Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
By the end of this chapter the reader should:
Have an understanding of normal child development
Understand the scientific basis of normal development
Be aware of the theory and tools available for assessment
Understand the concept of ‘red flags’ and limit ages for developmental milestones
Understand the importance of repeated developmental assessment over time
Understand the basis of the Healthy Child Programme
One of the greatest joys, and challenges, of paediatrics is that each child is truly different and will follow their own, often unpredictable, developmental path. The result is that there is a wide spectrum of skills that children of similar ages possess, and it is difficult to define what is ‘normal’. The concept of defining ‘normal’ child development arose relatively recently from statistical analysis. One of our roles as paediatricians is to know and understand the process of child development, in order to detect when a child falls outside the limits of what we would expect, and take appropriate action.
Child development encompasses both physical and cognitive change as the child grows. The child moves from a helpless and dependent infant to a mobile and exploratory child, and onwards to an increasingly autonomous adolescent. Skills and knowledge are acquired during the first few years faster than at any other time in the child's life. Developmental surveillance is designed to identify early any signs of developmental problems in order to ensure prompt access to specialist services, early intervention or therapy, and to enable the child to be supported in reaching their full potential. Developmental monitoring is carried out as part of the general Healthy Child Programme in the UK, but also by medical, educational, and allied professionals whenever contact is made. Parents themselves play a central role, and are equipped with guidance on normal child development through publications (e.g. Birth to five ) and through advice and contact with professionals such as health visitors.
If concerns are identified or suspected, a more detailed assessment is performed to look at individual areas or overall development. In order to understand the scientific basis of child development, we must first establish a few overriding concepts that explain how things occur, and the order in which they happen.
The key principles are as follows:
Development commences in the fetus and continues throughout infancy and childhood and into adulthood.
Development is influenced by both internal (genetic and child-specific) and external (environmental) factors.
Development is a varied continuum rather than a discreet set of steps or limits.
Developmental progress builds on what has been achieved before.
Development is adaptive to the circumstances and situations that the child encounters.
Below is a list of primitive reflexes normally found in infants.
Asymmetric tonic neck reflex
Babinski (extensor plantar) reflex
Galant reflex
Grasp reflex
Moro reflex
Sucking (rooting) reflex
Walking (stepping) reflex
From the list (A–G), please select the reflex BEST described by each of the following statements:
Usually the first of the primitive reflexes to disappear
Lateral curvature of the spine towards the side stimulated, disappearing by 6 months
May be present at 9 months in a normal infant
G. Walking (stepping) reflex
C. Galant reflex
B. Babinski (extensor plantar) reflex
In assessing ‘normality’ in children, paediatricians need to understand the normal natural history of the changes that occur throughout life ( Table 4.1 ).
| Reflex | Description | Age by which it should disappear |
|---|---|---|
| Sucking and rooting | Coordinated suck and swallow and turning towards the breast. May not develop until 32–36 weeks' gestation |
4 months |
| Grasp | Fist clenches when palm stimulated | 5–6 months |
| Moro | Throws head back, extends then contracts limbs and clenches fists | 5–6 months. |
| Galant | Stroking to the side of the spine causes the body to curve towards the stimulus | 4–6 months |
| Walking | Supporting the infant upright with the soles touching a surface causes each foot in turn to be lifted as if ‘walking’ | 2 months |
| Asymmetric tonic neck reflex | Extension of ipsilateral arm and contraction of contralateral elbow upon head turning (‘fencer’s posture’) | 6–7 months |
| Babinski | Extension of toes upon stroking lateral border of the foot | 2 years |
Just as a child's appearance changes from infancy through to puberty and adulthood, so does brain function. We are born with certain things ‘hard-wired’ into our nervous system that we require for survival. These are discarded when no longer useful, and new abilities take over. An example is primitive reflexes in newborn infants.
