Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The term ‘operative birth’ is used to describe both instrumental vaginal delivery (also known as ‘operative vaginal delivery’ or ‘assisted vaginal birth’) and caesarean section. Operative deliveries are usually performed by obstetricians and account for a third or more of all births in most high-resource settings. Caesarean sections can be performed before the onset of labour as either elective (or scheduled) when planned, or pre-labour emergency caesarean sections when unplanned. All caesarean sections in labour are considered emergency procedures and occur in either the first or second stages of labour. Emergency caesarean sections occasionally occur after an unsuccessful attempt at instrumental delivery.
Instrumental vaginal delivery using a ventouse (also known as vacuum device) or forceps can be performed only in the second stage of labour. It is preferable that instrumental delivery is completed with the first choice of instrument. However, in circumstances in which the ventouse dislodges and the baby’s head is close to the perineum, the delivery may be completed with forceps, a situation known as ‘sequential’ instrumental delivery. The indications for operative delivery can be classified as ‘fetal’ or ‘maternal’, with a high degree of overlap. The majority of instrumental vaginal deliveries occur in women labouring for the first time. The majority of caesarean sections occur in either women labouring for the first time or women who have had a previous caesarean section.
The most common indications for instrumental vaginal delivery are suspected fetal compromise (e.g., fetal heart rate abnormalities on cardiotocography) and second-stage delay. Second-stage delay may occur as a result of maternal exhaustion, fetal malposition (occipitoposterior (OP) or occipitotransverse (OT)) or cephalopelvic disproportion (relative mismatch between the size of the fetus and the birth canal). In practice, the indication for assistance frequently includes both fetal and maternal elements; for example, a prolonged second stage of labour is often associated with fetal heart rate abnormalities. The safety criteria in Box 36.1 must be fulfilled before an instrumental vaginal delivery can be attempted.
Consent from the mother obtained
The cervix fully dilated and the membranes ruptured
The head fully engaged, at the level of the ischial spines or below, with no more than one-fifth of the head palpable abdominally
The position of the head known
The bladder empty
Analgesia satisfactory (perineal infiltration and pudendal block usually suffice for mid-cavity forceps and ventouse deliveries, but regional anaesthesia is required for Kielland rotational forceps)
Neonatal resuscitation available
Contingency planning in case delivery is unsuccessful and an emergency caesarean section is required
A careful assessment is required prior to instrumental delivery, including abdominal palpation, vaginal examination, assessment of the fetal heart rate pattern, analgesia requirements and the preferences of the labouring woman. There should be no fetal head palpable above the symphysis pubis on abdominal examination (0/5ths), although occasionally one-fifth is palpable in an OP position. One of the most difficult parts of assessment is being certain of the fetal head position prior to applying the forceps or ventouse. A systematic vaginal examination should determine the orientation of both the anterior and posterior fontanelles, as the most common mistake is diagnosing an occipitoanterior (OA) position when, in fact, it is OP. If there is a suspicion from palpation of the sutures that the fetal head is OT, it may be helpful to feel for an ear anteriorly under the symphysis pubis. The station of the fetal head should be determined relative to the ischial spines of the maternal pelvis. This is important because instrumental delivery should not be attempted when the fetal head is above the ischial spine’s ‘high station’. The degree of flexion (ideally well flexed with the fetal chin on its chest), caput (scalp swelling) and moulding (overlap of fetal skull bones), and the dimensions of the pelvis should be assessed.
Where uncertainty exists regarding the position of the fetal head, some obstetricians use transabdominal ultrasound to confirm the position; others will seek a second opinion or re-examine the woman in an operating theatre with good anaesthesia. Incorrect assessment of the fetal head position or the station of the presenting part results in a higher incidence of failed instrumental delivery and traumatic injury to the mother and baby.
Instrumental vaginal delivery requires a multidisciplinary approach to maximise the likelihood of success and minimise maternal and fetal trauma. In addition to the attending midwife, a practitioner experienced in neonatal resuscitation should be present and an anaesthetist should be available to provide adequate anaesthesia. Umbilical artery and vein acid–base status should be routinely tested and recorded immediately after delivery. This is a reflection of the oxygenation of the baby immediately prior to birth. The Apgar scores at 1 and 5 minutes reflect the early condition of the neonate and the response to resuscitation, if required. A midwife will write a contemporaneous record of the birth events and timings, and the obstetrician will complete a detailed record immediately following the procedure.
Complications include failure with the chosen instrument, resulting in either caesarean section or use of sequential instruments. Perinatal complications include low Apgar scores, fetal acidosis (on cord blood testing), cerebral trauma (haemorrhage/haematoma or skull fracture) and brachial plexus injury or skeletal fractures (clavicle or humerus) if shoulder dystocia is encountered. Maternal complications include perineal tearing that may involve obstetric anal sphincter injury (OASI, classified as third- or fourth-degree tears), postpartum haemorrhage (PPH), subsequent perineal infection, urinary or bowel incontinence, dyspareunia or subsequent fear of childbirth (tokophobia). In appropriately selected cases, the incidence of complications is low. When considering potential complications, the morbidity associated with instrumental vaginal delivery should be compared with the morbidity associated with a caesarean section in the second stage of labour, which is itself a potentially complex procedure associated with maternal and perinatal complications.
