Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Most primary lung cancers comprise the histologic variants described in other chapters of this text. On occasion, however, the thoracic surgeon must diagnose and treat an unusual primary lung cancer. These tumors frequently have a similar clinical presentation to more common tumors, but there are often subtle differences in treatment. Hence, knowledge of these tumors, their characteristics, and the ensuing diagnostic and treatment paradigms are important for the practicing thoracic surgeon.
Bronchopulmonary carcinoid tumors account for one quarter of all carcinoid tumors, represent 1.2% of all primary lung tumors in adults, and are the most common primary lung tumor in children. Overall, when all carcinoids are accounted for, they are distributed almost equally between males and females; however, in the bronchopulmonary subset, they are found predominantly in females. The incidence is significantly higher in white patients than in black, Asian, and Hispanic patients. Compared with bronchogenic carcinomas, carcinoid tumors occur more frequently in younger patients and are less likely to be associated with a significant smoking history.
Bronchopulmonary carcinoid tumors arise from neuroendocrine cells and are thus positioned on the neuroendocrine tumor spectrum, which includes the more aggressive large-cell neuroendocrine carcinomas and small-cell lung carcinomas. Bronchopulmonary carcinoid tumors are classified as either typical or atypical on the basis of histologic features. Typical carcinoid tumors account for three quarters of bronchopulmonary carcinoids, are often centrally located, and rarely metastasize. In contrast, atypical carcinoid tumors are located more frequently in the lung periphery and metastasize in more than 40% of cases. Atypical carcinoid tumors occur more often with increasing age and are rarely seen in patients younger than 30 years. Unlike high-grade bronchopulmonary neuroendocrine tumors (large-cell and small-cell variants), typical and atypical bronchopulmonary carcinoids rarely occur in combination with other adenocarcinomas; however, the risk of synchronous breast and prostate cancer is slightly elevated.
Most bronchopulmonary carcinoid tumors, particularly typical carcinoids, are centrally located. Fink et al reported that 68% of bronchopulmonary carcinoid tumors were located in the major bronchi (13% in the mainstem bronchi and 55% in lobar bronchi), with the remaining 32% in peripheral locations. Because of the predominance of central location, these tumors can often be visualized bronchoscopically, demonstrating a sessile, red-brown to bluish-tan endobronchial mass with variable vascularity and a smooth surface. On gross pathologic examination, typical carcinoids appear as a white or gray cut surface without evidence of hemorrhage or necrosis. In contrast, atypical carcinoids tend to be located peripherally in the lungs. On gross pathologic examination, atypical carcinoids appear white-gray on section but can exhibit a color of tan, pink to yellow-brown, and red.
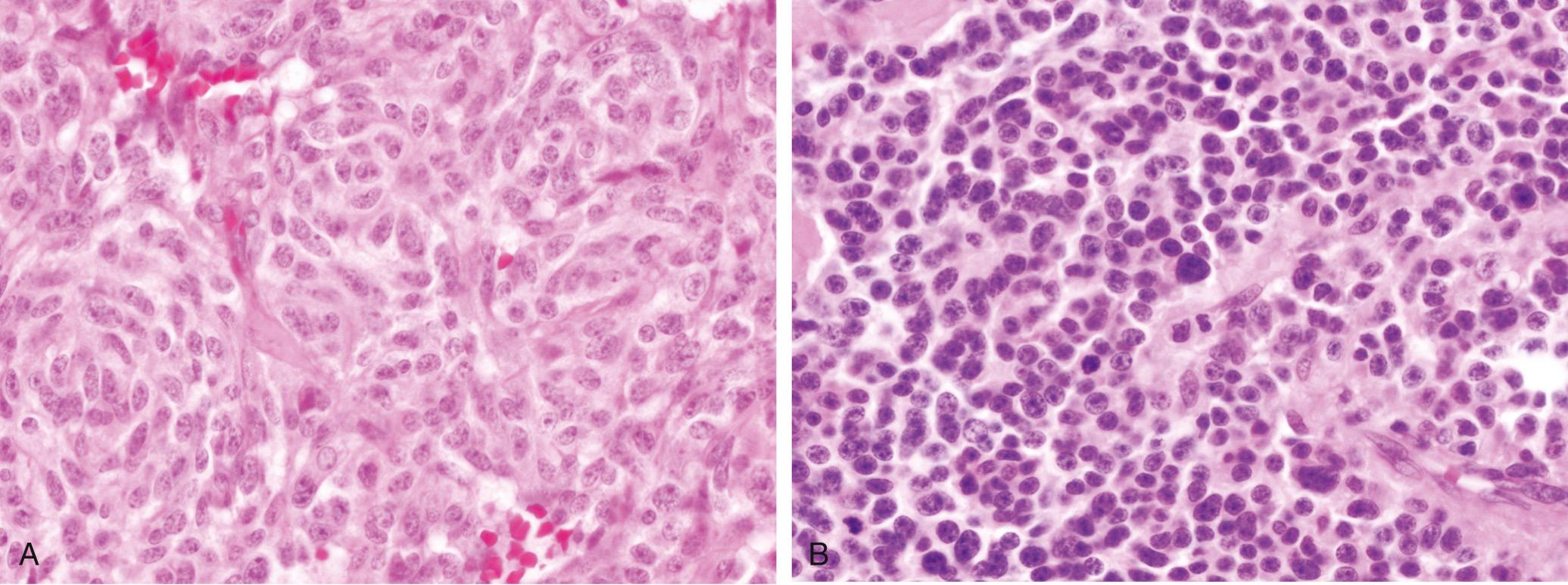
