Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Patients with nonsyndromic craniosynostosis are at increased risk for developing subtle neurocognitive deficits, which may or may not, be altered through surgical intervention
The goals of cranial vault reconstruction include to optimize cerebral blood flow via expansion of intracranial volume and to improve the head shape
Reconstruction is an age-dependent approach with early diagnosis simplifying and directing operative management
Surgical timing balances neurocognitive impact of disease, neurocognitive impact of interventions, and the potential need for revisional surgery
The prevailing controversy in operative management remains comparative outcomes following less invasive strip craniectomy versus open cranial vault remodeling
Outcomes can be separated into four categories: (1) measures of perioperative safety; (2) neurocognitive development; (3) aesthetic results; and (4) psychosocial development
![]() Access video lecture content for this chapter online at Elsevier eBooks+
Access video lecture content for this chapter online at Elsevier eBooks+
Single suture nonsyndromic craniosynostosis (CS) affects approximately 1 in 2000 children. The absence of a known heritable or genetic syndrome defines this subset of CS as “nonsyndromic”. The etiology of nonsyndromic CS remains unknown and is thought to be multifactorial, with emerging reports suggesting genetic predispositions. These patients represent 80% of CS cases and this incidence is 10–50 times more common than syndromic causes such as Apert and Crouzon syndromes. Surgical techniques have evolved from simple strip craniectomies to open cranial vault remodeling (CVR) procedures with improving perioperative profiles and anesthesia. Emerging less invasive techniques, including endoscopic strip craniectomy (ESC), spring-mediated cranioplasty (SMC), and distraction osteogenesis (DO), offer comparable aesthetic outcomes to CVR with improved perioperative morbidity. Unlike syndromic CS, patients with nonsyndromic CS infrequently present with intracranial hypertension (ICH). Afflicted children are at increased risk for developing subtle neurocognitive deficits, which may or may not be altered through surgical intervention. The prevailing controversy in operative management of nonsyndromic CS remains comparative outcomes following less invasive strip craniectomy versus open cranial vault remodeling. The ensuing text attempts to highlight lessons learned and long-term outcomes derived from a longitudinal experience managing these patients.
The treatment of craniosynostosis requires a longitudinal, multidisciplinary team approach during diagnosis, treatment, and follow-up. Critical team members include neurosurgeons, pediatricians, ophthalmologists, audiologists, speech pathologists, and child psychologists who work together with the craniofacial surgeon. As greater than 93% of nonsyndromic CS cases are sporadic in nature, most patients do not have a diagnosable syndrome; despite this fact, all families are offered genetic counseling, and emerging literature suggests genetics may underlie a substantial fraction of nonsyndromic craniosynostosis risk. Preoperative ophthalmologic evaluation involving fundoscopic examination and use of optical coherence tomography (OCT) may reveal concerns for intracranial hypertension (ICH), prompting more timely intervention to alter neurocognitive outcomes. Neurosurgeons serve as critical partners, as their preoperative and intra-operative assessments of the underlying brain help to diagnose functional and structural abnormalities including ICH and/or Chiari malformation.
The goals of cranial vault surgery include: (1) optimizing cerebral blood flow via expansion of intracranial volume and (2) improving head shape. In general, reconstruction is an age-dependent approach with early diagnosis simplifying and directing operative management across all nonsyndromic CS phenotypes. Surgical timing carefully balances neurocognitive impact of disease, neurocognitive impact of interventions, and the potential need for revisionary surgery. The operative technique employed further informs surgical timing. Despite the myriad of described techniques, these modalities involve either strip craniectomies or cranial vault remodeling. In general, less invasive techniques, that include endoscopic strip craniectomy with postoperative helmet therapy (ESC + PHT) and strip craniectomy with spring-mediated cranioplasty (SMC), rely on underlying rapid brain growth and the viscoelastic nature of an infant’s skull. These procedures ideally occur before 4–5 months of age. Proponents of ESC + PHT argue that suture release at an earlier age may account for improved outcomes related to subsequent craniofacial growth. In contrast, open cranial vault remodeling procedures that include fronto-orbital advancement (FOA), posterior vault remodeling (PVR), and whole vault cranioplasty ideally occur between 6 and 12 months of age when (1) the brain’s rapid growth provides an internal molding force postoperatively, (2) maturing yet malleable cranial bones allow for hardware fixation and reshaping, and (3) anesthetic risks are decreased. Beyond 18 months of age, CVR interventions may lead to persistent bony defects in an age-dependent manner presumably due to a less osteogenic dura mater.
