---|---|
| Behavioral disorders/mental health | School problems | Adverse childhood experiences (ACEs) |
| Family crisis | Mood and anxiety disorders | Toxic stress |
| Abuse & neglect | Adolescent suicide/homicide | Allostatic load |
| Long term disease | Firearms in home | Chronic illnesses of lifestyle (e.g., obesity, type-2 diabetes, hypertension) |
| Substance abuse | School violence | Behavioral conditions (autism, ADHD, depression, anxiety) |
| School difficulties | Drug and alcohol abuse | Food insecurity |
| HIV infection | Oral health | |
| Effects of media | Witnessing community/interpersonal violence | |
| Poverty | Peer victimization/bullying | |
| Homelessness | Discrimination | |
| Single-parent families | ||
| Effects of divorce | ||
| Struggle of working parents | ||
| Childcare quality & policy |
* Each column adds further categories and refinements to prior columns.
The framing of salient child health issues under the “new morbidity” concept acknowledges that the determinants of health are heterogeneous but interconnected. Biology, genetics, healthcare, behaviors, social conditions, and environmental influences should not be viewed as mutually exclusive determinants; they exert their influences through complex interactions on multiple levels. For example, epigenetic changes that result from specific social and environmental conditions illustrate the influence of context on gene expression.
Studies have demonstrated that while each of these interrelated determinants are important for optimal health, development, and well-being, the greatest contributions to health outcomes occur in the behavioral, social, and environmental domains—the social determinants of health . From 40% to 70% of the relative variation in certain health outcomes is caused by social and economic conditions, health behaviors, and environmental factors. Whereas traditional medical education and clinical practice emphasized the biologic, genetic, and healthcare-related determinants of health, the recognition of the new morbidities as a focus of child healthcare provision reinforced the need to address social determinants as a key component of pediatric care, training, and research.
The new morbidities concept brought into perspective the importance of addressing the social determinants of health, as well as the increasing prevalence and salience of chronic physical and behavioral health conditions in pediatric healthcare. Since then, advances in epidemiology, physiology, and epigenetics have expanded the scope of inquiry into the effects of a broad range of health determinants and provided more sophisticated explanatory models for the mechanisms that explain their effects ( Table 1.4 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here