Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Antepartum hemorrhage can be a very serious complication of pregnancy. Hemorrhage may be painless or painful, and the source of the bleeding is usually maternal, but it can rarely be from the fetus. The initial evaluation must be carefully performed to first stabilize the patient, assess the well-being of the fetus, and determine the cause while establishing a plan of management.
The causes of severe antepartum/intrapartum hemorrhage are usually secondary to abnormal implantation of the placenta. The incidence of placenta previa, the most common type of abnormal placentation, is 0.5%, and bleeding from a placenta previa accounts for approximately 20% of all cases of antepartum hemorrhage. The classic presentation of placenta previa is painless vaginal bleeding in a previously normal pregnancy. Placenta accreta is a condition that occurs because of excessive invasion of the placental trophoblasts into the myometrium, resulting in failure of placental separation. This usually leads to excessive bleeding when the placenta is manually removed intrapartum. Abruptio placentae is due to premature separation of the normally implanted placenta. Placental abruption complicates 0.5-1.5% of all pregnancies (1 in 120 births). Because the bleeding penetrates into the myometrium, it is associated with pain.
Fetal bleeding may be caused by an abnormal (velamentous) insertion of the umbilical cord between the amnion and chorion and away from the placenta. When the cord insertion and placental edge are close to the cervical opening, changes in the lower uterine segment that occur before labor can cause stretching and bleeding from the cord vessels. With vaginal ultrasound and a simple bedside test to differentiate maternal blood from fetal blood, the source of the bleeding can be diagnosed.
Postpartum hemorrhage is defined as blood loss in excess of 500 mL at the time of vaginal delivery or in excess of 1000 mL for cesarean delivery. Postpartum hemorrhage is a leading cause of maternal mortality worldwide. The prevalence of postpartum hemorrhage is approximately 6% of all deliveries and accounts for 25% of all maternal deaths. Formulating a plan of management based on risk factors for postpartum hemorrhage and using intravenous oxytocin and manual uterine massage after the delivery are key elements of an effective prevention plan for postpartum hemorrhage.
When postpartum hemorrhage occurs after the patient leaves the labor and delivery area, the obstetric team must reassess the patient to identify the less common causes of delayed postpartum hemorrhage. This requires a careful search for retained products of conception and clotting within the uterus that can keep it from contracting. Other rare causes, such as uterine rupture, must also be considered.
The most common causes of maternal death are hemorrhage, embolism, hypertensive disease, and infection. In this chapter, the causes of obstetric hemorrhage in the late second trimester and the third trimester are discussed. The antepartum causes include placenta previa and accreta, conditions that represent abnormalities of placentation. Placental abruption and fetal causes of bleeding may also present before labor and may result in fetal death.
Postpartum hemorrhage (PPH) is the leading cause of maternal mortality worldwide, and its prevention is an important part of labor management. Uterine atony, genital tract birth trauma, and placental retention are the most common causes of PPH.
The incidence of bleeding in the late second trimester and the third trimester is between 5% and 8%, because bleeding before 20 weeks (time of potential viability) is usually related to the risk of abortion and the management is less emergent. It is therefore critical for the well-being of both the mother and the fetus that the patient who presents with bleeding in the late second trimester and the third trimester be evaluated and managed emergently.
After a complete history has been taken, physical examination is performed, but a pelvic examination is usually postponed until an abdominal ultrasound has been obtained to rule out placenta previa. The differential diagnosis of second- and third-trimester bleeding is listed in Box 10-1 .
The vital signs and amount of bleeding should be checked immediately, as should the patient's mental status. The patient's medical history should be checked for known bleeding disorders or liver disease, which predispose the patient to coagulopathy. Once placenta previa has been excluded by abdominal ultrasound, a sterile speculum examination can safely be done to rule out genital tears or lesions (e.g., cervical cancer ) that may be responsible for the bleeding. If none are identified, a digital examination or pelvic ultrasound may be performed to determine whether cervical dilation is present.
If a patient is bleeding profusely, a team approach to the assessment and management should be instituted to establish hemodynamic stability. This team should include an obstetrician, an anesthesiologist, and nurses who are knowledgeable about the management of a potentially critically ill patient. At least two large-bore peripheral intravenous (IV) lines should be placed, as they allow the most rapid replacement of fluid and blood volume. A central venous pressure line, or preferably a pulmonary artery catheter, is helpful in the management of hypovolemic shock.