Of the craniosynostoses, SC perhaps represents the widest disparity in surgical management. In the 1890s, Lannelongue and Lane independently proposed isolated strip craniectomies as a treatment for SC. Subsequent to operative morbidity and early re-ossification leading to recurrent cranial deformity, however, the practice was abandoned for more extensive, open cranial vault remodeling (CVR) procedures. Proponents of open CVR argue this type of intervention alone normalizes multidimensional scaphocephaly in a single stage. Specifically, CVR techniques aim to expand regions of the skull inherently restricted by an overlying fused sagittal suture (thereby increasing cerebral blood flow) while reducing regions of the skull affected by compensatory growth (i.e., frontal bossing and posterior bulleting). In contrast, proponents of endoscopic strip craniectomy procedures argue the less invasive technique offers a similar cranial expansion reliant on a rapidly expanding brain with decreasing perioperative risks.
Our institutional practice relates to timing of patient presentation. For younger infants less than 4–5 months of age, we typically recommend strip craniectomy and SMC. For older infants beyond 6 months of age, we typically recommend posterior two-thirds CVR with or without staged bifrontal orbital expansion (BFOE). Additional treatment modalities that are less frequently employed include ESC + PHT, middle vault transverse distraction osteogenesis (DO), and acute middle cranial vault expansion, depending on timing and clinical examination.
The resurgence of strip craniectomies began in late 1990s. David Jimenez and Constance Barone addressed two critical observations that re-popularized the technique: (1) most infants treated around 2–3 months of age with a simple suturectomy ultimately required CVR 6 months later for relapse in scaphocephalic head shape; and (2) open procedures were historically morbid given the scalp incisions, blood loss, and lengthy operative times involved. In 1998, they introduced endoscopically assisted strip craniectomy to limit soft-tissue dissection, thereby addressing these concerns. Although recent literature fails to demonstrate any appreciable difference in head shape with varying craniectomy widths or osteotomy patterns, several techniques emerged, with differing craniectomy widths and multiple osteotomies. In order to maintain a durable normocephalic head shape postoperatively, Jimenez, Barone, and colleagues later introduced PHT, paving the way for contemporary ESC + PHT operative modalities in the treatment of classical scaphocephaly.
The initially described operation begins with two 3-cm transverse incisions centered on the sagittal suture, one posterior to the anterior fontanelle and one anterior to the posterior fontanelle, through which subgaleal dissection occurs. The extradural space is dissected through a parasagittal burr hole. Bone scissors complete the strip craniectomy and are used to barrel stave the temporal and parietal bones to achieve transverse biparietal widening. The strip craniectomy bone is delivered through the scalp incisions and the patient starts postoperative molding helmet therapy one week later. The authors recommended a 12-month helmeting protocol consisting of three helmets during three postoperative phases. Phase one (i.e., normalization) occurs during the first two months and aims to correct scaphocephaly. Phase two (i.e., overcorrection) occurs for the next four months and aims to overcorrect the head shape into a brachycephalic range. Phase three (i.e., maintenance) occurs during the second half of the first postoperative year and aims to maintain normocephaly.
In the late 1980s, Persing and colleagues demonstrated in rabbits that springs could enhance growth when placed across a linear craniectomy. Building upon this experimental model, Lauritzen published a case report on the use of expanding torsion springs (instead of restrictive helmeting) to correct scaphocephaly. He aimed to provide a limited surgery involving insertion of springs across a suturectomy site to promote slow bitemporal widening. The springs, which push apart two bony segments in an analogous manner to conventional distraction techniques, cannot be manipulated nor their vectors altered once placed (unlike distraction techniques). The technique, which requires a second same-day surgery for spring removal, has been widely adopted and is thought to be most efficacious if applied prior to 4–5 months of age.