The World Health Organization (WHO) classification of pulmonary neuroendocrine tumors is based on morphologic and histologic features, which clearly influence tumor behavior and prognosis. The spectrum of neuroendocrine tumors includes low-grade typical carcinoids, intermediate-grade atypical carcinoids, and high-grade large- and small-cell variants. Typical carcinoid tumors have fewer than 2 mitoses per 10 high power fields (HPF), have no evidence of necrosis, and are larger than 0.5 cm. Tumors smaller than 0.5 cm are classified as carcinoid tumorlets and are addressed later in this chapter. Atypical carcinoid tumors have 2 to 10 mitoses per 10 HPF or necrosis. Figure 22-1 demonstrates the histologic appearance of a typical and an atypical carcinoid tumor. In comparison, large- and small-cell carcinomas contain greater than 10 mitoses per 10 HPF and are further distinguished on the basis of other morphologic characteristics. Although the WHO classification places these four subtypes under the general heading of bronchopulmonary neuroendocrine tumors, the results of histopathologic and immunochemical studies support the idea that bronchopulmonary carcinoids are distinct from the more malignant and high-grade neuroendocrine tumors.
Gustafsson and colleagues discussed a separate entity termed diffuse idiopathic pulmonary neuroendocrine cell hyperplasia (DIPNECH). This rare preneoplastic condition features proliferation of pulmonary neuroendocrine cells and neuroepithelial bodies. When this proliferation extends beyond the basement membrane, the group of cells is identified as a carcinoid tumorlet. These tumorlets are nodular, carcinoid-like proliferations of neuroendocrine cells less than 5 mm in size; those that proliferate to greater than 5 mm are classified as carcinoid tumors. DIPNECH can be both an adaptive response, as seen in persons living at high altitudes, and a reactive response to lung injury, as seen in patients with obliterative bronchiolitis, chronic cough, and interstitial lung disease. Table 22-1 describes the major distinctions among DIPNECHs, tumorlets, and carcinoids.
| Type of Tumor | Location | Nodal Metastases | Gross Pathologic Examination | Histologic/WHO Criteria |
|---|---|---|---|---|
| DIPNECH | Variable | None | Nodular bronchial wall thickening | No extension beyond basement membrane |
| Carcinoid tumorlet | Variable | None | Small, similar appearance to carcinoid tumors | Carcinoid-like, but <0.5 cm in size, mitoses very uncommon |
| Typical carcinoid | Central | Rare | White or gray with minimal evidence of necrosis or hemorrhage | <2 mitoses/2 mm 2 >0.5 cm in size Lack of necrosis |
| Atypical carcinoid | Peripheral | Frequent | White-gray that on section appears tan, pink, red, or yellow-brown | 2-10 mitoses/2 mm 2 >0.5 cm in size Necrosis |
Molecular genetic analysis has demonstrated that multiple genes are involved in the development and progression of carcinoid tumors. One important genetic mechanism is loss of heterozygosity (LOH), which can occur in multiple chromosomes, including but not limited to 3p, 5q21 (MCC/APC), 9p21 ( p16 gene), 11q13 ( MEN1 gene), 13q14 (retinoblastoma [RB] gene), and 17p13 ( p53 gene). LOH at chromosome 3p is the most frequent change in bronchopulmonary neuroendocrine tumors and has been observed in 40% of typical carcinoids and 73% of atypical carcinoids. p53 mutations and loss of 5q21 occur in higher-grade tumors and are associated with worse survival.
