Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The histiocytoses are a group of disorders characterized by the proliferation of macrophages and dendritic cells. The contemporary classification of histiocytic disorders (a classification proposed by the Reclassification Working Group of the Histiocyte Society and the World Health Organization Committee on Histiocytic/Reticulum Cell Proliferations) divides them into three groups: dendritic cell–related disorders, macrophage-related disorders, and malignant disorders. In 2008, the World Health Organization classified neoplasms of histiocytes and dendritic cells according to their putative normal counterparts. These entities are covered in Chapter 53 . In this chapter, we discuss the non-neoplastic proliferations of histiocytes and their differential diagnosis. Box 52-1 lists the disorders discussed in this chapter.
Reactive sinus histiocytosis
Sinus histiocytosis with massive lymphadenopathy
Hemophagocytic syndromes
Familial hemophagocytic lymphohistiocytosis
Secondary hemophagocytic syndrome
Storage disorders
Gaucher's disease
Niemann-Pick disease
Tangier disease
Sinus histiocytosis with massive lymphadenopathy (SHML), also known as Rosai-Dorfman disease, is a rare, self-limited histiocytic disorder of unknown cause. It is typically characterized by massive bilateral enlargement of the cervical lymph nodes, often accompanied by fever and weight loss; extranodal presentations can occur, and lymph nodes in other sites may be involved (see Pearls and Pitfalls ).
SHML can occur at any age but is most common in the first and second decades of life (median age, 20 years); there is a slight male preponderance. The disease has been found worldwide, with a slightly higher prevalence in Africans. It is thought to be a non-familial disorder, although one report described the presence of the disease in three brothers. Moreover, histologic features of SHML have been reported in lymph nodes of patients with autoimmune lymphoproliferative syndrome (ALPS).
The cause and pathogenesis of SHML remain unclear. The indolent clinical course suggests a reactive rather than a neoplastic process. Studies of clonality indicate that it is polyclonal. It has been hypothesized that SHML is a reaction to an infectious agent, such as human herpesvirus 6, parvovirus B19, polyomavirus, or Epstein-Barr virus (EBV); however, no infectious agent has been definitively linked to SHML. An association with systemic lupus erythematosus has also been reported. Recent publications reported patients with SHML to have an increased number of immunoglobulin G4 (IgG4)–positive plasma cells and an increased IgG4/IgG ratio in affected tissues, suggesting that SHML may be a part of the spectrum of IgG4-related diseases. However, most studies concluded that whereas SHML patients may have increased IgG4-positive plasma cells, patients lack the criteria needed to belong in the spectrum of IgG4-related diseases.
Patients with SHML typically have painless, massive bilateral cervical lymphadenopathy, accompanied by low-grade fever, weight loss, leukocytosis, polyclonal gammopathy, and elevated erythrocyte sedimentation rate. A mild normochromic normocytic anemia may also be present. Extranodal involvement occurs in 25% to 40% of patients and may be the initial manifestation of SHML in some cases. Cases with pure extranodal presentation have been reported, mainly within the central nervous system, nasal cavity, and paranasal sinuses. In general, the most common extranodal sites are skin, upper respiratory tract, soft tissue, orbit, bone, salivary gland, central nervous system, breast, and pancreas.