One of the first reflexes to develop in utero is the sucking (or rooting) reflex, which begins to develop around 32 weeks' gestation. Essential for feeding, premature babies may be born before this reflex is sufficiently developed and require time and practice to attain the skill. Likewise, the rooting reflex, where stimulation of a corner of the mouth/cheek prompts the baby to turn towards the source and open the mouth, makes perfect sense for helping establish breastfeeding. The grasp reflex, with clenching of the fist around whatever touches the palm, can be hypothesized as useful when observing our primate ancestry, carrying infants around clinging to their mother's fur. The Moro reflex prompts the infant to throw the head back, throw their arms and legs out wide, then clench their fists and pull the limbs in again with a cry. One theory is that this evolved as a response to an infant losing its grip on the mother and starting to fall, causing the infant to fling their arms out and grab onto the mother and pull themselves back towards her.
However, these and other neonatal reflexes diminish and disappear at different times over the first year or two. If they fail to do this, it is not only disadvantageous to the infant, but serves as an indicator to the clinician that all is not well. For example, the grasp reflex must be overcome and extinguished if the baby is to be able to voluntarily pick up and release objects and food. Another example is the asymmetric tonic neck reflex (adoption of the ‘fencer posture’, when the head turns to one side). Initially useful for coordinating gaze and upper limb extension, it becomes counterproductive if every time you turn your head your arm extends outwards on that side. Persistence of the reflex would hamper ability to bring both hands to the midline or to bring food to the mouth.
The senses allow us to experience and interpret the physical world. Although we have internal sensors that provide feedback on internal status (for example, baroreceptors and blood pressure), it is the external senses that provide the brain with information that allows us to interact with the world. Sense itself is highly individual, and the interpretation of the same stimulus may differ between individuals, or to the same individual at different times. It is also highly influenced by our emotional state at the time. An example might be the taste of coffee or wine. Both flavours are rarely liked by children, but a taste for them may be acquired as they reach adulthood. A fast-paced piece of music may be enjoyed whilst exercising, but found unpleasant when relaxing at home in the evening. Furthermore, some individuals appear to have enhanced sensitivity to certain stimuli. Children with autism often have increased sensitivity to sound, touch, and taste. This may lead them to actively seek some stimuli, but to find others intolerable. Commonly reported examples include a dislike of loud noise (leading some to require ear-defenders in noisy settings), finding certain tastes and textures of food unpalatable (leading to a restricted diet), and difficulty with things rubbing against the skin (leading to labels being cut out of clothes and items being worn inside-out to prevent the seams touching the skin).
Taste is governed by the cranial nerves VII and IX, and partly by X. Chemoreceptors in the form of papillae are distributed over the tongue and are able to detect five different tastes. Salt is an important chemical in human physiology, and it is not surprising that it is one of the main flavours we can detect. Similarly, we are designed to recognize and prefer the sweet taste that tells us that a fruit is ripe or that food is a likely source of energy in the form of carbohydrate. Sourness is usually judged as an unpleasant taste in the young child, and signals that a fruit is not ripe and so it may be unwise to eat it. Bitterness also indicates a potentially toxic substance that is best avoided. If you present sour or bitter food to an infant, it will usually be rejected outright. However, an older child is able to overcome this instinct, and actively consume sour sweets and candies.
The final taste is more difficult to define and is described in Japanese as ‘umami’. It represents the savoury or ‘meaty’ taste of foods. The receptors for this taste are activated by the food additive monosodium glutamate (MSG), which is why it is used as a flavour enhancer so widely in many parts of the world. Interestingly, the interpretation of taste seems to be affected by habituation – for example, needing to add more and more sugar or salt to foods over time in order for the full taste to be detected. Disorders causing loss of taste are relatively rare, but may occur if cranial nerve VII or the tongue surface is damaged. Smoking also seems to dull the sense of taste, but this may be more via its effects on the sense of smell.
E. Temporal lobe epilepsy.
Temporal lobe epilepsy is occasionally associated with a sudden appreciation of a smell (which is not truly present). Whilst congenital anosmia is rare (about 1% of total cases of anosmia), diagnosis is frequently delayed as the child will not understand that their sense of smell is diminished. The most common cause of congenital anosmia is Kallmann syndrome. Most cases in childhood are not permanent and relate to blockage of the nasal passages, e.g. commonly rhinoviral infection or more rarely ciliary dyskinesia. Head injury can damage the cribriform plate, severing the olfactory nerves and leading to a permanent loss.