We have used springs for SC since 2011, and our institutional practices related to SMC are outlined below ( Fig. 25.2.1 ). Spring gauge, length, and curvature may be altered to affect resultant spring force and expansile width, with an average resultant spring force, which is confirmed on a bench-side force dynamometer, between 6 and 13 Newtons (N). Average spring expansile distance varies between 5 and 7 cm from a compressed position to a relaxed position. On the recommendation of Sood et al ., preoperative helmeting may be considered at time of initial evaluation at the craniofacial surgeon’s discretion until operative intervention in subjects with severe or worsening scaphocephaly. The procedure can be done in either the supine or prone position, and we have used a variety of minimal scalp incisions to approach the strip craniectomy, generally about 1.5 cm wide. In general, endoscopic visualization of the dura is not necessary, though can be performed if the access incisions are not providing sufficient visualization. We typically place two or three springs along the strip craniectomy segment, and out-of-plane bending of the springs allows for force distribution without tenting of the overlying skin. Springs are generally removed during a twenty-minute outpatient procedure 3–5 months after they are placed. A subgroup of patients may undergo subsequent postoperative helmeting to aid in the correction of significant saddling, severe occipital bossing, or severe frontal bossing. Our anecdotal evidence suggests improvement in eurional height following SMC, which appears to correct the posterior skull height discrepancy characteristic of SC.

In 1978, John Jane introduced the Pi procedure, which consisted of extended parasagittal strip craniectomies connected with a transverse ostectomy located behind the coronal suture extending into the temporal regions in the form of the Greek letter “π”. The procedure was the first to achieve on-table compression of the cranial length while passively expanding the cranial width. Specifically, the frontal bone and the remaining fused sagittal suture are approximated with sutures or plates to produce anteroposterior (AP) shortening and passive biparietal widening. Jane further refined his Pi procedure with the addition of parietal osteotomies to increase the biparietal diameter more actively and mitigate concerns of acute decreases in intracranial volume (ICV). The technique does not utilize postoperative helmeting therapy.
While not a standard practice at our center, the Pi procedure offers a single-stage scaphocephalic correction that may maintain more vascularized bone than some other CVR modalities. The technique, however, may not correct the cephalic index to a similar extent as other open CVR techniques and does not address orbital deformities. Regardless of the specific osteotomy design, open CVR procedures share the same goals of shortening the AP diameter, widening the biparietal diameter, reducing the frontal bossing and occipital bulleting, and expanding the intracranial volume in a single- or two-stage setting.
Conventional CVR remains the most widely performed treatment for SC, and our operative approach now involves strip suturectomy with SMC in patients presenting prior to 5 months of age and staged posterior two-thirds CVR with or without BFOE in a minority of older patients as advocated by Fearon.
Our center’s CVR technique was initially described in 2002 by Weinzweig et al . The specific form of vault remodeling was based on the underlying phenotype (i.e., anterior, posterior, or a combination). For patients with anterior and posterior pathology, reshaping typically occurred in two stages with posterior and middle vault reconstruction followed by BFOE or vice versa. With the patient in the prone position, posterior two-thirds remodeling begins with a tongue and groove osteotomy of the synostotic sagittal suture and parietal bone flaps overlying the vertex. Ultimately, these bone flaps will be transversely widened, interdigitated, and transferred to the occiput, thereby raising the posterior cranial height, transversely expanding the posterior vault, and shortening the AP dimension minimally. The bulleted occipital bone flap is radially osteotomized, flattened, and transposed to the vertex. Anterior barrel-stave osteotomies, generally carried out to the coronal suture region, further blend the anterior and posterior bone segments. This two- to three-segment osteotomy PVR technique relies on removal of bone down to the basicranial ring (i.e., cranial base) to effect a desirable change in posterior head shape.
In general, patients treated by our PVR technique by 18 months of age rarely require frontal surgery; however, nearly 50% of patients presenting in the delayed fashion do not undergo auto-remodeling of the frontal region and therefore benefit from anterior vault reconstruction. Not only is the scaphocephalic phenotype more severe in these late-presenting patients, but the biparietal narrowing often results in fronto-orbital deformity. Our center’s technique for BFOE typically performed in delayed patient presentations involves transverse expansion of the frontal bone and supraorbital bar with interpositional bone graft harvested posterior to the coronal sutures, which simultaneously achieves further AP diameter reduction.
