Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
This chapter describes key clinical and histologic features of relatively common or well-known non-neoplastic disorders of pigmentation.
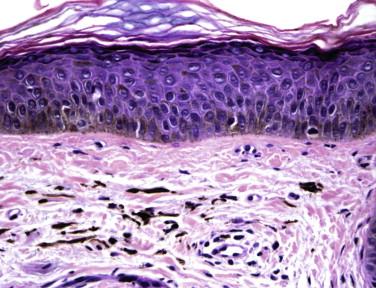
Café-au-lait macules are very common. Solitary lesions are seen in approximately 10% to 20% of the adult population. They are more common in the black population than in whites. Clinically, they appear as homogeneous light to dark brown completely macular lesions with well-defined borders that range in size from freckle-sized lesions to 20 cm or more in diameter ( Fig. 7-1 ). Café-au-lait macules may be present at birth and may increase in both size and number as a child ages. They can be normal variants or part of a systemic disease, such as neurofibromatosis or Albright's syndrome. Multiple lesions, especially if they are larger in size, are unusual and should prompt consideration of an underlying systemic disorder.

There is an increase in melanin pigment deposition within basilar keratinocytes. The density of melanocytes is normal or only slightly increased. The increased pigmentation typically spares the adnexal epithelium.
Café-au-lait macules have a distinctive appearance and are usually easily recognizable on clinical examination, although they may be confused with postinflammatory hyperpigmentation, melasma, or melanocytic nevi. Café-au-lait macules have a tendency to grow in proportion to growth of the rest of the body. They do not change with sun protection or bleaching agents. Their completely macular appearance may be helpful for the correct diagnosis. Histologically café-au-lait macules are usually indistinguishable from freckles, melasma, and the melanotic macules of Albright's syndrome. They can be differentiated from melanocytic nevi and simple lentigines by their lack of melanocyte proliferation and rete ridge elongation. Café-au-lait macules differ from lesions of postinflammatory hyperpigmentation by the presence of an inflammatory infiltrate or pigment incontinence in the latter.
Café-au-lait macules are benign lesions. Bleaching agents and sun protection do not affect the appearance of these lesions. Laser surgery has been used to treat the cosmetic appearance of these lesions with variable success.
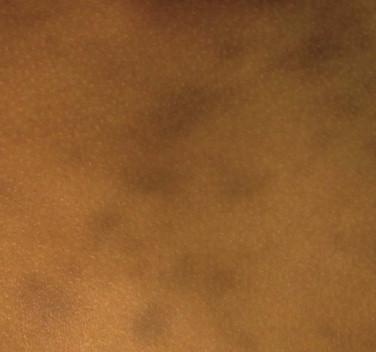
Melasma is a common acquired symmetrical hyperpigmentation of sun-exposed areas on the face and neck found predominantly in women. Melasma has a complex etiology, with genetic predisposition, ultraviolet light exposure, and hormonal influences all potentially playing roles. Melasma typically presents as individual brown, gray, or blue macules that coalesce into irregular patches without erythema or other evidence of inflammation. Three different patterns of pigmentation are commonly found: centrofacial (most common), malar, and mandibular. Wood's light examination may be helpful in determining the depth within the skin of melanin deposition. Increased melanin may be found either within the epidermis or dermis. In lesions with increased epidermal melanin, the contrast between unaffected skin and lesions enhances with Wood's light examination. These lesions are amenable to bleaching agents. Lesions with increased dermal melanin do not demonstrate increased contrast and do not respond to bleaching agents. A mixed type may show some enhancement in some areas of the lesion. In individuals with darkly pigmented skin, a Wood's light examination may be difficult to perform accurately, and a biopsy may be needed to determine the level of melanin deposition within the skin.
Two patterns may be seen upon microscopic examination in melasma. In the first, pigment predominates within the epidermis; in the second, it is primarily localized to the superficial dermis ( Fig. 7-2 ). Melanin is deposited in keratinocytes throughout the epidermis in the first type. Vacuolar degeneration of basal cells may also be seen. In the second type, melanin-laden macrophages collect around vessels throughout the dermis. Both an increased number of melanocytes and an increased amount of melanin may be seen. In some patients with melasma, melanin deposition occurs within both the epidermis and dermis.
Melasma must be distinguished from postinflammatory hyperpigmentation, drug-induced hyperpigmentation, and exogenous ochronosis. Clinically, a careful history for medications associated with hyperpigmentation, either systemic or topical; the absence of other primary lesions; and a history of worsening with sun exposure or during increased hormonal states such as pregnancy or while the patient is taking oral contraceptive pills help to distinguish melasma from other diseases.
Melasma may be histopathologically indistinguishable from postinflammatory hyperpigmentation. Microscopic examination may allow differentiation from certain drug-induced hyperpigmentation states that have distinctive features, such as the yellow-brown pigment seen in ochronosis.
This disorder is difficult to treat. Patients must minimize sun exposure and use a broad-spectrum sunscreen consistently. If the pigment is determined to be superficial by Wood's light examination or biopsy, the patient may benefit from bleaching agents such as hydroquinone. Other modes of therapy, including lasers, have also been attempted.
This disease was first described in El Salvador in 1957. It is most commonly described in Latino patients, but cases have also been described in Asians and non-Hispanic whites. The age of onset is variable, and there is no gender predilection. A variety of inciting triggers in genetically predisposed individuals has been suggested as the mechanism for this disorder, but no clear etiology has been established.