Often overlooked, smell is one of the most powerful of the senses. It is believed to account for 80–90% of what we interpret as ‘taste’. It develops very early, and animals (including humans) rely on the smell of their mother and the mother's milk to identify a parent and to locate the nipple. Governed by cranial nerve I, the axons from thousands of cells expressing the same odour receptor converge in the olfactory bulb. We are able to distinguish the chemical signatures of an impressive range of substances. However, our sense of smell is weak compared to many other animals.
Smell is a potent emotional and memory trigger, possibly due to the olfactory system's proximity to the limbic system and hippocampus, which are involved in emotion and memory. A smell can rapidly influence our consciousness and behaviour. In animals, chemical messages in the form of pheromones are used to carry signals that are designed to influence the behaviour of other members of the same species; while best known for promoting sexual attraction, they may be competitive (e.g. ‘stink fights’ in male lemurs) or collaborative (as with ants laying down trails to food). It is unknown if pheromones exist in humans.
Temporary loss of sense of smell is very common, as with the common cold. Permanent loss can occur in head injuries, intracranial tumours, and in the genetic condition Kallmann syndrome (associated with absent or incomplete pubertal development). Some forms of temporal lobe epilepsy also trigger the sense of smell, with an odd smell prior to or during an attack. The olfactory neurons are also remarkable for their capacity to regenerate, which raises the possibility of using them to repair damaged nervous tissue in clinical practice.
Good visual function depends on a combination of good visual acuity and sensitivity to targets in the peripheral visual field. Visual acuity is defined as the minimal distance that two targets need to be separated in order to be seen as distinct. An individual with ‘perfect’ vision can resolve two targets separated by one minute of arc (i.e. one sixtieth of a degree), this is equivalent to 6/6 (or 20/20 US measurement) Snellen vision. The Snellen chart is usually viewed from 6 metres (20 yards) and this gives the numerator; the denominator is the number printed beneath the smallest line the child can read, e.g. a child with 6/36 vision is reading print which an individual with normal vision would see at 36 metres.
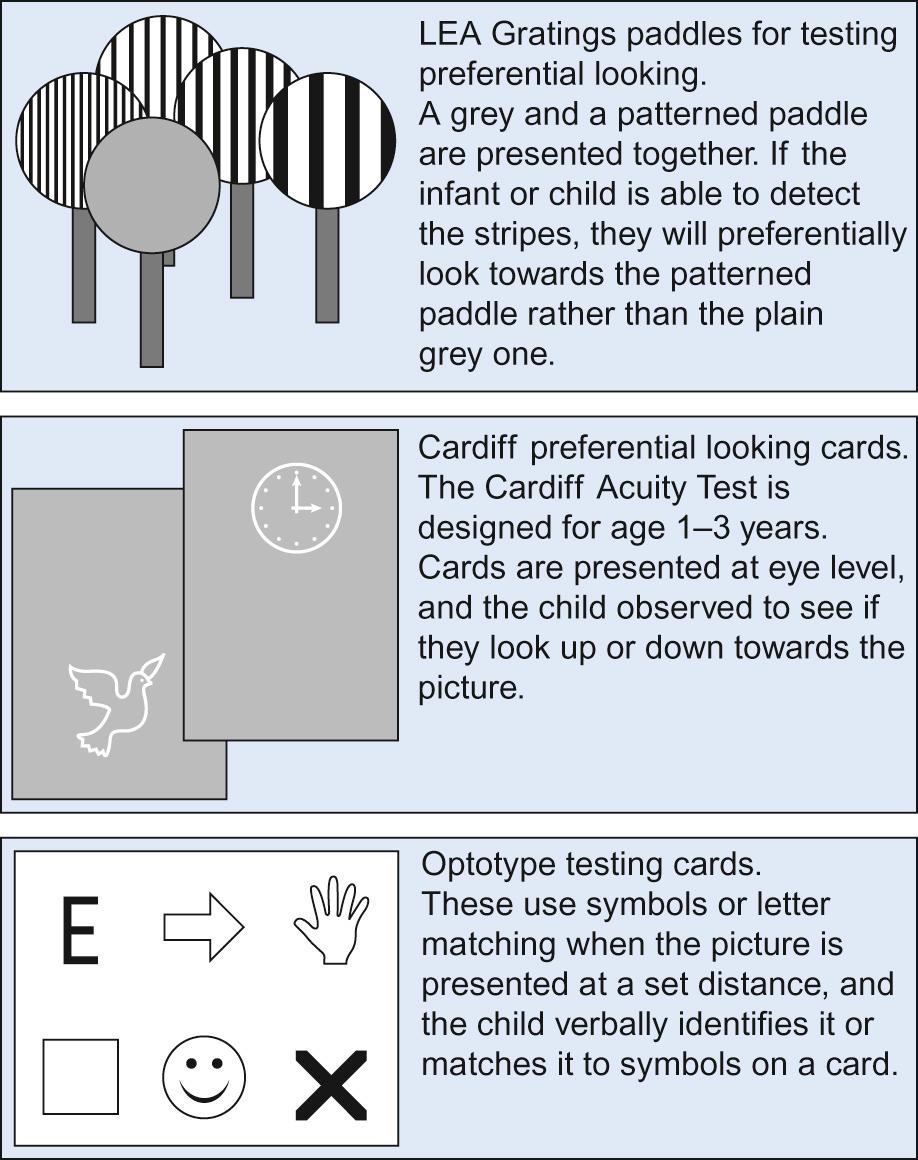
