Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
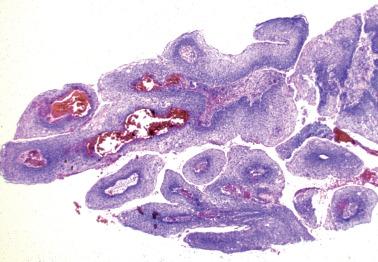
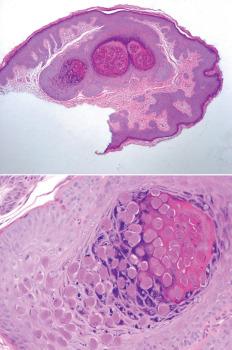
Sexually transmitted HPV (usually low-risk types, especially HPV 6 and 11) is the cause of condyloma acuminatum (venereal wart), the incidence of which in the USA increased 4- to 5-fold between 1966 and 1981.
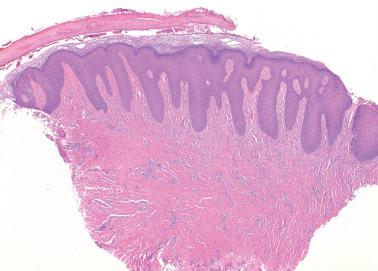
Condylomas, which are considered LSIL/VIN1, most commonly involve the vestibule and the medial aspects of the labia majora and vary from only colposcopically visible lesions to small excrescences to large, sessile or pedunculated, white to red, cauliflower-like masses that may be multiple or confluent.
Synchronous or metachronous condylomas, precancerous changes, or invasive squamous cell carcinoma (ISqCC) may occur locally, including the perineal and perianal skin and the mucosa of the anus, urethra, vagina, and cervix.
The clinical course is typically protracted unless the lesions are ablated or removed. They may enlarge and increase in number during pregnancy but can regress postpartum.
Srodon et al. found that condylomas harbored a low-risk HPV in 67% of cases, but 42% contained a high-risk HPV that may account for the progression of some condylomas to high-grade VIN or ISqCC.

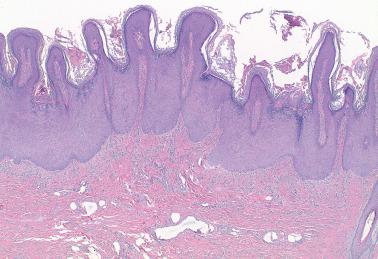
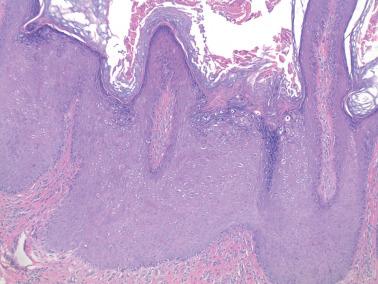
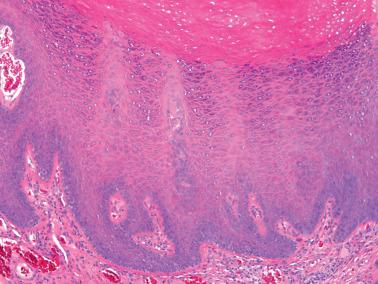
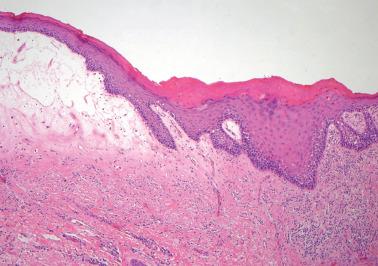
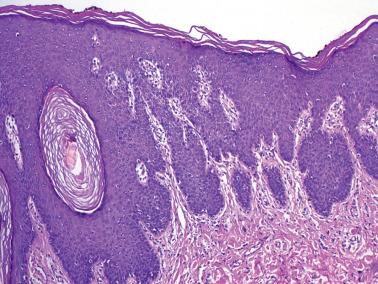
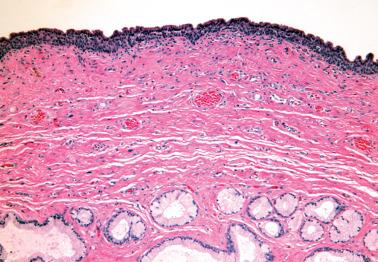
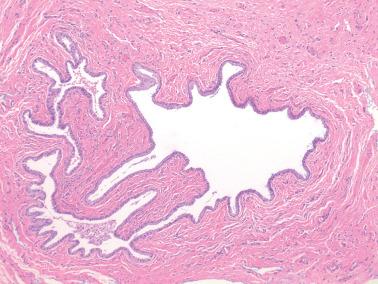
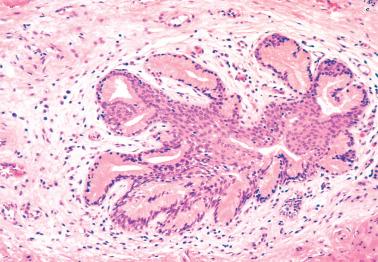
Fully developed condylomas are characterized by simple to complex branching papillae of acanthotic squamous epithelium and fibrovascular cores. Flat condylomas occur but are less common in the vulva than in the cervix (see Chapter 5 ).