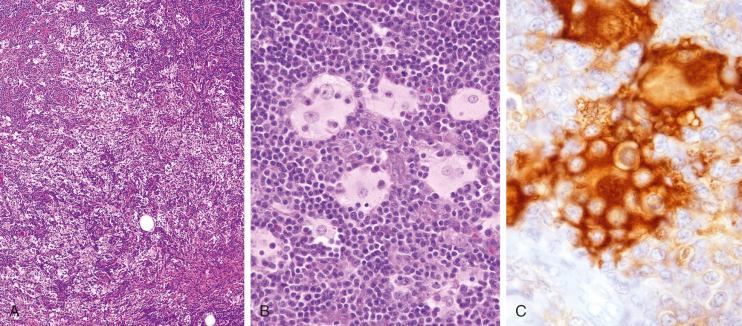
SHML is characterized by the expansion of lymph node sinuses by large histiocytes accompanied by lymphocytes and plasma cells, causing pronounced sinusoidal dilation ( Fig. 52-1 ). Total effacement of the normal lymph node architecture may occur as the disease progresses. The histiocytes have large, round or oval nuclei with dispersed chromatin, often prominent nucleoli, and abundant pale cytoplasm. Within the histiocytes, the presence of lymphocytes and plasma cells in intracytoplasmic vacuoles that protect them from degradation by cytolytic enzymes, a process called emperipolesis, is characteristic but not specific for SHML ( Fig. 52-1 ). Erythrophagocytosis may also be observed. Plasma cells are typically numerous in the medullary cords. Granulomas may be seen in rare cases. In extranodal sites, where there are no sinuses, the histiocytes form aggregates that resemble dilated sinuses ( Fig. 52-2 ). Emperipolesis may be less conspicuous in extranodal sites and prominent loose fibrosis may be seen, often with a somewhat edematous-appearing background ( Fig. 52-2 ). Although the diagnosis of SHML can be made on fine-needle aspirates, which show the characteristic histiocytes exhibiting emperipolesis identified in a background of lymphocytes and plasma cells, limited sampling may lead to difficulty in establishing diagnosis.
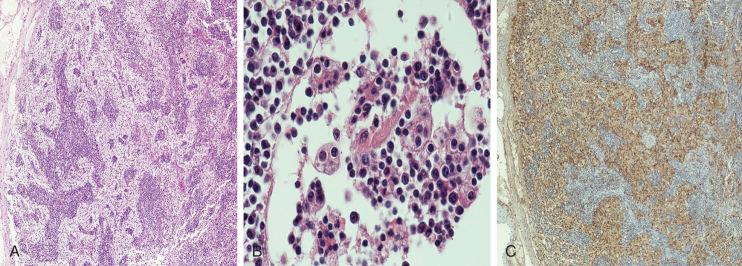
The histiocytes in SHML express S100 (see Fig. 52-1 ) and other macrophage-associated markers, such as CD4, CD11c, CD14, CD64, CD33, and CD68. A variable number of cells express the macrophage-associated enzymes lysozyme, α 1 -antitrypsin, and α 1 -antichymotrypsin. CD30 is reportedly positive in half the cases, although the histiocytes show cytoplasmic staining and not true membranous staining, likely representing nonspecific staining. In contrast to Langerhans cell histiocytosis, CD1a positivity is seen in less than 10% of cases of SHML; cathepsin D and E are positive in both disorders.
SHML typically has an indolent, protracted course with an excellent prognosis. The disease usually lasts between 3 and 9 months, followed by spontaneous remission. However, persistent disease lasting more than 5 years may infrequently be seen. On occasion, the disease is fatal, particularly in patients with immunologic abnormalities. Patients with an aggressive course and recurrences after complete remission tend to have multiple sites of lymph node involvement or involvement of multiple extranodal sites. Development of lymphoma in patients with SHML has been reported, as has focal SHML in lymph nodes involved by lymphoma, but an increased risk of lymphoma has not been documented. Complete surgical resection is the most effective treatment for recurring cases and for cases with an aggressive course. Several postoperative modalities, including chemotherapy, steroids, interferon, and radiotherapy, have been used but with variable results.
It is important to differentiate SHML from Langerhans cell histiocytosis. In contrast to the histiocytes of SHML, the characteristic cytologic features of Langerhans cells include elongated, grooved nuclei, inconspicuous nucleoli, and a smaller amount of pale cytoplasm. Eosinophils are typically numerous, plasma cells are absent, and emperipolesis does not occur in Langerhans cell histiocytosis. Other disorders in the differential diagnosis are reactive sinus histiocytosis and sinusoidal malignant tumors. Both of these lack the massive expansion of sinuses by histiocytes and lymphophagocytosis that occur in SHML. Although the prominent nucleoli of the histiocytes in SHML can give them an atypical appearance, the absence of mitotic activity is useful in ruling out malignancy. Hemophagocytic syndromes, especially the familial form that occurs in early life, can mimic SHML; however, these syndromes are characterized by disseminated disease and an aggressive clinical course. Infectious processes inducing the proliferation of histiocytes, such as tuberculosis, should also be considered in the differential diagnosis, but true granulomas and necrosis are uncommon in SHML.