Vision is poor at birth but develops rapidly as the retina and visual pathways mature ( Table 4.2 ). Infant visual acuity is measured by visual behaviour, i.e. the ability to fixate and follow targets or the infant's natural preference to look towards a more interesting stimulus (as tested by preferential looking acuity cards). Toddlers and pre-schoolers can be tested on optotype (letter or picture) charts using matching cards ( Fig. 4.1 ). In eye departments, Snellen charts are being replaced by the more scientific logMAR (logarithmic minimal angle of resolution) charts, which have a uniform five letters per line. A logMAR score of 0.00 is equivalent to 6/6 vision; the higher the logMAR number, the worse the visual acuity. When formal visual acuity testing is not possible, smart phone apps (iSight, iChart2000) can be helpful because they are cheap and portable.
| Developmental age | Expected mean visual acuity (Snellen) | Visual acuity test | Visual field test |
|---|---|---|---|
| Newborn | <6/60 | Fixation to lights | Not possible |
| 0–3 months | 6/60–6/38 | Fixation to faces/large toys | Visually elicited eye movement Confrontation techniques |
| 3–24 months | 6/38 improving to 6/12 | Preferential looking cards (Teller/Cardiff) | |
| 2–4 years | 6/12–6/9 | Picture optotype charts | |
| 5+ years | 6/9–6/6 | Letter optotype charts | Goldmann perimetry/automated perimetry (Humphrey/Octopus) sometimes possible |
Visual acuity can also be objectively assessed using the visual evoked potential (VEP) pattern reversal test. During this electrophysiological test, skin electrodes are used to measure the cortical activity stimulated from a reversing white/black chequerboard pattern. The visual acuity is quantified by the smallest check size to elicit a cortical reaction and can be particularly useful in non-organic visual loss. Peripheral visual fields are notoriously difficult to test in young children but, by five years, a horizontal field of 150° and vertical field of 130° are expected.
Variable angle squint (ocular misalignment) is common in neonates and reflects the poor visual acuity at that stage of development. By three months, the visual acuity should be sufficient to stimulate ocular alignment. The presence of a squint after three months should alert the clinician that either the vision is poor or the squint is pathological. Ocular and cortical immaturity causes pursuit and saccadic eye movements to be jerky and inaccurate until 3–4 months of age.