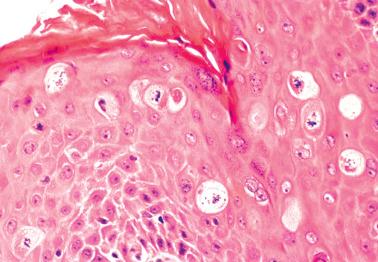
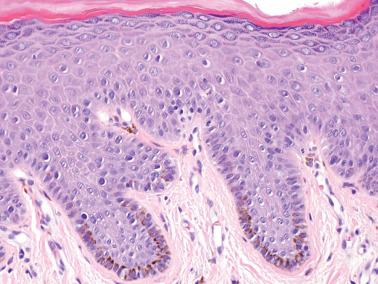
The pathognomonic koilocytes (HPV-infected keratinocytes) in the superficial layers are usually prominent but may be focal or even absent. ‘Condyloma without cytopathic effect’ has been applied in the latter situation, but ‘squamous papilloma, possibly condyloma’ may be preferable given the implications of a condyloma diagnosis.
The variably sized koilocytes have a perinuclear halo of clear cytoplasm typically surrounded by a peripheral zone of condensed amphophilic cytoplasm. Their hyperchromatic, granular or smudgy, enlarged to shrunken nuclei have an irregular contour (‘koilocytotic atypia’); binucleated or multinucleated cells are common. Occasional mitoses, usually confined to the lower third of the epithelium, may be seen.
Ki67 expression is present in the upper two-thirds of the epithelium and correlates with the presence of HPV.
p16 staining is typically focal, cytoplasmic, and often in the upper layers (consistent with LSIL), although rare condylomas harbor foci of HSIL (as noted above) with typical diffuse (block) p16 staining (Sulaiman et al.) necessitating thorough sampling. Lewis et al. found focal block p16 staining in 4% of lesions they considered flat vulvar LSILs, although most investigators equate block staining with HSIL.
Nonspecific features include para/orthokeratosis, hypergranulosis, parabasilar hyperplasia, and underlying superficial chronic inflammation.
Variant condyloma phenotypes:
Seborrheic keratosis (SK)-like condyloma. HPV+ SK-like lesions have also been referred to as ‘condyloma with features of SK’ (see Seborrheic Keratosis ).
Condyloma with pseudobowenoid change. Apoptosis in the superficial keratinocytes with chromatin dispersal or clumping and cytoplasmic condensation and retraction results in a dense hyaline globule (the residue of a dead cell). The appearance may suggest VIN, but nuclear atypia and mitotic activity in the lower layers are absent.
Epidermodysplasia verruciformis-like condylomas. Pohthipornthawat et al. described this flat condyloma variant in immunosuppressed women (with β papilloma virus type 5 infection) that exhibited acanthosis, variable hyperkeratosis, and enlarged cells with blue-gray cytoplasm, and occasional perinuclear halos. Atypical nuclei are found only superficially or extending through the full epidermal thickness.
Podophyllin treatment results in mitotic arrest in the lower epidermis, karyorrhexis, and cellular swelling. In contrast to VIN, nuclear atypia is mild and confined to the upper layers. A history of recent treatment is obviously helpful.
Verruca vulgaris (HPV type 2) infection:
Aguilera-Barrantes et al. found that 41% of vulvar warts in girls <5 years of age contained HPV 2 (likely nonvenereal), the remainder HPV 6/11 (vs 3% HPV 2 and 94% HPV 6/11 in adults).
HPV 2-related vulvar lesions resembled typical verruca vulgaris including marked hyperkeratosis.
HPV testing of vulvar warts in children can be diagnostically helpful.
Squamous papilloma (vs condyloma with loss of koilocytosis). Ki-67+ cells in the upper epithelial layers indicate condyloma.
Vestibular papillomatosis (see corresponding heading). These squamous papillomas are typically confined to the vestibular area, are usually smaller than condylomas, and typically lack koilocytosis and hyperkeratosis.
Condyloma lata (see Syphilis ).
Epidermolytic hyperkeratosis. This lesion exhibits acanthosis, compact papillomatous hyperkeratosis, and dissolution of the suprabasilar epithelium resulting in perinuclear clear zones. Keratohyaline clumping and dyskeratosis resulting in intracellular eosinophilic globules facilitate distinction from condyloma.
Warty VIN and warty ISqCC. Unlike typical condylomas, these lesions ( Chapter 2 ) have nuclear atypia and mitoses in all epithelial layers, typically strong and diffuse ‘block’ p16 staining, and in some, invasion.
Verrucous carcinoma ( Chapter 2 ). These usually large solitary highly differentiated SqCCs occur in older women and are usually HPV-negative. They lack the fine branching papillae and koilocytosis of condylomas and have a well-circumscribed deep border formed by broad bulbous pegs.