A complete blood count should be obtained and compared with previous evaluations to help assess the amount of blood loss, although acute blood loss may not be reflected in the hemoglobin level until homeostasis has been reestablished. An assessment of the patient's coagulation profile should be done by obtaining a platelet count, serum fibrinogen level, prothrombin time (PT), and partial thromboplastin time. Additionally, the patient should be typed and crosshatched for at least 4 units of blood (packed cells). A rapid but subjective method to test for coagulopathy is to partially fill a “red-top” tube with blood. If a clot does not form, or once formed does not stay clotted, the patient most likely has disseminated intravascular coagulation (DIC).
An important and accurate method of determining the cause of bleeding in the late second trimester and the third trimester is ultrasonography. This evaluation should include not only the location and extent of the placenta (initial ultrasonic assessment to rule out placenta previa) but also an assessment of gestational age, an estimate of fetal weight, determination of the fetal presentation, and screening for fetal anomalies. Uterine activity and the fetal heart rate should be assessed with a monitored strip to rule out labor and to establish fetal well-being (see Chapter 9 ).
The incidence of placenta previa, the most common type of abnormal placentation, is 0.5%. Approximately 20% of all cases of antepartum hemorrhage are due to placenta previa. Seventy percent of patients with placenta previa present with painless vaginal bleeding in the third trimester, 20% have contractions associated with bleeding, and 10% have the diagnosis made incidentally on the basis of ultrasonography or at term.
Factors that have been associated with a higher incidence of placenta previa include (1) multiparity, which is associated with changes in the size and shape of the uterus, providing more space in the lower uterine segment for implantation; (2) increased maternal age; (3) prior placenta previa; (4) multiple gestation; and (5) cesarean delivery, which also changes the shape of the lower uterine segment. Patients with a prior placenta previa have a 4-8% risk of having placenta previa in a subsequent pregnancy.
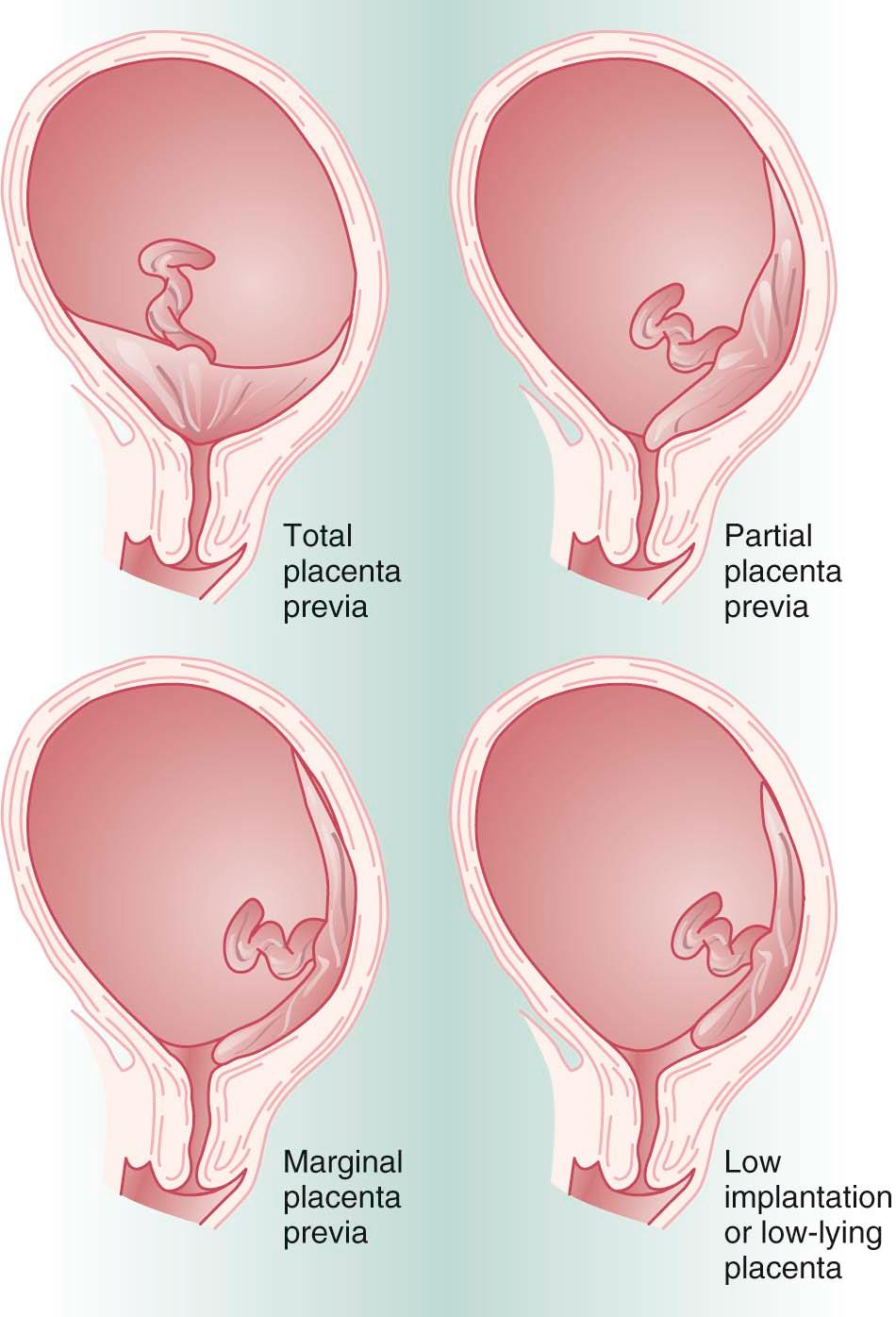
Placenta previa is classified according to the relationship of the placenta to the internal cervical os ( Figure 10-1 ). Complete placenta previa implies that the placenta totally covers the cervical os. A complete placenta previa may be central, anterior, or posterior, depending on where the center of the placenta is located relative to the os. Partial placenta previa implies that the placenta partially covers the internal cervical os. A marginal placenta previa is one in which the edge of the placenta extends to the margin of the internal cervical os.