Bronchopulmonary carcinoids are known to occur as components of familial endocrine cancer syndromes, namely multiple endocrine neoplasia 1 (MEN1), although this rarely occurs. The MEN1 gene is inactivated by mutation in approximately 47% of typical carcinoids and 70% of atypical carcinoids. More recently, a study evaluated 129 patients with MEN1 and found that 6 of these (5%) had been diagnosed with bronchopulmonary carcinoids on initial diagnosis. An additional 32 patients had chest computed tomography (CT) scans for review, and 12 of these (38%) had pulmonary nodules suspicious for bronchopulmonary carcinoid, 4 of which were histologically confirmed to be a carcinoid. This study demonstrated that the incidence of bronchopulmonary carcinoid in MEN1 is much higher than previously believed; therefore, it is recommended that patients with MEN1 be screened for bronchopulmonary carcinoids with chest CT imaging every 3 years, with onset at 20 years of age.
The p53 gene (chromosome 17p13) is important for maintaining genomic stability, in addition to numerous other functions. LOH or abnormal expression at the p53 locus has been detected in 4% of typical carcinoids and 29% of atypical carcinoids. Kobayashi et al evaluated the frequency of p53 protein expression in several bronchopulmonary carcinoid tumors and found that the sampled typical carcinoids did not demonstrate any expression; in contrast, 20% of the sampled atypical carcinoids had expression.
The presentation of bronchopulmonary carcinoid tumors is dependent on both the size and the location of the tumor; given the high proportion of centrally located carcinoid tumors, most patients are symptomatic at presentation. The most common symptoms are cough, hemoptysis, dyspnea, wheezing, and recurrent upper respiratory infections or pneumonia, caused by endoluminal obstruction by the tumor. Symptoms may be present for many years before diagnosis is made and almost entirely reflect the anatomic location of the lesion, as opposed to the secreted bioactive products. Although some patients with bronchopulmonary carcinoid tumors may initially have carcinoid syndrome (diarrhea, flushing, bronchoconstriction, and heart failure), in general this is exceedingly rare. Infrequently, bronchopulmonary carcinoids may secrete adrenocorticotropic hormone (ACTH) (Cushing syndrome), growth hormone, or other bioactive substances. Carcinoid tumors are one of the most frequent causes of ectopic secretion of ACTH. Box 22-1 depicts common endocrinopathies associated with carcinoid tumors. A quarter of patients are asymptomatic, and thus many of these tumors are found incidentally or are never discovered. A population-based study in Denmark showed that 24% of typical carcinoids and 7% of atypical carcinoids were discovered on autopsy.