Papillary SqCC, NOS. These lesions are rare in the vulva and are composed of obviously malignant cells that lack koilocytosis.
Most cases of herpetic vulvitis are due to sexually transmitted herpes simplex (HSV) type 2, or less commonly, HSV-1.
The clinical presentation can include vulvar pain, inguinal lymphadenopathy, malaise, and fever, with sequential appearance of vesicles, pustules, and painful ulcers, often with synchronous involvement of the perineum, perianal skin, cervix, vagina, and urinary tract.
The lesions persist for 2–6 weeks and heal without scarring. Rarely, chronic hypertrophic herpetic vulvitis clinically simulates a neoplasm or harbors carcinoma.
Detection of HSV-2-specific antibodies is diagnostic. Antibodies in many women without a history of infection indicate that subclinical infections are common.
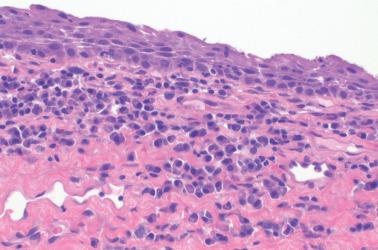
A smear or biopsy of a new lesion reveals the characteristic ground-glass nuclei or eosinophilic intranuclear inclusions. Cells infected by HSV-1 or herpes zoster have a similar appearance.
Recurrent episodes are common but are usually much milder, often inconspicuous, and become less frequent.
Vulvitis secondary to herpes zoster (varicella) infection is rare, usually occurring in postmenopausal women who present with vulvar pain usually followed by unilateral vesicles and ulcers. Recurrent similar episodes are common.
Cytomegalovirus (CMV) causes an ulcerative vulvovaginitis resembling herpetic infection; HIV+ women are most susceptible. Characteristic CMV-inclusion bodies in epithelial and endothelial cells are detectable with routine and immunohistochemical stains, culture, or by PCR.
Molluscum contagiosum can be venereally transmitted resulting in vulvar and perineal lesions that are often asymptomatic and overlooked by patients and physicians. The histologic features are similar to those involving extravulvar sites.
Human immunodeficiency virus (HIV) is cultured from some genital ulcers in HIV+ women, and may cause or exacerbate genital ulcers in this population.
Epstein–Barr virus is a rare cause of painful vulvar ulcers and may be associated with mononucleosis.
Vulvar syphilis is rare. The primary lesion or chancre forms within days or several months of initial contact. The secondary phase is evident by 6 months as a mucocutaneous rash and papules (condyloma lata). Tertiary lesions (gummas) are uncommon.
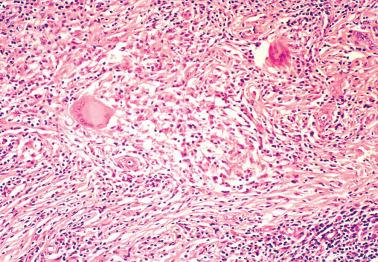
Chancres are superficial ulcers whereas condylomata lata are nonulcerated lesions with marked acanthosis and papillomatosis, often accompanied by intraepidermal neutrophils. In both lesions, a perivascular plasmacellular infiltrate with endothelial proliferation suggests the diagnosis.
Organisms can be confirmed by a Warthin–Starry stain. Dark-field examination or immunofluorescent staining of lesion-derived serum and serologic studies can also facilitate the diagnosis.
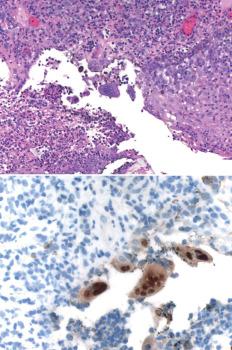
This disorder is caused by the gram-negative bacterium Calymmatobacterium granulomatis . The primary lesions (vulvar, vaginal, cervical) are painless papules or ulcers that appear within a month of exposure (sexual contact or fecal contamination).
The ulcers can persist for years and mimic a neoplasm, including ISqCC. Lymphatic spread can result in brawny vulvar edema or parametrial or retroperitoneal involvement.
Unlike lymphogranuloma venereum, inguinal lymphadenopathy is uncommon but can be mimicked by inguinal abscesses that often ulcerate.
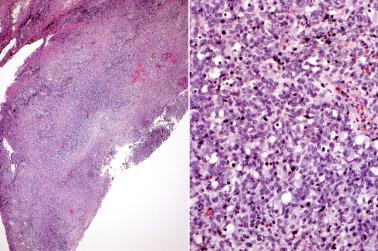
Granulation tissue with neutrophils, plasma cells, and vacuolated histiocytes contain coccoid to bacillary organisms (Donovan bodies) demonstrable within the vacuoles by Giemsa or Warthin–Starry staining of tissue sections or touch imprints, or by culture.
This venereal disease is caused by Chlamydia trachomatis . An initial ulcer is followed by painful inguinal lymphadenitis (buboes) that can rupture and drain through the skin. Later, chronic lymphatic obstruction can result in nonpitting vulvar edema and vaginal and rectal fibrosis (sometimes with strictures).