Not only does what we see change as we mature, but our interpretation of it also matures. An example of this is arranging two objects on a table in front of a child, so that one partially obscures the other. If asked to draw what they see, a young child will often draw two separate objects side by side or one on top of the other. An older child will be able to marry together what they ‘know’ (they are two distinct objects) with what they ‘see’ (one object partially obscuring the other), and draw an accurate picture. Likewise, it is not until mid-to-late childhood that a child will be able to draw a scene as if from a different viewing position.
Beyond ‘red reflex’ screening of newborns, the next routine visual assessment recommended by the UK National Screening Committee is at age 4–5 years, as an orthoptist-led service. The most common condition to pick up at this age is amblyopia, which is usually treated by patching the ‘good’ eye to promote visual pathway development in the weaker eye (see Chapter 30, Ophthalmology ).
The fetus can hear from as early as 19 weeks' gestation. Reaction to low frequency sound develops first, then to higher frequency as the fetus reaches over 30 weeks' gestation. Humans are able to hear sounds between about 20 Hz and 20,000 Hz. We are able not only to distinguish many sounds, but also to determine their location by processing the difference in amplitude and timing of sound received in one ear versus the other.
Around 900 children are born each year in the UK with significant permanent hearing loss, and 1–2 per 1000 have some form of hearing impairment. All children in the UK are offered hearing screening at birth as part of the NHS Newborn Hearing Screening Programme, utilizing otoacoustic emission (OAE). If this suggests hearing loss, a further OAE and, if required, an automated auditory brainstem response (AABR or ABR) is performed (see Box 2.12 and Chapter 31, Hearing and balance ). OAE assesses the function of the inner ear, whilst AABR also assesses the auditory nerve pathway.
AABR is offered as routine alongside OAE in infants who are at high risk of hearing impairment, for example those who have been in intensive care or who had high serum levels of ototoxic drugs such as gentamicin. A clear response to testing in an infant does not rule out later hearing loss, and conditions such as chronic otitis media with effusion (‘glue ear’) are very common causes of later problems. Certain groups of patients are also at high risk and are offered extra screening: those with a family history, children with Down's syndrome, cleft palate, and those with a congenital infection.
The method used to assess hearing in children is determined by their developmental level and ability. Even small infants will usually become still and attend to a gentle rattle or bell near the ear. At around 6–9 months, an infant will actively turn to try and find the source of the sound produced by an examiner, and can be assessed using the distraction test. This test, however, is no longer in routine use.
Visual reinforcement audiometry (VRE) uses the same basic principle, but a speaker replaces the examiner as the source of the sound. Whilst the child is engaged, the speaker emits a tone. If the child stops and looks at the speaker, the examiner provides a visual reinforcement by making a toy placed on the speaker light up. Pure tone sweep testing is still performed at school entry, but may be phased out in future. Older children who can cooperate are able to have formal pure tone audiometry testing.
In addition to formal testing, any parental or school concern about a child's hearing should prompt further evaluation. Clues may be that an infant who was previously babbling has not progressed or has regressed in speech. Speech delay, speech disorders, behavioural difficulties, and social skill concerns at any age may be related to an underlying hearing problem. If a child or infant is identified with significant hearing impairment, early referral to specialist services is essential.
Bone-anchored hearing aids (BAHA) and cochlear implants have revolutionized the management of hearing disorders, and use of non-verbal communication strategies such as sign language and Makaton allow these difficulties to be overcome. The earlier a hearing loss is detected and treated, the better the outcome. Infants with hearing loss who receive sound amplification by 2–3 months (ideally by 6 months at the latest) are more likely to develop and retain the neural pathways required for later language development. Assessment of hearing and management of hearing impairment are considered in more detail in Chapter 31, Hearing and balance .
