Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Lumbar and flank hernias are caused by defects originating in the lateral abdominal wall. Such defects can be congenital or acquired as a consequence of surgery, trauma, or progressive weakening of native tissues. There are some specific challenges associated with these hernias that require surgeons who repair them to have a profound knowledge of the abdominal wall and anatomy. First, their anatomic location is bordered by bony prominences and neurovascular structures, thus calling for the identification of important anatomic landmarks to perform a safe and efficient dissection. Second, the close location to the costal margin and iliac crest limits mesh overlap, which is a key tenet for an adequate hernia repair. Similarly, proximity to bony structures and retroperitoneal vessels, nerves, and ureter poses a challenge to obtain adequate mesh fixation along all the edges of the mesh. Consequently, understanding the unique anatomic challenges imposed by a flank/lumbar hernia is necessary to provide the patient with a durable hernia repair.
Differentiation between lumbar and flank hernias and overlapping nomenclature and classifications is confusing and can be overwhelming for the surgeon. Nevertheless, the surgical management of lumbar and flank hernias does not differ significantly. A suggested nomenclature and classification was developed by the European Hernia Society and has been endorsed by hernia societies worldwide, standardizing reporting and facilitating the communication between surgeons. Lateral hernias are those occurring lateral to the rectus sheath and linea semilunaris and involving the posterolateral abdominal wall. They occur within the limits of the costal margin (cranially), inguinal ligament (caudally), the lateral border of the rectus sheath or the linea semilunaris (medially), and the lumbar region (laterally). These are further divided into four different zones, each with its own anatomic boundaries: subcostal (L1), occurring between the costal margin and an imaginary horizontal line 3 cm above the umbilicus; flank (L2), occurring lateral to the rectus sheath and within 3 cm above and below the umbilicus; iliac (L3), between an imaginary horizontal line 3 cm below the umbilicus and the inguinal region; and lumbar hernias (L4), those located posteriorly to the anterior axillary line ( Fig. 39.1A ).
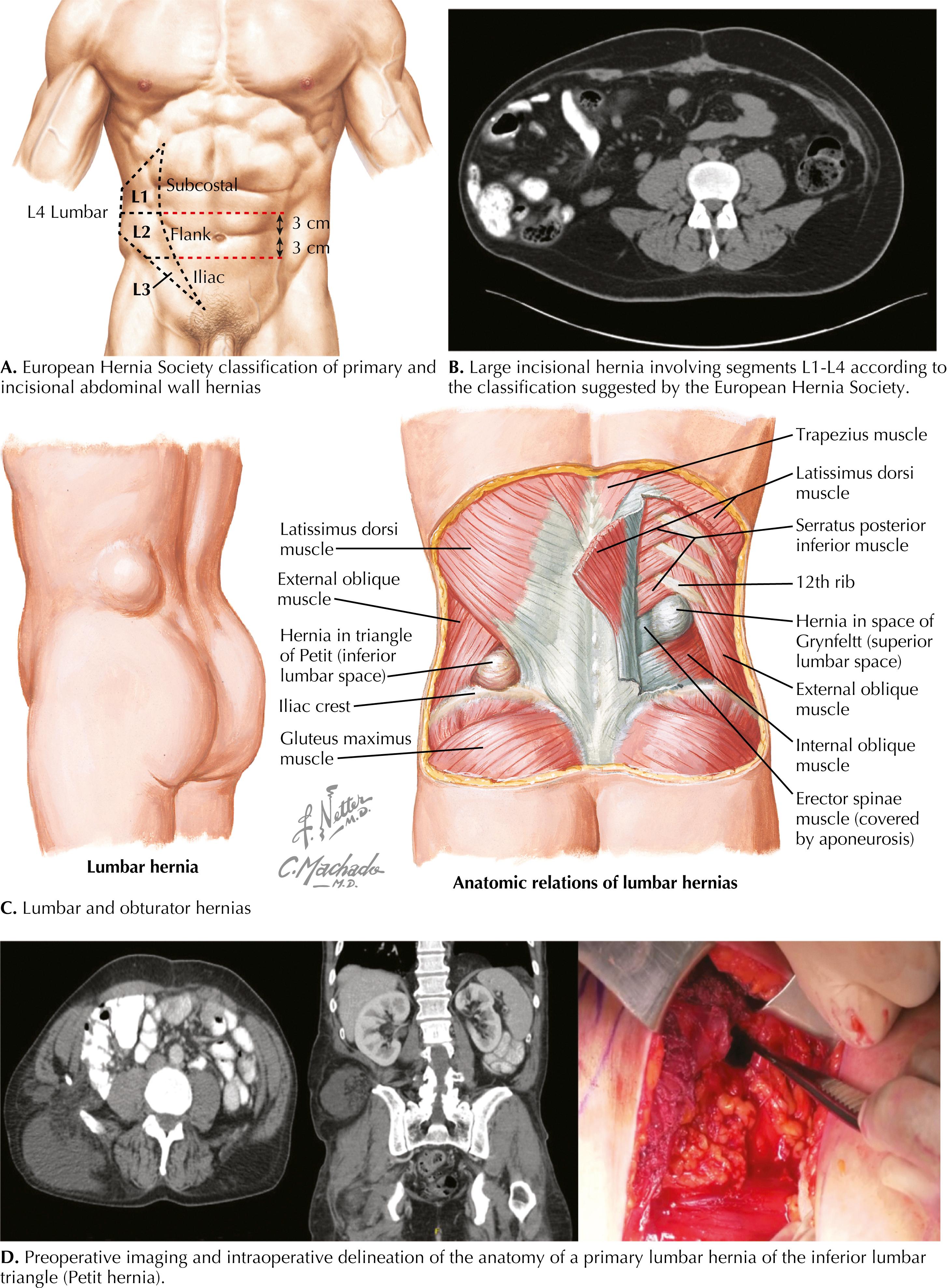
Acquired hernias, particularly after surgery or trauma, tend to be larger and often extend into more than one of the aforementioned zones ( Fig. 39.1B ). Congenital hernias are the true lumbar hernias and are usually limited to the lumbar area (posteriorly to the anterior axillary line): 12th rib superiorly, erector spinae muscle laterally, the iliac crest inferiorly, and the external oblique muscle medially. The Petit hernia occurs within the inferior lumbar triangle, which is defined by the iliac crest inferiorly, the latissimus dorsi muscle posteriorly, and the external oblique muscle anteriorly. A Grynfeltt hernia occurs below the latissimus dorsi muscle, where the superior lumbar triangle is located. Anatomic limits are the 12th rib superiorly, the erector spinae muscle posteriorly, the internal oblique muscle inferiorly, and the external oblique muscle anteriorly ( Fig. 39.1C ).
Fig. 39.1D illustrates a Petit hernia.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here