The inflammatory infiltrate is nonspecific (lymphocytes, plasma cells, histiocytes including giant cells). Diagnosis rests on the characteristic clinical findings, culture, immunostaining, and complement fixation tests.
This venereal disease, which is caused by the gram-negative bacillus Haemophilus ducreyi , presents with painful, often purulent, vulvar ulcers and tender inguinal lymphadenopathy.
The ulcer consists of a superficial zone, a middle zone with characteristic vascular changes, and a deep zone with a lymphocytic and plasma cell infiltrate.
Gram stains of tissue sections or smears may reveal the organisms in the superficial zone but definite diagnosis requires culture identification.
Vulvar tuberculosis is rare and usually due to direct or lymphatic spread from other sites in the FGT that are usually due to blood-borne spread from pulmonary tuberculosis.
The lesion begins as a nodule that later ulcerates and may drain caseous material and pus through one or more sinuses. Epidermal hyperplasia may result in a warty tumor-like mass (hypertrophic tuberculosis).
There is typical granulomatous inflammation with caseation. Diagnosis requires acid fast stains and/or culture or molecular testing to identify the organisms ( Mycobacterium tuberculosis or occasionally atypical mycobacteria).
Nontuberculous mycobacterial infection can clinically mimic invasive cancer as exemplified by a cervical case in an immunocompetent woman (Ukita et al.).
The differential includes noninfectious forms of granulomatous vulvitis (see corresponding heading).
Vulvar involvement by these disorders, which represent mixed synergistic bacterial infections, is often associated with diabetes mellitus and/or atherosclerosis.
Necrotizing fasciitis presents with vulvar erythema, edema, and pain, followed by rapidly progressive dark discoloration, bullae, and necrosis of the skin, subcutaneous tissue, and fascia; toxic shock syndrome is a rare complication. Fatalities can occur without prompt excision of involved tissues and antibiotic therapy.
Progressive synergistic gangrene, unlike necrotizing fasciitis, is a slow process that can involve fascia with less severe systemic manifestations. It is more likely to develop in postoperative wounds, whereas necrotizing fasciitis is prone to develop at sites of minor injury.
Infection of Bartholin's gland (bartholinitis) is usually caused by sexual transmission of Neisseria gonorrhoeae or Chlamydia trachomatis ; occasional cases follow vulvovaginal operations. Complications include Bartholin's abscess (sometimes with secondary infection by anaerobic bacteria) and, rarely, toxic shock syndrome.
Hidradenitis suppurativa is a chronic suppurative process of the vulvar and inguinal apocrine sweat glands that often results in scarring and draining sinuses. Microscopic examination reveals acute and chronic inflammation and apocrine glands dilated with keratinaceous material. Chronic cases have been complicated by SqCC.
Rare cases of vulvar bacillary angiomatosis occur and can result in a mass. Microscopic examination reveals a lobular epithelioid vascular proliferation and bacteria ( Bartonella henselae or Bartonella quintana ) that stain with the Warthin–Starry method.
Erythrasma, a chronic infection of the vulvar and perianal skin, is due to the bacterium Corynebacterium minutissimum , and usually diagnosed by Wood's lamp examination.
Rare cases of vulvar malakoplakia, involvement by Actinomyces israelii, or botryomycosis have been reported.
Chronic fungal infections of the vulvar and perianal skin are commonly caused by Candida albicans and dermatophytes. Vulvovaginal candidiasis results in pruritic, moist, red lesions that exhibit spongiosis and intraepithelial and dermal neutrophils. PAS or GMS stains and cultures can confirm the diagnosis, but a paucity of organisms can cause false-negative results.
In developed countries, rare vulvar parasitic infestations include enterobiasis, schistosomiasis, and myiasis, the last due to infestation of the larva of the muscoid fly and sarcophaga. Enterobiasis and late cutaneous vulvar schistosomiasis can elicit striking pseudoepitheliomatous hyperplasia that can mimic SqCC if the organisms are not appreciated. These diseases are common in certain parts of the world.
* Formulated by the International Society for the Study of Vulvar Disease (ISSVD) and the International Society of Gynecological Pathologists (ISGyP).
Lichen sclerosus
Squamous cell hyperplasia
Other dermatoses
Lichen sclerosus (LS) accounts for 30–40% of non-neoplastic epithelial vulvar lesions. It may occur at any age, including in children, but is most common in postmenopausal patients.
The etiology is unknown, but recent evidence indicates that it is a chronic T-cell-mediated inflammatory dermatosis.
LS is associated with autoantibodies and in some cases systemic autoimmune diseases, such as autoimmune gastritis, Hashimoto's thyroiditis, and extragenital psoriasis.
Up to 50% of cases have a monoclonally rearranged T-cell receptor γ-chain gene, the T-cells having an immunoprofile of an antigen-mediated immune response.
A familial occurrence and HLA class II DQ antigen restrictions in some cases suggest genetic factors.