Carcinoid syndrome
Cushing syndrome
Acromegaly
Hypercalcemia
Hypoglycemia
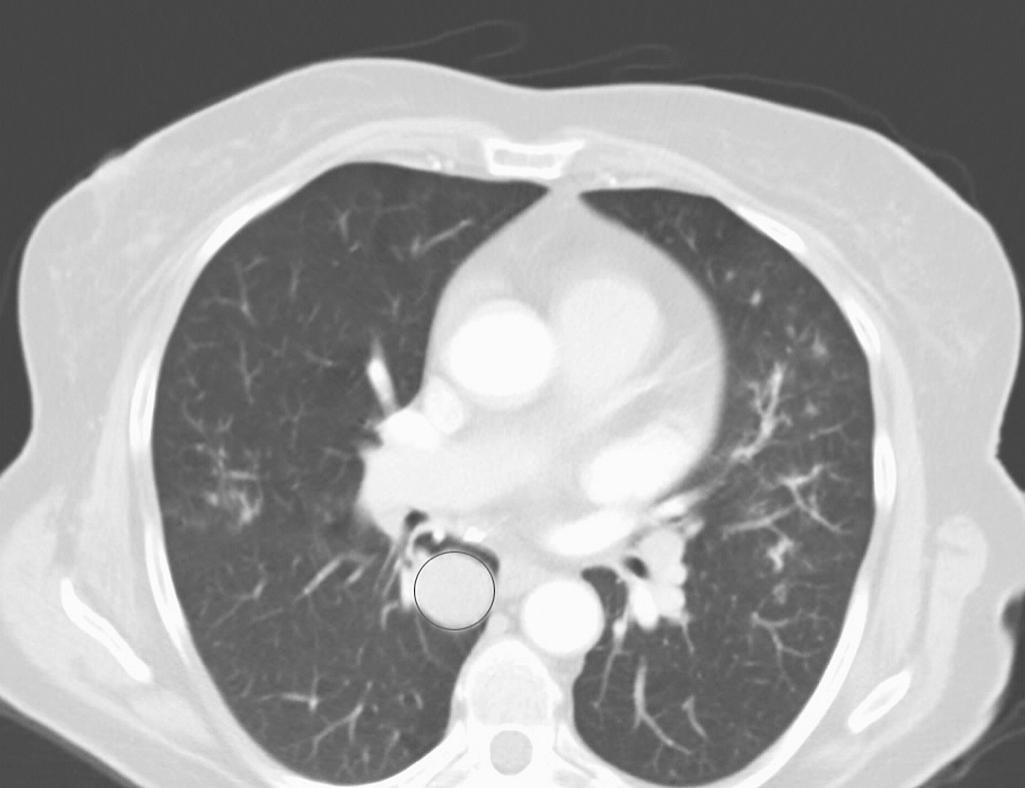
Chest radiographs (CXRs) are nonspecific for bronchopulmonary carcinoids but may demonstrate an isolated, well-defined hilar or perihilar mass, occasionally with associated atelectasis or postobstructive pneumonia. Suspicious lesions should be examined further with chest CT, which is the preferred diagnostic imaging study and which allows for determination of tumor size, location, and potential lymph node involvement. On CT, carcinoids appear as well-defined, homogeneous, spherical/ovoid, endobronchial masses ( Fig. 22-2 ) that exert mass effect or cause distal airway obstruction. Spiculation is absent. Typical carcinoids are often vascular and more commonly centrally located. In contrast, atypical carcinoids are usually located peripherally, and 30% have calcifications.
Most bronchopulmonary neuroendocrine tumors (80%) express somatostatin receptors, predominantly SST 2 receptors. Somatostatin receptor scintigraphy (SRS) with radiolabeled somatostatin analogs ( In-octreotide and In-lanreotide) can be used to locate bronchopulmonary carcinoid tumors or metastatic lesions. However, only two thirds of these carcinoids will have positive findings on SRS, and CT is generally superior for visualizing both primary and metastatic lesions. Furthermore, benign pathologic results can produce false-positive findings on SRS. Given these limitations and the superiority of CT scans, SRS should rarely be used in the diagnosis or workup of bronchopulmonary carcinoids.
The role of positron emission tomography (PET) in diagnosing bronchopulmonary carcinoids is not as well defined as that of either CT or SRS but has been investigated in several small, single-institution series and may benefit select patients. PET functions by detecting the accumulation of radiolabeled biological molecules (most commonly F-fluorodeoxyglucose [FDG]) within neoplastic cells. Historically, the use of FDG-PET has been fraught with false-negative results in patients with solitary bronchopulmonary carcinoids, because they are often hypometabolic on FDG-PET. More recently, however, FDG-PET, particularly when combined with CT, has shown improvement in the staging of select patients, particularly those with atypical carcinoid tumors. Typical carcinoids generally demonstrate significantly lower average standardized uptake values (SUVs), compared with atypical carcinoids. Chong et al reviewed FDG-PET scans of typical carcinoids ( n = 2) and atypical carcinoids ( n = 5) for maximum SUV. The typical carcinoids had an SUV range of 3.2 to 3.4, with both specimens exhibiting less than mediastinal uptake. Three of the five atypical carcinoids had a higher SUV (4.0 to 7.1) than the mediastinum. One of the five atypical carcinoids had a maximum SUV of 1.7, with an ipsilateral hilar lymph node measuring an SUV of 11.2. A further potential benefit of FDG-PET is its ability to identify lymph node and distant metastases in some cases, although it does not identify these metastases in all cases. In summary, the role of FDG-PET is evolving, and in the future it will likely play a role in the workup of select patients, particularly those with suspected atypical carcinoid tumors. Given the possibility for false-negative results in FDG-PET scans, a lesion that is suspicious for carcinoid on CT should be treated as such.