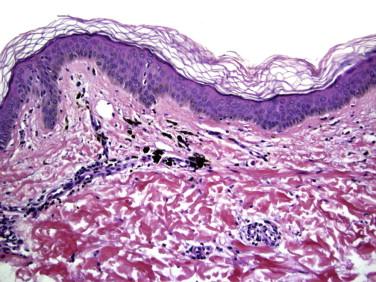
The condition manifests as gray, gray-blue, or brown macules and patches of variable size and shape ( Fig. 7-3 ), sometimes seen with a narrow erythematous peripheral border. The lesions are symmetrically distributed, most commonly on the neck, trunk, and proximal arms. The long axis of lesions sometimes follows skin cleavage lines. Lesions are usually slowly progressive and may persist for years.
The borders of active lesions show vacuolization of the basal layer; occasional colloid bodies; and a lichenoid or perivascular infiltrate of lymphocytes, histiocytes, and melanophages ( Fig. 7-4 ). Exocytosis of the infiltrate may also be seen in some lesions. In inactive lesions, a thinned epidermis, prominent pigment incontinence, and melanophages in the upper dermis may be observed.
Erythema dyschromicum perstans must be distinguished from postinflammatory hyperpigmentation and fixed drug eruption. Diseases that approximate the clinical distribution of erythema dyschromicum perstans, such as pityriasis rosea, may result in postinflammatory hyperpigmentation. Microscopically, however, these lesions lack the vacuolar change seen in erythema dyschromicum perstans. A careful drug history may be helpful in distinguishing erythema dyschromicum perstans from multiple lesions of a fixed drug eruption.
Erythema dyschromicum perstans may on occasion be confused clinically with a macular lichenoid keratosis or a melanocytic lesion such as an inflamed junctional nevus or melanoma in situ.
There are few effective treatments for this condition. In small series of patients, there have been responses to clofazimine or dapsone. There are occasional spontaneous remissions.
Many drugs are associated with hyperpigmentation of the skin. Medications commonly associated with pigmentary change include antineoplastic medications, antimalarial drugs, heavy metals, and hormones. Specific medications that are well known to cause hyperpigmentation include amiodarone, azidothymidine, clofazimine, and minocycline. The clinical and histologic appearance of lesions from drug-induced hyperpigmentation is markedly variable, depending on the inciting agent, and an exhaustive description is beyond the scope of this chapter. Three of the more distinctive drug-induced hyperpigmentations are described in detail here.
Minocycline is commonly used for acne and other inflammatory conditions. Long-term use of this tetracycline derivative can result in cutaneous hyperpigmentation.
Three types of cutaneous hyperpigmentation may be seen. Type I is a dark blue to black hyperpigmentation that occurs in areas of inflammation or previous scarring. Type II hyperpigmentation is a blue to gray discoloration of previously normal skin ( Fig. 7-5 ) that is most commonly encountered on the anterior legs but that may also involve the arms. The third type (type III) is a diffuse muddy brown hyperpigmentation that is most prominent in sun-exposed areas.

Each of the clinical types of minocycline hyperpigmentation has distinctive histopathologic features ( Fig. 7-6 ). Type I is characterized by aggregates of pigment-laden macrophages within the dermis. This pigment contains iron, as demonstrated by histochemical stains such as Prussian blue, but is negative for melanin as assessed by the Fontana reaction. Type II lesions also demonstrate macrophages containing pigment. This pigment is positive with iron stains and Fontana-Masson. The lesions in type III contain increased amounts of melanin within basal keratinocytes and within dermal macrophages. Iron is absent.
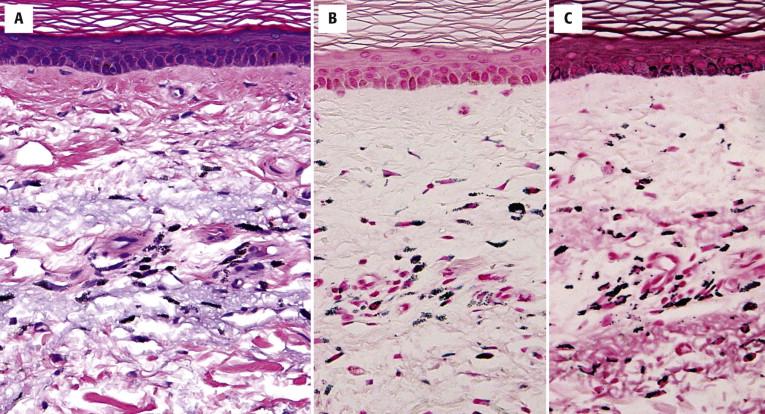
A combination of histochemical stains helps classify the pigment based on its reaction with the Prussian blue and Fontana stain (see the preceding discussion). Minocycline deposits can be observed directly with fluorescent microscopy as yellowish fluorescence after frozen tissue samples are allowed to sit overnight in 1 M of Mg-Cl 2 -ethanol.
Clinically, type I hyperpigmentation can be confused with other drug-induced hyperpigmentation such as that caused by amiodarone, exogenous ochronosis, and heavy metal exposure. Type II has fairly distinctive features both clinically and microscopically. Type III must be distinguished from melasma and postinflammatory hyperpigmentation. In all cases, a careful clinical history is the most straightforward means of determining the correct diagnosis.
After minocycline is discontinued, the hyperpigmentation will typically resolve over months to years. Laser therapy has been used with some success in recalcitrant cases.
Long-term continuous use of this antiarrhythmic agent can cause discoloration of the skin. After discontinuation of the drug, the hyperpigmentation typically resolves slowly over time. This condition is more common in fairer individuals than in individuals with darker skin pigmentation. A photodistributed erythema sometimes is seen in conjunction with the appearance of hyperpigmentation.
The discoloration typically has a bluish-gray hue. It affects sun-exposed areas, most typically the face.
Yellow-brown lipofuscin pigment granules are present within dermal macrophages and endothelial cells.
The granules are typically positive by periodic acid-Schiff (PAS) staining and in some cases stain with the Ziehl-Neelsen, Fontana, and Sudan black methods.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here