Hemophagocytosis describes the pathologic finding of activated macrophages engulfing erythrocytes, leukocytes, platelets, and their precursor cells. The contemporary classification of histiocytic disorders divides the hemophagocytic syndromes into primary (familial) and secondary hemophagocytic lymphohistiocytosis (HLH). The familial form occurs in infants or young children with a clear genetic or familial inheritance. Although HLH in these patients can be associated with infections or vaccination, the immunologic trigger is often not apparent. Secondary HLH typically affects older children or adults who present without a family history or known genetic cause for their HLH. It occurs in response to specific infections or malignant tumors or in the context of rheumatologic disorders. HLH thus encompasses two similar syndromes, one with a genetic cause and one without such a cause. The symptomatic presentations are highly overlapping. The most recent modified diagnostic guidelines for diagnosis of HLH are listed in Box 52-2 .
The diagnosis of HLH is established in the presence of
Molecular diagnosis consistent with HLH ( PRF1 , NC13D , STXBP2 , RAB27A , STX11 , SH2D1A , or XIAP )
or
Presence of five of the eight following clinical criteria
Fever
Splenomegaly
Cytopenias affecting ≥2 of 3 lineages
Hemoglobin <90 g/L (in infants <4 weeks: <100 g/L)
Platelets <100 × 10 9 /L
Neutrophils <1.0 × 10 9 /L
Hypertriglyceridemia or hypofibrinogenemia
Fasting triglycerides ≥3.0 mmol/L (i.e., 265 mg/dL)
Fibrinogen ≤1.5 g/L
Hemophagocytosis in bone marrow or spleen or lymph nodes
Low or absent natural killer cell activity (according to local laboratory reference)
Elevated ferritin ≥500 µg/L
Elevated soluble CD25 (i.e., soluble interleukin-2 receptor) ≥2400 U/mL
Familial HLH should have no evidence of malignancy.
Additional supportive evidence for HLH includes
Central nervous system symptoms and spinal fluid pleocytosis (mononuclear cells) or elevated spinal fluid protein
Jaundice, hepatic enzyme abnormalities, and histologic picture resembling chronic persistent hepatitis; coagulopathy, lymph node enlargement, edema, rash, hypoproteinemia, and hyponatremia
Absence of hemophagocytosis does not exclude HLH.
Familial hemophagocytic lymphohistiocytosis (FHLH) is a rare systemic syndrome with autosomal recessive inheritance that results from histiocyte activation manifested by the widespread proliferation of benign macrophages throughout the reticuloendothelial system and extranodal sites. This is associated with florid hemophagocytosis, various systemic symptoms, and peripheral blood cytopenias. The disorder encompasses familial erythrophagocytic lymphohistiocytosis, which was described by MacMahon and colleagues in 1963.
FHLH has an incidence of approximately 1 to 2 per 1 million children, although in Sweden, the estimated incidence is 1/50,000 live births. The symptoms usually become evident within the first 6 months of life and may, in rare cases, even develop in utero or at birth. However, familial forms with a later onset, at any time up to adulthood, have also been reported. The disease occurs in a known familial setting in about 50% of the cases and as a sporadic event in about 50%.
A variety of genetic syndromes are associated with HLH, all of which lead to immunologic dysregulation and persistent hypercytokinemia, which triggers T-cell and macrophage activation and a predisposition to development of HLH. Genetic forms of HLH can occur as primary FHLH or in association with several distinct immune deficiency syndromes.
In FHLH, a number of candidate genes have been identified by linkage analysis ( Table 52-1 ); however, in 20% to 50% of the cases, the involved genes are yet to be identified. They all lead to the common phenotype of impaired cytotoxic function by natural killer (NK) cells and T cells. PRF1 was the first gene reported as a cause of FHL2, accounting for about 30% to 35% of cases. It causes a deficiency of the cytolytic effector perforin, resulting in absent or barely detectable perforin protein in cytotoxic granules. In addition, several unusual missense mutations of the perforin gene have been identified, resulting in a mutated protein that is not cytotoxic to the target cell, which may be associated with atypical (late-onset) FHLH. Perforin polymorphism C272T (Ala91Val) is also frequently found in late-onset FHLH. Homozygosity for this allele appears to be associated with susceptibility to lymphoma and leukemia. MUNC13-4 deficiency (FHL3), caused by mutations in UNC13D , accounts for about 30% of FHLH cases. MUNC13-4 is essential for cytolytic granule fusion with other structures related to the cytoplasmic membrane, and the mutations result in defective degranulation. The third gene found to be mutated in FHL4 was STX11 , which encodes syntaxin 11. Patients with mutations in STX11 have a worldwide distribution, although the vast majority is of Turkish/Arab descent (accounting for 20% of cases), and show a late-onset disease. The most recently identified cause of FHL5 is a deficiency of the STXBP2 gene, which encodes syntaxin-binding protein 2, also termed MUNC18-2. STXBP2/MUNC18-2 proteins play a complementary role in membrane fusion.