Hormonal factors may play a role. Some patients have low serum levels of dihydrotestosterone, free testosterone, and androstenedione, and respond to topical testosterone. Lagerstedt et al. found that ~80% of childhood-onset and ~50% of adult-onset LS had decreased ERα staining.
LS may be asymptomatic but often causes pruritus, burning, and dyspareunia. Any part of the vulva can be involved by irregular, ill-defined, white patches. Focal red and brown areas can be due to dilated vessels and melanin incontinence, respectively. Synchronous vulvar lichen planus is present in some cases (see Differential Diagnosis).
Hart et al. found that the labia minora were involved in 68% of cases, the labia majora in 60%, the clitoris in 51%, the perineum in 41%, and the posterior fourchette in 36%. Almost 90% of the lesions are multiple. Bilateral, sometimes symmetrical, lesions are common.
Vaginal involvement occurs in rare cases. Extragenital lesions occur in two-thirds of children with vulvar LS, but in only about 10% of adults.
Longstanding LS in adults can result in shiny and wrinkled skin, atrophic labia, a narrowed introitus, and agglutination and scarring of the prepuce and frenulum that may obscure the clitoris. Complications, especially in children, include anal fissures and perianal and genital ulcers.

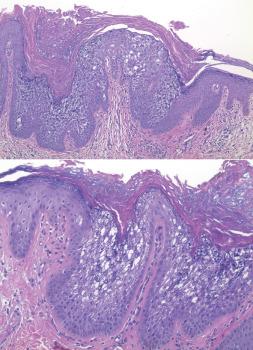
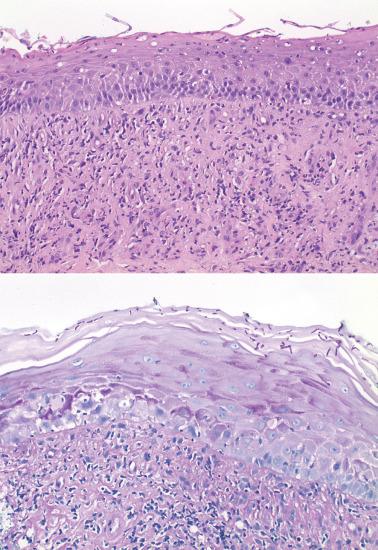
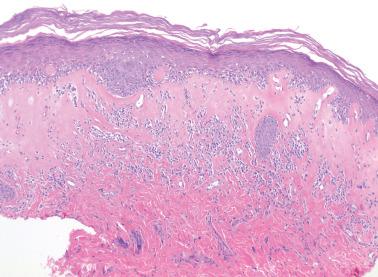
Well-developed lesions exhibit a subepithelial edematous to hyalinized zone with a loss of elastic fibers, usually subtended by a band of lymphocytes.
Additional findings may include spongiosis, vacuolar alteration and squamatization of basal keratinocytes, intraepithelial lymphocytes, prominent thickening of the basement membrane, and sclerosis and/or ectasia of dermal vessels.
A perivascular lymphocytic infiltrate and a lymphocytic vasculitis occurs, respectively, in up to two-thirds and half of vulvar LS, but can be focal and subtle ( ).
‘Hypertrophic’ LS, characterized by prominent dyskeratosis and parakeratosis, was found in 20% of cases encountered by Weyers, mostly in elderly women. Unlike differentiated VIN (dVIN), there was no significant atypia, nuclear crowding, mitotic activity, or subsequent SqCC.
Associated lichen simplex chronicus and/or squamous hyperplasia are more common than in extravulvar LS and can result in detached dermal squamous cell nests that may suggest invasion. Unlike the latter, the nests lack atypia, are confined to the abnormal collagen, and are not associated with dVIN ( Chapter 2 ).
Subtle findings in early LS, which may lead to underdiagnosis, include preferential involvement of adnexal structures with acanthosis and luminal hyperkeratosis and hypergranulosis. A thickened basement membrane may be appreciable, particularly with a PAS stain.
The presence of dyskeratosis and parakeratosis, hyperplasia, and/or basal cellular atypia (but less than in dVIN [ Chapter 2 ]) should be noted, one study finding that >50% of LS cases associated with ISqCC had basilar atypia.
The basal cells are typically p53+, usually with a discontinuous pattern (unlike dVIN). In hypertrophic LS, the suprabasilar cells may also be p53+. Sadalla et al. found that p53 expression in LS did not predict progression to SqCC.
Lichen planus (LP) (also see Other Dermatoses).
Genital involvement by LP can be difficult to distinguish from early LS and the two lesions may be synchronous. Day et al. suggest that when one lesion is present or suspected the presence of the other should be considered with separate biopsies from morphologically distinct areas.
Cytoid bodies, wedge-shaped hypergranulosis, basal squamatization, and pointed rete ridges favor LP, but these findings are less common than in extravulvar LP.
dVIN (vs LS with basilar atypia) ( Chapter 2 ).
Postradiation fibrosis. A history of radiation is obviously helpful. This diagnosis is also favored in the presence of more diffuse (vs band-like) fibrosis, atypical fibroblasts and endothelial cells, and thick-walled vessels.