The sense of touch is the first of the senses to develop in utero . Primarily a function of the skin, the largest organ in the body, the sense of touch utilizes three different types of receptors: mechanoreceptors (sensitive to pressure and vibration), thermoreceptors (sensitive to temperature), and nociceptors (responsible for pain). Mechanoreceptors include Pacinian corpuscles (the largest, these detect vibration and large pressure change), Meissner's corpuscles (near the surface of the skin, these detect fine touch or vibration), and Merkel's discs (fine discrimination of pressure). These receptors are able to adapt to a sustained stimulus rather than firing repeatedly, hence the fact we do not feel the clothes we are wearing. Ruffini corpuscles detect changes in temperature, and can also detect stretch, as used to sense joint position and proprioception. Nociceptors are free nerve endings that signal adverse stimuli to the brain.
Piaget described four phases in normal cognitive development. The correct order is:
Formal operational, concrete operational, preoperational, sensorimotor
Preoperational, sensorimotor, concrete operational, formal operational
Preoperational, sensorimotor, formal operational, concrete operational
Sensorimotor, concrete operational, preoperational, formal operational
Sensorimotor, preoperational, concrete operational, formal operational
E. Sensorimotor, preoperational, concrete operational, formal operational. See below for discussion.
Whilst neurological structure changes with age, there are also rapid cognitive changes. The child's brain is designed to absorb and process new information, even when not being directly taught. Although children attend school and formal education, much of our learning is done beyond the classroom, through play and exploration of cause and effect. We also learn through environmental exposure, so children develop much of their language skills by hearing conversations occurring around them.
Many theories have been put forward about cognitive development. One of the best known was by Jean Piaget (1896–1980). He proposed that cognitive development could be broken down into four stages ( Box 4.1 ). Understanding the stages can help explain how a child interacts and interprets the world around them, and also informs educationalists about how best to engage and support a child with learning. As a child matures they progress through each stage in order, but some may never reach the later stages even as an adult.
Sensorimotor (0–2 years): Knowledge is based on experience and the interaction of senses and the environment. There is evolution of the concept of self as distinct from the world, and later to the concept of object permanence (the concept that an object can still exist even when out of sight – e.g. a ball hidden beneath a blanket). Use of language and symbolism appears.
Preoperational (2–7 years): The child is egocentric with difficulty seeing things from another's point of view. There is belief that all events are related to the self, animism (objects are like people, e.g. the table bumped my leg because it is mean), precausal thinking (e.g. rainbows are there because someone paints them in the sky), and magical thinking (e.g. if I say something is true, it becomes true). Symbolism and symbolic play appear, there is use of imagination, and the child has a keen interest in asking questions and gaining knowledge about how and later why things are.
Concrete operational (7–11 years): There is awareness of their own versus others' thoughts and feelings. Skills develop in the field of logic and problem-solving. There is interest in categorization, classification and lists (e.g. types of animals, football score tables, collecting things), and ability to generalize information from specific observations.
Formal operational (11+ years): This encompasses the ability to handle abstract concepts and to use deductive reasoning in problem-solving. Not all adults reach this stage.
Some measures of cognitive ability are included in standard developmental assessments used in routine clinical practice. Examples would include knowing colours, shapes and numbers, problem-solving for puzzle boards, being able to select which of two objects is bigger or smaller, or understanding concepts such as that a bird flies or that a horse runs fast. Other aspects of thinking require more specialized assessment, such as the higher cognitive functions of executive planning or understanding and using the complex social rules that govern teenage peer–peer interaction.
High quality pre-school education is associated with improved cognitive and social development. Sure Start Local Programmes, and their successors the Sure Start Children's Centres, were aimed at supporting young children and their families by integrating early education, childcare, healthcare and family support services in disadvantaged areas. The children in areas where these schemes were set up were found to have low cognitive and language development at three years of age, being on average roughly one standard deviation below the population mean. The children in these areas were followed up at 9 months, 3 years and 5 years, with a subset reassessed at 7 years. At five years, children were less likely to be overweight and had better physical health in Sure Start locations. Results at age 7 years suggested a reduction in use of harsh discipline and a more stimulating home environment as a result of the scheme. There was also an association with increased life satisfaction and other markers of function such as a less chaotic home environment.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here