The classic presentation of placenta previa is painless vaginal bleeding in a previously normal pregnancy. The mean gestational age at onset of bleeding is 30 weeks, with one-third presenting before 30 weeks. Placenta previa is almost exclusively diagnosed on the basis of ultrasonography. Between 4% and 6% of patients have some degree of placenta previa on ultrasonic examination before 20 weeks' gestation. With the development of the lower uterine segment, a relative upward placental migration occurs, with 90% of these resolving by the third trimester. Complete placenta previa is the least likely to resolve, with only 10% of cases resolving by the third trimester. When placenta previa is diagnosed in the second trimester, a repeat sonogram is indicated at 30 to 32 weeks for follow-up evaluation.
Transabdominal ultrasonography has an accuracy of 95% for placenta previa detection. If the placenta is implanted posteriorly and the fetal vertex is low, the lower margin of the placenta may be obscured and the diagnosis of placenta previa missed. Transvaginal ultrasonography can accurately diagnose placenta previa in virtually 100% of cases.
Once the diagnosis of placenta previa is established, management decisions depend on the gestational age of the fetus and the extent of the vaginal bleeding. With a preterm pregnancy, the goal is to attempt to obtain fetal maturation without compromising the mother's health. If bleeding is excessive, delivery must be accomplished by cesarean, regardless of gestational age. When the bleeding episode is not profuse or repetitive, the patient is managed expectantly in the hospital on bed rest. With expectant management, 70% of patients will have recurrent vaginal bleeding before completion of 36 weeks' gestation and will require delivery. If the patient reaches 36 weeks, fetal lung maturity should be determined by amniocentesis and the patient delivered by cesarean if the fetal lungs are mature. Elective delivery is preferable, as spontaneous labor places the mother at greater risk for hemorrhage and the fetus at risk for hypovolemia and anemia.
A patient with a low-lying placenta (placental margin within 2 cm of the endocervical os) may present in the same way as a patient with placenta previa. It may be difficult to distinguish a low-lying placenta from a marginal placenta previa, but a transvaginal ultrasound is typically diagnostic. Vaginal delivery is not contraindicated, because during labor the fetal head compresses the edge of the placenta, decreasing the risk of bleeding. The same level of monitoring should be maintained for maternal hemodynamic stability and fetal well-being.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here