Spontaneous remission may occur at puberty or postpartum. In some cases, the lesions respond to topical testosterone or corticosteroids.
There is strong evidence that LS is a premalignant lesion; Davick et al. found that the proportion of women with vulvar ISqCCs who had ever had a diagnosis of LS was 36%. Longitudinal studies indicate that up to 5% of cases of LS progress to vulvar ISqCC.
found that women with LS have a lifetime cumulative risk for vulvar ISqCC of 15% compared to only 0.06% for women in the general population.
Up to 65% of cases of dVIN and ISqCC are associated with synchronous LS.
Some LS lesions are monoclonal and exhibit an increased frequency of allelic imbalance.
found a monoclonal γ-T-cell receptor rearrangement in LS-associated ISqCC, but not in uncomplicated LS, suggesting that local immune dysregulation in LS promotes development of ISqCC.
The frequency of p53 mutations and aneuploidy is higher in LS associated with ISqCC than in uncomplicated LS.
Patients with LS, particularly those with acanthotic or atypical LS, should be monitored for the development of SqCC.
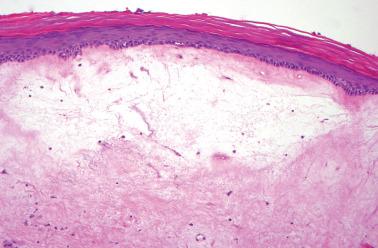
The term ‘squamous cell hyperplasia, NOS’ (SCH), which replaced the term ‘hyperplastic dystrophy’, refers to epidermal hyperplasia not attributable to more specific dermatologic disorders and lacking dysplasia.
SCH has been found adjacent to 40% of SqCCs, in 20–50% of patients with a clinical diagnosis of vulvar dystrophy, and in about a third of patients with LS.
A white plaque-like thickening of the involved skin may be seen clinically. The thickened epidermis may show hyperkeratosis or parakeratosis. There is normal maturation from the basal to superficial layers. Atypia is usually absent, and its presence should suggest dVIN ( Chapter 2 ). Mitotic figures, if present, are confined to the basal and parabasal zones.
There is some evidence to suggest that SCH, if not directly premalignant, may be an early stage in vulvar carcinogenesis:
The lesion may abut or merge with dVIN and/or SqCC.
Monoclonality and an increased expression of p53, p53 mutations, and allelic imbalance occur in some lesions, especially in those with synchronous SqCC. Some lesions have contained HPV, yet all cases studied by Santos et al. were p16-negative.
Patients with SCH, like those with LS, need to be monitored for the possible development of dVIN or ISqCC.
Almost any dermatosis can involve the vulva (see review by Greene and Dulaney and review of vulvar lichenoid dermatitis by Lewin et al.), the most common being lichen simplex chronicus, spongiotic dermatitis, psoriasis, and lichen planus.
Lichen simplex chronicus is a common vulvar dermatosis that can follow or coexist with a wide variety of irritative and infectious factors.
The clinical manifestations include pruritus and burning and a leathery skin with scaly plaques and accentuated cutaneous markings.
Microscopically there is psoriasiform hyperplasia (with rete ridges that are thicker and more variable in length than in psoriasis), hypergranulosis, hyperkeratosis, and occasionally, focal parakeratosis. The papillary dermis is thickened; collagen bundles may be arranged vertically, parallel to the rete ridges. Scattered dermal inflammatory cells may be present.
Vulvar (or vulvovaginal) lichen planus can be erosive and lead to scarring and stenosis. Associated pseudoepitheliomatous hyperplasia may rarely progress to SqCC. The differential diagnosis between lichen planus and lichen sclerosus is considered under the latter heading. The differential between erosive lichen planus and differentiated VIN is discussed under the latter heading ( Chapter 2 ).
‘Vulvar acanthosis with altered differentiation’ is a lesion often associated with vulvar verrucous carcinoma (see latter heading in Chapter 2 ).
Squamous papillomatosis (squamous micropapillomatosis, vestibular papillomatosis) refers to multiple, often countless, squamous papillomas that typically involve the medial aspect of the labia minora, vulvar vestibule, hymen, introitus, and urethral meatus.
Women of reproductive age are typically affected. They are usually asymptomatic, although occasionally there is pruritus, burning, or dyspareunia. The lesions usually regress spontaneously.
The etiology is unknown; most studies have not found an association with HPV. A study finding a high frequency of HPV included koilocytic lesions that most would consider condylomas.
The papillomas are ~1 mm in diameter and 1–8 mm in length and consist of bland, nonkeratinized, glycogenated squamous epithelium and a fibrovascular core. Absence of koilocytosis (a definitional feature in most studies) and a low Ki-67 rate (staining confined to basal layer) allow distinction from condyloma.

Benign pigmented vulvar lesions, which occur in about 10% of women, often have atypical clinical and/or histologic features that may suggest malignant melanoma.