After the identification of an endobronchial or centrally located tumor, the next step in the diagnostic workup should be bronchoscopic evaluation. Rivera et al reviewed almost 3800 patients with central, endobronchial lesions and found that the overall sensitivity of flexible fiberoptic bronchoscopy for detecting lesions was 88%. As mentioned previously, most bronchopulmonary carcinoids (75%) are centrally located and are thus amenable to bronchoscopic evaluation. Recently, electromagnetic navigational bronchoscopy (ENB) has proven to be an effective means of obtaining tissue in peripheral lesions not amenable to biopsy by standard bronchoscopic techniques. In a recent study, ENB was able to establish a diagnosis in 37 of 48 patients (77%) with such lesions who were at high risk for requiring more invasive procedures. On bronchoscopic evaluation, carcinoid tumors are often smooth with a distinct reddish-brown appearance. Biopsy should be performed in an effort to establish a diagnosis, although distinguishing typical from atypical carcinoids can sometimes be challenging because of the small tissue sample typically obtained with flexible bronchoscopy. Given this difficulty and the fact that 5% to 20% of typical carcinoids and 30% to 70% of atypical carcinoids metastasize to regional lymph nodes, lymphadenectomy at the time of surgery should be strongly considered for accurate staging. Additionally, there are several cases in the literature of carcinoid tumors overdiagnosed as small-cell carcinomas on the basis of bronchoscopic biopsies. An accurate diagnosis is best achieved by careful evaluation of hematoxylin and eosin sections and mitotic index, as treatments differ radically among these separate entities.
In the past, a feared complication of bronchoscopic biopsy of carcinoid tumors was major hemorrhage; however, several more recent studies have shown this to be a rare occurrence, and biopsy is considered a safe venture. In a review of 587 biopsies by flexible and rigid bronchoscopy, there was significant hemorrhage in 15 patients (2.6%), with only 4 (0.7%) requiring emergency intervention secondary to massive uncontrollable hemorrhage. Mucosal injection of an epinephrine solution before biopsy can mitigate some of the risk of hemorrhage. In the event of significant bleeding that is difficult to control, a neodymium:yttrium-aluminum-garnet (Nd:YAG) laser is helpful. If standard bronchoscopic and ENB biopsy techniques are unable to successfully biopsy peripheral tumors, CT-guided percutaneous transthoracic needle biopsy, video-assisted thoracic surgery, and thoracotomy are other options.
Serotonin and urinary 5-HIAA are well-known markers of hormonally active carcinoid tumors; however, they are not specific for bronchopulmonary carcinoids. Chromogranin A (CgA) elevation in plasma is a relatively sensitive (75%) marker of bronchopulmonary carcinoids. Care must be taken in patients with renal impairment and atrophic gastritis and during proton pump inhibitor therapy, because these conditions cause elevations in CgA and thus false-positive results. In clinical practice, there is no evidence that measurement of tumor marker levels adds value or alters patient management; therefore, it is not routinely performed.
The TNM ( t umor, n odes, m etastasis) classification for lung cancer remains the most widely used staging classification for bronchopulmonary carcinoid tumors. Fink et al analyzed 142 bronchopulmonary carcinoids, of which 128 were typical and 14 were atypical. Lymph node metastases were less common in the subset of typical carcinoids (N0 = 87%, N1 = 10%, N2 = 3%), compared with atypical carcinoids (N0 = 43% N1 = 29%, N2 = 14%, N3 = 14%). As for other histologic variants of lung cancer, for bronchopulmonary carcinoids, N1 disease is defined as ipsilateral hilar lymph node involvement, N2 disease is defined as ipsilateral mediastinal lymph node involvement, and N3 disease is defined as contralateral or distant nodal involvement. None of the patients with typical carcinoid was found to exhibit N3 disease. Distant metastatic disease (M1) was found in 2% of typical and 21% of atypical carcinoid tumors.