All SC may not present with classical scaphocephaly amenable to relatively standardized strip craniectomy and vault remodeling procedures. Morritt et al . previously estimated that atypical non-scaphocephalic SC comprises ~4.0% of all isolated SC in their practice. Lee et al . further described cranial distraction interventions specific to varying phenotypes by changing the vectors of the bone flaps in the AP and biparietal directions. Patients presenting with classic scaphocephaly with increased head circumference (HC) and cephalic index (CI) <0.75 underwent a 1- to 2-cm bicoronal strip ostectomy with two distractor devices placed for AP compression and a midsagittal osteotomy with two to three distractor devices placed for biparietal expansion. Patients presenting with normocephaly with a normal HC and CI between 0.75 and 0.80 underwent midsagittal osteotomy with placement for two to three distractor devices to achieve biparietal expansion and a bicoronal osteotomy when anterior and posterior cranial expansion requirements differed. Patients presenting with a decreased HC and CI >0.80 underwent bicoronal and midsagittal osteotomies with distractor placement to expand in the AP and biparietal dimensions. While not a standard operative practice for SC at our center, there may be certain technical advantages worthy of discussion, including maintenance of dural–endocranial vascularity, minimization of extradural dead space through gradual expansion, and progressive expansion of the overlying soft tissues.
Middle vault expansion serves as a viable alternative to DO for the treatment of late-presenting normocephalic SC. The technique involves elevation of bilateral parietal bone flaps without elevation of the mid-parietal bone overlying the fused sagittal suture to prevent further blood loss and surgical risk. Temporal and occipital barrel staves further expand the cranium. At our institution, we use a hinged biparietal tongue and groove osteotomy pattern with anterior and posterior barrel-stave osteotomies to further expand the cranium while maintaining temporoparietal dural–endocranial vascularity.
Single-stage TVR remains a viable option when patients present with severe scaphocephaly (i.e., frontal and occipital deformities, bitemporal narrowing, decreased CI, anteriorly located vertex, and narrow sloping occiput). Building upon Jane’s Pi technique, Persing and colleagues introduced whole-vault cranioplasty in 1989 as a form of active CVR that achieved an immediate intra-operative scaphocephalic correction. Whole-vault cranioplasty begins in the modified prone position (i.e., sphinx) with chin support in a padded “bean bag” to allow simultaneous access to the anterior and posterior skull – a position initially popularized by Persing and colleagues. A series of sequential craniotomies are performed to elevate bifrontal, separate parietal, and biparietal occipital bone flaps. Radial osteotomies into the occipital and bifrontal flaps allow for flattening of the occiput convexity (i.e., “bullet”). Triangular wedges of frontal bone are resected laterally to allow for more posterior inclination of the forehead. A 10- to 15-mm strip of midline frontoparietal bone is removed to achieve anteroposterior shortening and further posterior inclination of the newly remodeled forehead. Laterally oriented barrel-stave osteotomies in the temporal bones allow for biparietal widening. The parietal bone flaps are remodeled to maintain the newly created lateral convexity. Excessive bifrontal bossing resulting from overgrowth of the underlying frontal lobes may necessitate dural plication. The parietal bone flaps are connected to the underlying dura but not to surrounding bone, essentially creating parasagittal “neosutures” that allow for further biparietal widening during brain growth and development.
Nearly 20 years later, Holmes and colleagues described the Melbourne method of TVR similarly aimed to address all the phenotypic aspects of severe scaphocephalic deformity in a single operation through vertical occipital elevation and simultaneous anteroposterior shortening. Unlike the sphinx position classically described with Persing’s whole-vault cranioplasty, the procedure begins in the supine position on a horseshoe headrest that allows for full rotation to access the occiput from multiple approaches. A precoronal bifrontal bone flap is transposed posteriorly to reduce frontal bossing and widened in the bitemporal dimension through lateral barrel-stave osteotomies. The coronal suturectomy strip is bisected in the midline, widened laterally, and lowered centrally to widen the mid-vault constriction. A 3- to 4-cm coronal strip posterior to the native coronal sutures is rotated 90° and positioned along the inferior occiput to increase the deficient vertical height of the posterior vault. The deformed occipital bone including a 3- to 4-cm sagittal suture strip is elevated en bloc , widened posteriorly through barrel-stave osteotomies, and fixated inferiorly to the newly repositioned posterior coronal strip. Anteroposterior shortening is achieved through fixation of the en bloc sagittal and occipital bone flap to the bifrontal bone flap. The parietal bone flaps are reshaped and replaced to broaden the biparietal region. In 30 consecutive patients undergoing the Melbourne TVR technique at mean age 7.5 months, the authors reported a 12.9% mean increase in CI.