Lentigo simplex refers to a lesion exhibiting benign epidermal hyperplasia, hyperpigmentation, and benign melanocytic hyperplasia. The term ‘melanosis’ is most commonly used to refer to similar hyperpigmented lesions, with or without melanocytic hyperplasia, that lack epidermal hyperplasia.
The lesions, which typically occur in Caucasians of reproductive age, may have been longstanding. Melanotic macules involve the labia, introitus, or perineum. Lentigines are usually <5 mm, whereas areas of melanosis may reach 2 cm.
Occasionally the features suggest or mimic lentigo maligna or malignant melanoma, including multifocality, an irregular margin, and variegated pigmentation.
Microscopically, there is basilar hyperpigmentation and basilar melanocytic hyperplasia without nesting or atypia. However, as noted above, some lesions designated ‘melanosis’ have lacked melanocytic hyperplasia. Acanthosis with elongation of rete pegs is present in lentigines; dermal melanophages also may be present.
The differential is with malignant melanoma in situ that, unlike lentigo or melanosis, exhibits transepidermal nests of atypical melanocytes that may exhibit mitoses.
Vulvar nevi are only a third as common as the lesions considered in the preceding section, being found in only 2–3% of women. Most resemble their extravulvar counterparts.
Some vulvar melanocytic nevi overlie or are entrapped by the sclerosis of lichen sclerosus and may resemble persistent melanocytic nevi.
Michalova et al. described dVIN-like changes (atypical basal keratinocytes) overlying anogenital melanocytic nevi. These foci showed normal p53 immunoreactivity in contrast to diffuse or null p53 staining in dVIN.
Vulvar nevi with atypical features that differ from those of the usual dysplastic nevus have been referred to as ‘atypical melanocytic nevi of genital type’ or ‘atypical genital nevi’ (AGN). AGN may have striking architectural and cytologic atypia, but are clinically benign.
Gleason et al. found a median patient age of 26 (range, 6–54) years and no site predilection.
A lentiginous or nested junctional component exhibits variability in the size, shape, and position of the nests, including a confluent band-like arrangement.
In addition to the usual location at the rete tips, the nests may be seen on the sides of rete or between the rete and adnexal structures, often with a retraction artifact around the nests and/or cellular dyscohesion within the nests.
Pagetoid involvement of the upper epidermis may occur, but in contrast to melanoma, the lesional cells are usually focal or multifocal rather than extensive or diffuse, and lack cytologic atypia and lateral extension. However, atypia of the cells in the junctional component is present and was moderate to severe in 80% of cases in the Gleason study.
An underlying, often large, common dermal nevus is often present that is diffusely or focally covered by the junctional component.
The cells in the dermal component may show atypia, but which is less common and less severe than that of the junctional component; mitotic figures are rare and maturation is typically present.
A broad zone of dense fibrosis within the superficial dermis is present in 40% of cases, but usually lacks the distinctive lamellar pattern seen in dysplastic nevi.
AGN must be distinguished from vulvar dysplastic nevi and superficial spreading melanoma (see Clark et al. and Gleason et al.).
These lesions are most common in the vagina and are discussed in Chapter 3 .
Obstruction of the vestibular orifice of Bartholin's duct results in a cyst filled with secretions. The usual presentation is a lateral introital mass that may be asymptomatic or associated with dyspareunia.
The cysts are lined by squamous, transitional, mucinous, ciliated, or flattened nonspecific epithelium. Acute and chronic inflammation is often present. One cyst had melanocytic colonization (Nigam et al.).
A location consistent with Bartholin's origin (posterior lateral to vaginal introitus) and/or normal Bartholin's gland acini adjacent to the cyst facilitate distinction from cysts arising from minor vestibular glands (see below).

These cysts typically present as a solitary (or occasionally multiple), sometimes painful, subcutaneous mass on the inner surfaces of the labia minora in the reproductive age group.
The cysts are usually <3 cm in size and are lined by a single layer of columnar mucinous epithelium, ciliated nonmucinous epithelium, squamous epithelium, or admixtures thereof. The lining cells may be ER+ and PR+.
The cysts have traditionally been presumed to arise from the minor vestibular glands in the anterior and posterior vestibule. To account for the typical location of the cysts, Scurry et al. suggest that minor vestibular glands likely also occur at the vulvar mucocutaneous junction (Hart's lines).
Vulvar epidermal inclusion cysts are common, and usually within the labia majora. They are lined by stratified squamous epithelium and filled with keratinaceous debris.
Vulvar epidermal inclusion cyst formation may occur following female genital mutilation. Reports have documented cyst formation as a delayed late complication, and these can present as large cysts that may clinically mimic clitoromegaly or a neoplasm.
Rare mesothelial cysts derived from the canal of Nuck (the incompletely obliterated processus vaginalis) are usually found in the superior aspect of the labia majora or the inguinal canal. They may be associated with, and should be distinguished from, an inguinal hernia.
Rare mesonephric cysts occur in the lateral aspects of the vulva and histologically resemble vaginal mesonephric cysts ( Chapter 3 ).