A larger, more recent Italian study retrospectively analyzed 252 patients, 174 with typical and 78 with atypical carcinoid tumors, during a 38-year period and found that 96% of patients with typical carcinoids presented without nodal metastases, 3.4% presented with N1 disease, and 0.6% presented with N2 disease. In contrast, only 72% of patients with atypical carcinoids presented without nodal metastases, 17% presented with N1 disease, and 11% presented with N2 disease. Thus, typical carcinoids rarely have nodal disease, whereas atypical carcinoids commonly have either N1 or N2 disease—again highlighting the different tumor biology between these two tumors. The two previously mentioned studies and others are summarized in Table 22-2 .
| Author | Year | BP Carcinoid | Patients | N0 | N1 | N2 | 5-year Survival (Histology) | 10-year Survival (Histology) | 5-year Survival (Node Negative) | 10-year Survival (Node Negative) | 5-year Survival (Node Positive) | 10-year Survival (Node Positive) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fink et al | 2001 | Typical | 128 | 111 | 13 | 4 | 89% | 82% | n/a | n/a | n/a | n/a |
| Atypical | 14 | 6 | 4 | 2 | 75% | 56% | ||||||
| Filosso et al | 2002 | Typical | 75 | 69 | 2 | 4 | 97% | 93% | 92% | 87% | 85% | 52% |
| Atypical | 38 | 24 | 7 | 7 | 77% | 52% | ||||||
| Cardillo et al | 2004 | Typical | 121 | 107 | 14 | 0 | 99% | n/a | 100% | n/a | 90% | n/a |
| Atypical | 42 | 15 | 18 | 9 | 70% | n/a | 100% | n/a | 59% | n/a | ||
| García-Yuste et al | 2007 | Typical | 569 | 517 | 32 | 20 | 97% | 92% | 97% | 92% | 100% | 66% |
| Atypical | 92 | 59 | 14 | 19 | 78% | 67% | 83% | 70% | 60% | 60% | ||
| Rea et al | 2007 | Typical | 174 | 167 | 6 | 1 | n/a | 93% | n/a | 87% | n/a | 50% |
| Atypical | 78 | 56 | 13 | 9 | n/a | 64% | ||||||
| Total | Typical | 1067 | 971 | 67 | 29 | 89-99% | 82-93% | |||||
| Atypical | 262 | 160 | 56 | 46 | 70-77% | 52-67% | ||||||
Complete surgical resection with preservation of normal lung tissue remains the only curative treatment of bronchopulmonary carcinoids. When considering bronchopulmonary carcinoid tumors, there should be three surgical goals: (1) complete resection of the tumor (R0 resection), (2) sparing of the parenchyma whenever possible, and (3) lymph node staging by either ipsilateral lymph node sampling or mediastinal lymph node dissection.
Centrally located typical carcinoids should be resected using lung parenchyma–sparing resections, such as sleeve resection, or anatomic segmentectomy. Because local recurrence is rare, surgical treatment of typical carcinoids does not require a wide margin of resection. Ferguson and coworkers, in a multicenter retrospective study, found that wide nonanatomic wedge resection or segmentectomy was justified in the case of peripheral typical carcinoid tumors because of the low likelihood of local recurrence. Additionally, sleeve bronchial resections without parenchymal resection have been described for select patients with typical carcinoid tumors who have no evidence of nodal metastasis.
Although most agree that nonanatomic resection, when possible, is acceptable for the management of typical carcinoids, the surgical approach for atypical carcinoids is typically lobectomy or, rarely, pneumonectomy. When sleeve lobectomy is a reasonable alternative to pneumonectomy, this approach is preferred. Given the greater propensity of atypical carcinoids to metastasize to lymph nodes, a more extensive and aggressive resection (lobectomy, bilobectomy, and pneumonectomy) and nodal dissection are recommended.