Fusion of the metopic suture prior to 7–9 months of age leads to a continuum of phenotypes ranging from a mild metopic ridge to severe trigonocephaly with hypotelorism. Given the variability in presentation, a variety of surgical techniques exist, including synostectomy, “le front flottant”, and fronto-orbital expansion with interposition bone grafts. At our institution, as in the majority of the developed world, bifronto-orbital advancement and remodeling (BFOAR) remains the most widely practiced method of treatment to improve frontal aesthetics, correct the hypoteloric orbit, and expand the frontal cranium to allow brain growth to resume along a more normal trajectory.
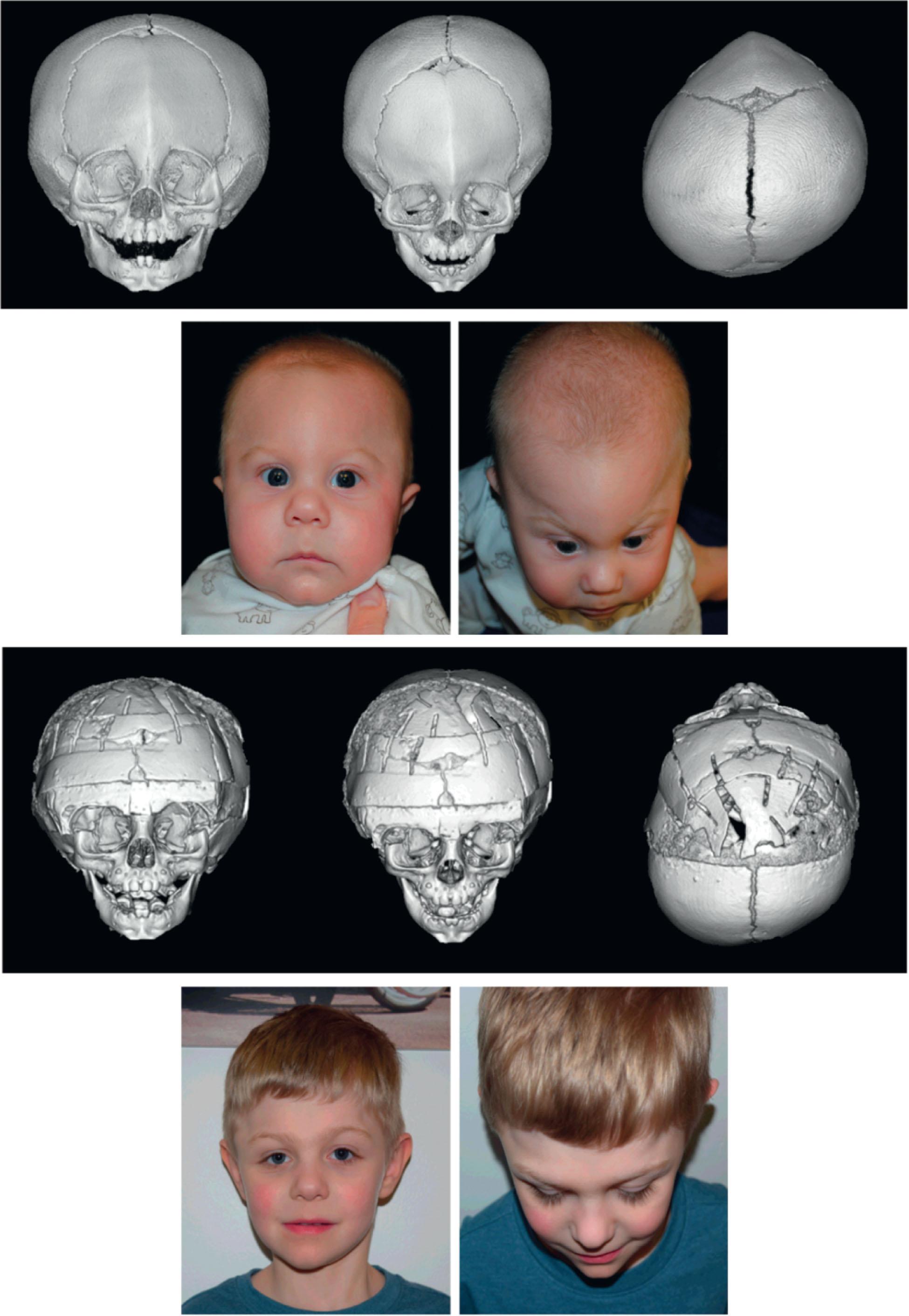
We have previously outlined in detail our center’s evolutionary operative approach to BFOAR correction of trigonocephaly ( Fig. 25.2.2 ). All operations involved a bicoronal incision, subgaleal versus subperiosteal scalp dissection, release of the bilateral temporalis muscles as separate units, and subperiosteal dissection of the orbits. The initial technique involved opening of the supraorbital bandeau with wire or titanium plate fixation. The technique evolved with the use of an interposition calvarial bone graft to expand the bandeau, thereby increasing the bitemporal and interorbital distances and creating a more obtuse endocranial angle. The next evolutionary step included lateral orbital kerf-style (i.e., closing wedge) osteotomies with resorbable fixation placed along the inner aspect of the construct to stabilize the reconstruction. To buttress further the interposition bone graft expansion of the central supraorbital bar, we introduced placement of additional calvarial bone graft along the posterior aspects of the central and temporal bandeau. The bandeau is secured by resorbable sutures at the zygomaticofrontal and nasofrontal regions, and resorbable plates and screws temporally. Most recently, we include placement of inlay strut grafts of cranial bone that are “press-fitted” by grooves created within the expanded superior orbital roof. The supraorbital bandeau reconstruction aims for overcorrection, as there is an anticipated loss of bandeau growth potential relative to continued overall cranial growth.