Rare vulvar cysts may arise from the mammary-like glands in this site (see Other Non-neoplastic Lesions ).
Vulvar vestibulitis (aka ‘provoked localized vulvodynia’ [PLV]) affects up to 15% of women in a general gynecologic practice, who are typically of reproductive age.
The typical feature is point tenderness of the vulvar vestibule in the absence of other identifiable causes; dyspareunia is also usually present. Vulvar erythema is seen in some cases. Munday et al., however, have concluded that the clinical features are nonspecific and part of a continuum within the general population.
The etiology is unknown and possibly multifactorial. HPV is usually absent or present with a frequency similar to that of control patients.
Proposed pathogenetic factors include an increased number of vulvar nerve fibers, hypersensitivity to seminal fluid, deficiency of interferon-α, deficient ER expression, and enhanced synthesis of proinflammatory cytokines produced by vestibular fibroblasts.
The histologic findings, which have varied between studies, can support the diagnosis, but generally the latter rests on the typical clinical findings.
Some studies have found a mild to severe chronic inflammatory infiltrate (T lymphocytes, plasma cells, and occasional B lymphocytes, mast cells, monocytes), including lymphoid follicles, in the superficial dermis and surrounding the vestibular glands and ducts.
Leclair et al. found that primary PLV specimens had more CD4+ T cells than secondary PLV specimens and unaffected controls, findings noteworthy given that CD4+ T cells are recruited by infectious, allergic, or autoimmune triggers.
Bornstein et al. found an increase in subepithelial mast cells, heparinase, and peripheral nerve fibers compared to asymptomatic women.
Squamous metaplasia of the vestibular ducts and glands is an occasional finding, but may not be an inherent feature of the disorder. Complete replacement of the vestibular glands and ducts by squamous epithelium producing an invagination or cleft was considered a diagnostic feature in one study, whereas two other studies found clefts to be uncommon and difficult to distinguish from infoldings of surface epithelium.
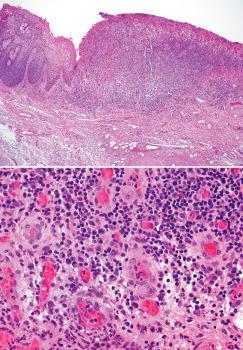
This idiopathic lesion typically presents with pruritus, burning, and red, sometimes multiple, macules.
Histologic features are a predominantly plasmacellular lichenoid infiltrate, a thinned epidermis, flattened rete ridges, absence of the granular/keratin layers, spongiotic parabasal keratinocytes with spindled horizontal nuclei (‘lozenge keratinocytes’), and prominent dermal blood vessels with hemorrhage and hemosiderin.
The differential includes syphilis, lichen planus, and other chronic dermatoses.
Isolated granulomatous vulvitis is idiopathic and likely the vulvar counterpart of granulomatous cheilitis; occasional patients have both lesions.
It occurs over a wide age range and usually presents as a labial mass or hypertrophy. Histologically, there is edema, fibrosis, lymphangiectasia, a mononuclear infiltrate, and non-necrotizing granulomas with giant cells.
More common than isolated granulomatous vulvitis, but identical histologically, is vulvar involvement by Crohn's disease.
There is usually a history of or synchronous intestinal Crohn's disease; rarely the vulvar involvement precedes bowel involvement.
Patients presenting with granulomatous vulvitis therefore need to be evaluated for Crohn's disease.
Behçet's disease is a systemic vasculopathy that is most frequent in Japan and eastern Mediterranean countries. The mean age at onset is in the third decade; there is a slight male predominance.
The disease is diagnosed by the presence of oral ulceration and any two of genital ulceration, skin lesions (pustules or erythema nodosa-like lesions), and eye lesions (uveitis or retinal vasculitis). Synovitis and meningoencephalitis may also occur.
The vulvar (and oral) ulcers are of minor or major aphthous or herpetiform type. Major aphthous ulcers, which may lead to gangrene, heal by scarring, but are often followed by new ulcers.
A necrotizing neutrophilic or lymphocytic vasculitis can involve all calibers and types of dermal and subcutaneous vessels and be accompanied by mural fibrin deposits, mural necrosis, and thrombosis.
This rare lesion has clinicopathologic features like those in the cervix ( Chapter 4 ). One vulvar case was associated with infectious mononucleosis and presented as a 1 cm crusted lesion on the labium minus.
The vulvovaginal area is the most common site in the female genital tract for GVHD (a complication of bone marrow transplantation).
The most frequent symptoms include vulvovaginal dryness, discharge, discomfort, ulceration, scarring, a narrowed or obliterated introitus and/or vagina, and dyspareunia that develop at a mean interval of 10 months after transplantation.
Vulvar biopsies show changes similar to cutaneous GVHD, including ulceration, apoptotic bodies in the epidermal basal layer, and chronic inflammation. Vaginal biopsies show inflammation, apoptotic bodies, and fibrosis. The cervical mucosa and endometrial glands may also show apoptotic bodies.
These patients are also at higher risk for condylomas and HPV-related neoplasms.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here