Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Metastatic melanoma is a chemotherapy refractory disease and historical treatment options have been limited. Dacarbazine was once considered the standard systemic treatment despite a response rate of only 5–15% and having never demonstrated an improvement in survival ( ). Alternative agents such as temozolomide, fotemustine, platinum-based regimens, and combinations with interferon alpha-2b or interleukin 2 had consistently failed to make meaningful improvements ( ). As such the historical median overall survival for advanced melanoma is in the order of 6–9 months ( ).
However, since the turn of the decade, advances in our understanding of melanoma driver mutations and immune checkpoint regulation have resulted in two distinct treatment approaches that both offer meaningful improvements in survival. Ipilimumab, an antibody directed against cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4), was the first immune checkpoint inhibitor that improved the survival in melanoma. Although response rates to ipilimumab were modest (11%), it led to improvements in survival with approximately 20% of patients alive at 3 years ( ). Pooled analysis of clinical trial and community-treated ipilimumab patients has confirmed a plateau in mortality persisting beyond 10 years ( ). Recently phase III trials of another class of checkpoint inhibitors directed against programmed death-1 (PD-1) have been completed, demonstrating improved response rates and progression-free survival compared to ipilimumab ( ). Response rates to PD-1 inhibitors, such as pembrolizumab and nivolumab, vary from 33% to 44% in phase III trials with significantly less immune-related toxicity in comparison to ipilimumab. Although the overall survival of combination ipilimumab and nivolumab data is pending, PD-1 monotherapy is currently regarded as a standard of care.
Despite these impressive developments in immune-checkpoint inhibitors, there is still a need for alternative agents where immunotherapy is contraindicated or those patients in visceral crisis requiring a rapid response. This chapter will focus on the development of specific targeted agents in response to discoveries characterizing oncogenic drivers in cutaneous melanoma. In particular, mutations resulting in the constitutive activation of the mitogen-activated protein kinase (MAPK) pathway, a key regulator of normal cellular growth and proliferation, appear central to the pathogenesis of the majority of melanomas. Vemurafenib followed closely by dabrafenib are specific BRAF inhibitors that were the first successful agents to target this pathway in cutaneous melanoma. These agents have been augmented with the development of MEK inhibitors such as trametinib and cobimetinib that synergistically inhibit the MAPK pathway. Subsequent studies of BRAF and MEK inhibitor combinations have now established these molecular targeted therapies as an alternative standard of care for BRAF mutant melanoma.
The mitogen-activated protein kinase pathway (MAPK) is a key oncogenic system of melanoma progression. The classical MAPK pathway is a stepwise relay system of kinases: RAS (HRAS, KRAS, NRAS), RAF (ARAF, BRAF, CRAF), MEK (MEK1 and 2), and ERK (ERK1 and 2) ( Fig. 12.1 ). ERK, the terminal step of the MAPK pathway, is hyperactivated in the majority of melanomas and is crucial in signaling of numerous cytoplasmic and nuclear targets regulating processes such as cell proliferation, differentiation, survival, migration, and angiogenesis ( ).
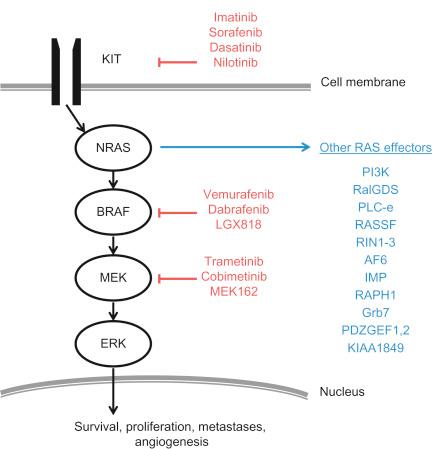
Initially extracellular ligands bind to specific membrane-bound receptor tyrosine kinases (RTK) to initiate MAPK signaling. Activation of the guanosine triphosphatase (GTPase), RAS results in phosphorylation and activation of RAF. Of the RAF kinases, BRAF is the most frequently mutated gene of the MAPK pathway with approximately 40–50% of melanoma patients harboring an activating mutation ( ). The most common BRAF mutation is a single valine to glutamine substitution at codon 600 (V600E), which accounts for greater than 75% of BRAF mutations ( ). The resultant protein possesses 10-fold greater kinase activity than wild-type BRAF and constitutively activates the MAPK pathway ( ). Other BRAF mutations have been described such as V600K (valine to lysine substitution) accounting for approximately 5–20% of patients with V600R (valine to arginine) and V600D (valine to aspartic acid) mutations both accounting for less than 5% of cases ( ). These other V600 mutations also exhibit constitutive upregulation of MAPK pathway and confer sensitivity to selective BRAF inhibitors.
Exemplifying the importance of MAPK dysregulation in melanoma oncogenesis is the recently proposed molecular classification of cutaneous melanoma into four subtypes: mutant BRAF, mutant RAS, mutant NF-1, and triple wild-type ( ). While mutant BRAF includes the aforementioned V600 mutations, other loci are also included in this subtype, including V601E, which occur in less than 1% of patients. Activating mutations of the RAS family occur in 20–30% of melanoma ( ), of which NRAS mutations involving Q61, G12, and G13 account for the vast majority (>95%) ( ). Neurofibromatosis-1 (NF-1) is a major regulator of NRAS and loss of function mutations account for approximately 10–14% of melanoma ( ). The presence of NRAS or NF-1 mutations in patients is invariably mutually exclusive of BRAF V600 mutations. Wild-type patients are primarily classified by the absence of activating BRAF, NRAS, or NF-1 mutations but may harbor KIT mutations ( ). In 10–20% of mucosal and acral melanoma cases, mutations or amplifications of KIT mutations are found ( ). These KIT mutations are potentially actionable with preexisting and novel inhibitors. Hence identification of these mutations is crucial in individualizing patient therapy in melanoma.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here