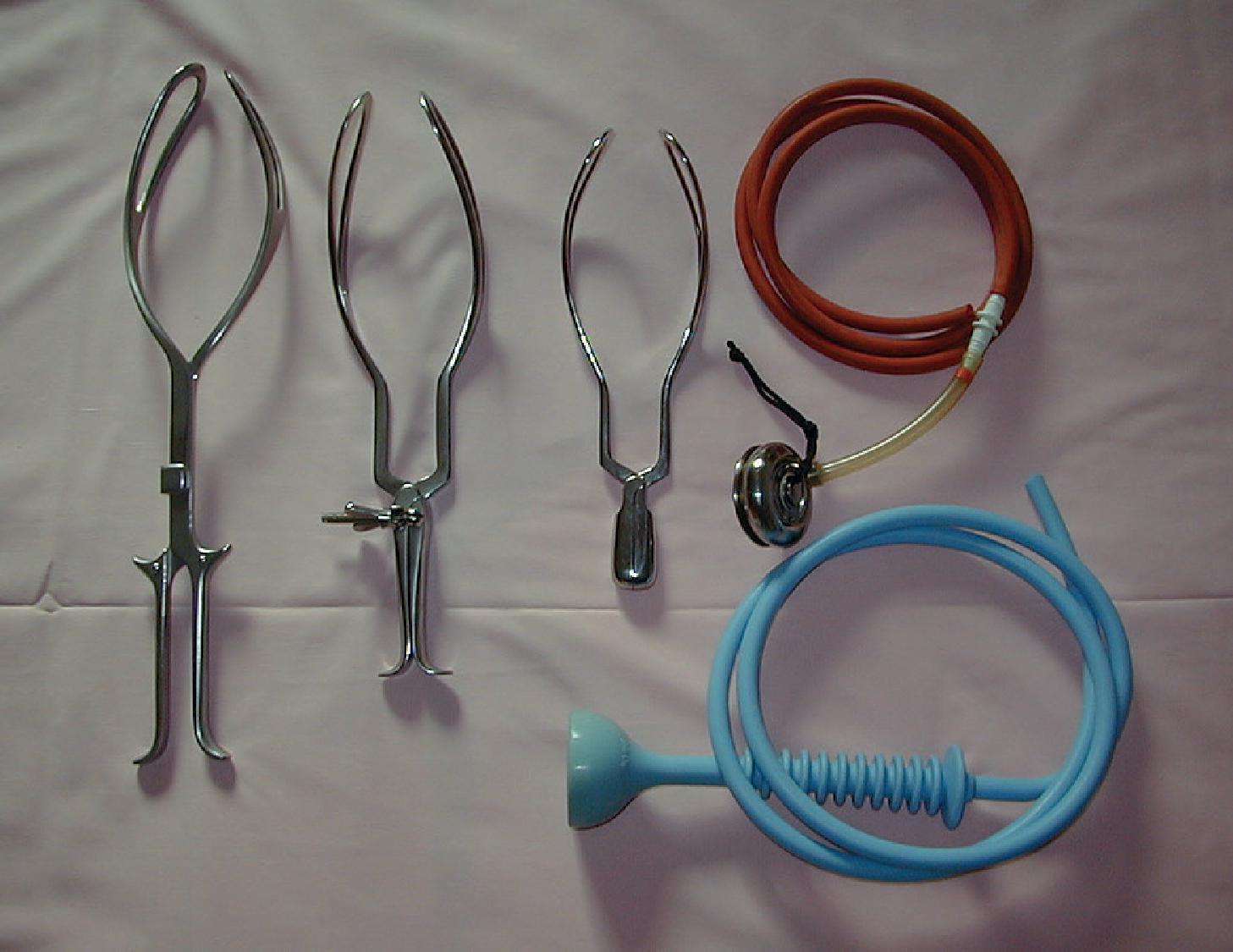
There are three main types of obstetric forceps ( Fig. 36.1 ):
Low-cavity outlet forceps (e.g., Wrigley’s), which are short and light and are used when the head is on the perineum (these forceps can also be used to assist delivery of the fetal head at caesarean section)
Mid-cavity forceps (e.g., Haig Ferguson, Neville-Barnes, Simpson), for use when direct traction is required and the sagittal suture is in the anteroposterior plane (preferably OA)
Kielland forceps for rotational delivery to an OA position from OP or OT. The reduced pelvic curve of the forceps allows rotation about the axis of the handle.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here