The in situ hinge technique for the supraorbital bandeau represents a nuanced, iterative approach to simplifying BFOA. Realizing that the temporal tenon of the supraorbital bandeau was invariably fixated in its original position, the senior author began to maintain the temporal tenon laterally into the temporal bone. The remainder of the operation is unchanged from the BFOA technique. Although there may be increased difficulty with lateral bandeau reshaping (i.e., lateral orbital kerf-cuts, bone-bending, etc.), the technique has been shown to decrease operative time, decrease hardware utilization and cost, and result in similar postoperative shape correction. A limitation of the technique relates to its inability to correct significant alterations in bandeau pitch and yaw, which would require a conventional bandeau release and reconstruction.
Forehead shape and expansion are largely determined by the new position of the supraorbital bandeau, as the forehead passively follows the cranial base. We consequently customize the frontal bone contours to the newly reshaped, expanded, and advanced bandeau (i.e., basicranial segment). The frontal bone is typically halved, bent, reshaped, and orthotopically replaced depending on the position of the newly reshaped bandeau. This frequently requires interposition bone graft harvested from the posterior aspects of the frontal bone flaps to further aid in frontal expansion. Lateral canthopexy is variably performed (~19% in our last published series). Again, surgical “overcorrection” remains the primary goal, as we anticipate some degree of long-term relapse.
Advocating for earlier surgical intervention, Jimenez and Barone argued that once the physical examination findings characteristic of severe CS develop, it is impossible to correct. Since the primary deformational force in single sutural synostosis was the suture itself, the authors believed early suturectomy during the phase of rapid brain growth would halt progression and potentially correct the deformity. Their described technique begins with a 2- to 3-cm incision made over the midline between the hairline just anterior to the anterior fontanelle. An ~7-mm-wide strip of bone is removed, which extends along the entire length of the stenosed metopic suture to the nasofrontal junction. The incision is closed and the patient undergoes up to 10–12 months of postoperative helmet therapy beginning on postoperative day 5.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here