| Disease | Gene | Location | Protein | Defect |
|---|---|---|---|---|
| FHL1 | Unknown | 9q21_3-22 | Unknown | Unknown |
| FHL2 | PRF1 | 10q21-22 | Perforin | Vesicle content |
| FHL3 | UNC13D | 17q25 | MUNC13_4 | Vesicle priming |
| FHL4 | STX11 | 6q24 | Syntaxin11 | Vesicle docking and fusion |
| FHL5 | STXBP2 | 19p13_2-3 | MUNC18_2 | Vesicle docking and fusion |
| Chédiak-Higashi | LYST | 1q42_1-42_2 | LYST | Vesicle trafficking |
| Griscelli type 2 | RAB27A | 15q21 | RAB27A | Vesicle fusion |
| Hermansky-Pudlak type 2 | AP3B1 | Vesicle trafficking | ||
| XLP type 1 | SH2D1A | Xq24-26 | SAP | Multiple, including CD8 + T/NK-cell cytotoxicity |
| XLP type 2 | XIAP | Xq25 | XIAP | Multiple signaling pathways |
Three distinct immunodeficiencies with pseudoalbinism have been associated with HLH: Chédiak-Higashi syndrome (mutations in lysosomal transport LYST ), Griscelli syndrome type 2 (mutations of RAS-associated protein 27A [RAB27A]), and Hermansky-Pudlak syndrome type 2 (mutations of adaptor protein 3 B1 subunit [AP3B1]). These are lysosomal trafficking disorders that share with FHLH the common pathophysiologic mechanism of impaired cytotoxicity responses that lead to the inability of effector lymphocytes to kill infected cells. Some of the proteins required for lytic granule secretion by effector lymphocytes are also required for melanocyte trafficking of pigment granules, which explains the association of albinism and impaired immune function in these syndromes.
X-linked lymphoproliferative disorder (XLP) is another inherited deficiency that is frequently associated with HLH. It is characterized principally by extreme vulnerability to EBV infection, which triggers HLH, malignant lymphoproliferation, or both. XLP type 1 is caused by mutations in the SH2D1A gene, whereas mutations in the gene encoding the X-linked inhibitor of apoptosis ( XIAP , also known as BIRC4 ) are responsible for XLP type 2.
The clinical presentation is usually characterized by fever, failure to thrive, rash, anemia, thrombocytopenia, disseminated intravascular coagulation, and hepatosplenomegaly. However, the presentation may vary widely with a variety of associated conditions, including non-remitting fever of unknown origin, hepatitis/acute liver failure, sepsislike features, hyponatremia, Kawasaki-like symptoms, and neurologic abnormalities. Neonates with HLH may have hydrops fetalis and liver failure. Hypertriglyceridemia, hypofibrinogenemia, and hyperferritinemia are typically found. Immunologic criteria for a provisional diagnosis include elevated levels of ferritin and soluble IL2Ra (sCD25), both markers of generalized inflammation. Very high levels of sIL2Ra are almost never seen outside HLH, and ferritin levels at the range of 10,000 g/mL are highly indicative of HLH. Upregulation of CD163 (a receptor for hemoglobin-haptoglobin complexes) on monocyte-macrophages facilitates hemophagocytosis. The plasma levels of soluble CD163 in HLH are considerably higher than those found in infections, autoimmune diseases, and cancer. NK-cell function is low or absent in many patients with HLH at initial presentation, although the number of circulating NK cells (CD56 + /16 + ) is generally normal.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here