Surgical resection of bronchopulmonary carcinoids should be combined with ipsilateral mediastinal lymph node dissection or sampling. The necessity of lymph node dissection is justified by the possibility of lymph node metastasis, which has an incidence of 4% to 13% in typical carcinoids and 28% to 67% in atypical carcinoids.
Endobronchial intervention using Nd:YAG laser removal or mechanical tumor removal has been described in highly selected patients with intraluminal typical carcinoid tumors, with excellent local control and low rates of recurrence. Bertoletti and colleagues conducted a study of 18 patients (all with typical carcinoid, strict endoluminal disease, and no evidence of lymph node invasion) treated with flexible bronchoscopy and cryotherapy. Patients were monitored for 55 months; there was one recurrence in 7 years, with no long-term complications. Finally, in a recent retrospective review, 25 endoscopically treated patients were compared with 48 patients who underwent surgical resection, and there was no difference in mortality. No recurrences were noted in either group. Although these results are encouraging, the current standard of care is surgical resection, and endobronchial resection should be reserved for patients who are not candidates for surgical intervention because of medical risk factors.
Bronchopulmonary carcinoids respond poorly to radiotherapy, and this treatment modality is generally reserved for use when surgical resection is impractical or as an adjunct when resection is incomplete.
There is no role for adjuvant chemotherapy following resection of a typical carcinoid tumor, regardless of lymph node status. In patients with atypical carcinoids, chemotherapy can be used as an adjunct, but response rates are typically low. The recommendations for adjuvant doublet, platinum-based chemotherapy are largely based on similar indications for other non–small cell lung cancer (NSCLC) histologic profiles and the presence of N1 or N2 disease. No clinical trials to date have specifically addressed the role, agent, or dosing regimen for atypical carcinoids.
Whereas cytotoxic chemotherapy regimens have had limited success, more recent evidence suggests that targeted therapies against mammalian target of rapamycin, vascular endothelial growth factor, and platelet-derived growth factor may be efficacious, although more clinical data are needed.
With an increase in the number of chest imaging studies performed, as well as the enhanced quality of the imaging techniques, there has been an increase in the incidence of bronchopulmonary carcinoids. Despite what could be perceived as earlier detection of all carcinoid tumors, a review of the SEER database demonstrated a decrease in the 5-year survival of patients with all carcinoids (including atypical ones) during the past 30 years. Reasons for this decrease in survival are unclear but may be related to an increase in the incidence of the atypical carcinoid histologic profile.
It is well known that typical carcinoids have a superior prognosis, compared with atypical carcinoids. This difference is primarily attributable to the differences in tumor biology between the two histologic profiles. Recent studies have shown the 5-year and 10-year survival rates for patients with typical carcinoids to be 89% to 99% and 82% to 93%, respectively. In contrast, the 5-year and 10-year survival rates for patients with atypical carcinoids are 70% to 77% and 52% to 67%, respectively.
The prognostic significance of lymph node involvement in atypical carcinoid tumors cannot be overstated and has been addressed by multiple studies (see Table 22-2 ). The 5-year survival for atypical carcinoids with node-positive disease is 59% to 60%, compared with 83% to 100% for node-negative disease. For typical carcinoids, however, the presence or absence of nodal disease does not correlate with survival.
A carcinoid tumorlet is a nodular proliferation of pulmonary neuroendocrine cells that extends beyond the basement membrane but is less than 5 mm in size; those that proliferate to greater than 5 mm are classified as carcinoid tumors. Carcinoid tumorlets and carcinoid tumors have long been associated in the literature, but a definitive relationship has not been firmly established. Studies have demonstrated the presence of tumorlets in normal lungs or in association with carcinoid tumors. There have also been case reports of isolated peribronchial and hilar lymph node metastases, which point to the possible neoplastic potential of carcinoid tumorlets. In each of these circumstances, the lymph nodes appeared normal on gross examination; however, on pathologic examination, microscopic metastases were found.
Carcinoid tumorlets develop from Kulchitsky cells, which are hyperplastic neuroendocrine cells in the bronchial and bronchiolar mucosa. Tumorlets can be single or multiple, are less than 5 mm in size, and have a carcinoid-like appearance. It has been suggested that these cells secrete neuropeptides that can elicit peribronchiolar reaction, leading to fibrotic lung disease.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here