Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
This lesion may occur as a smooth-surfaced nodule or have a bossellated, multinodular, or papillary appearance and is discussed in Chapter 5 .
This occurs in adults wearing maxillary dentures (usually in the sixth decade upwards) and is occasionally seen in patients with high-arched palates and mouth-breathing habit. Patients may report sensitivity, especially if associated with candidiasis because the denture often functions as a fomite ( Fig. 3.1 ).

Pebbly excrescences occur on the palatal vault in a diffuse, symmetric distribution.
Papillary hyperplasia of the palatal mucosa results from chronic irritation due to dentures or from mouth-breathing that leads to reactive hyperplasia of tissues.
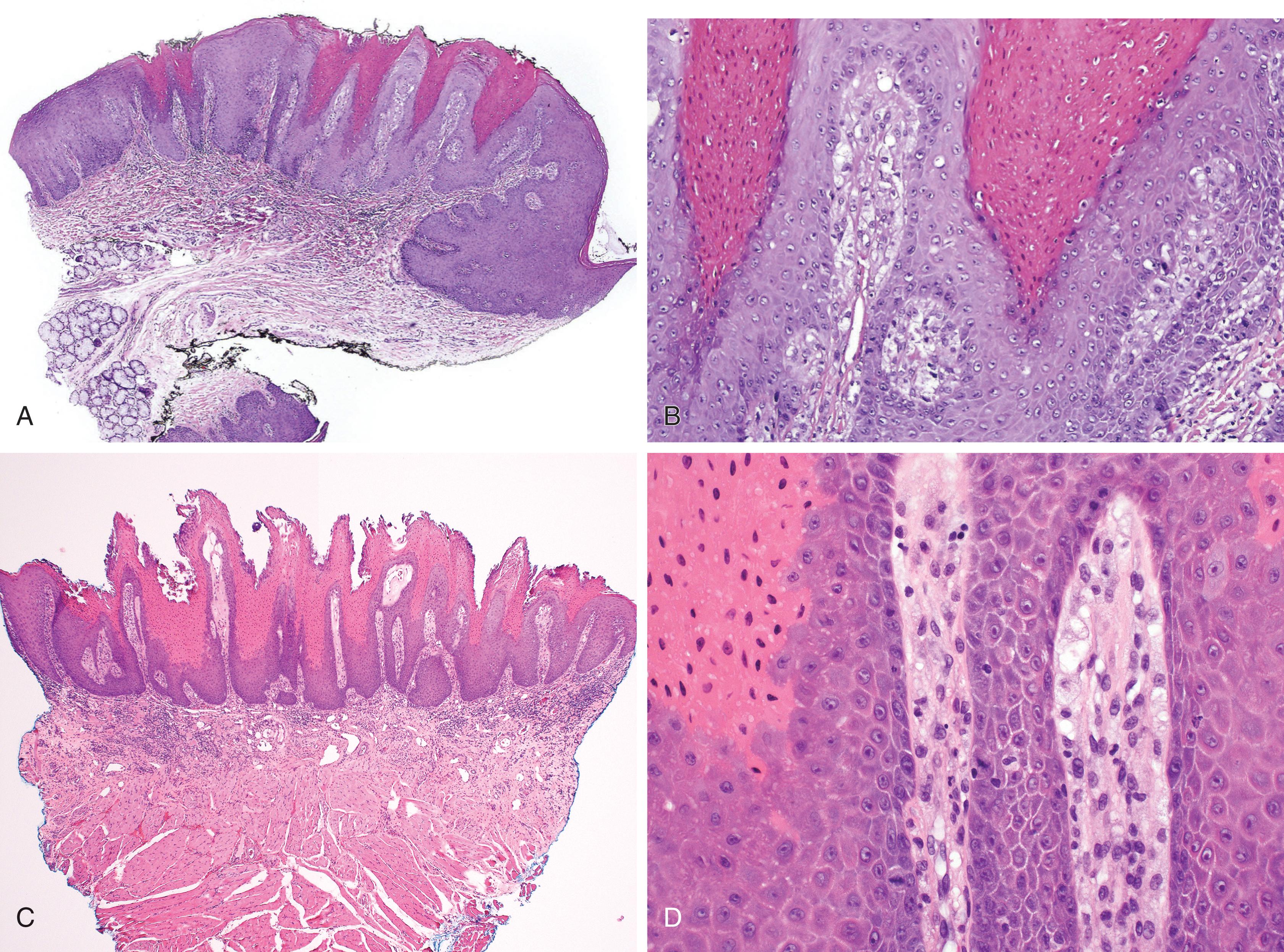
Proliferation of fibrovascular tissue occurs in nodules with a variable lymphoplasmacytic infiltrate. The overlying epithelium may be hyperplastic and exhibit spongiosis and leukocyte transmigration. Pseudoepitheliomatous hyperplasia may be seen ( Figs. 3.2–3.4 ).
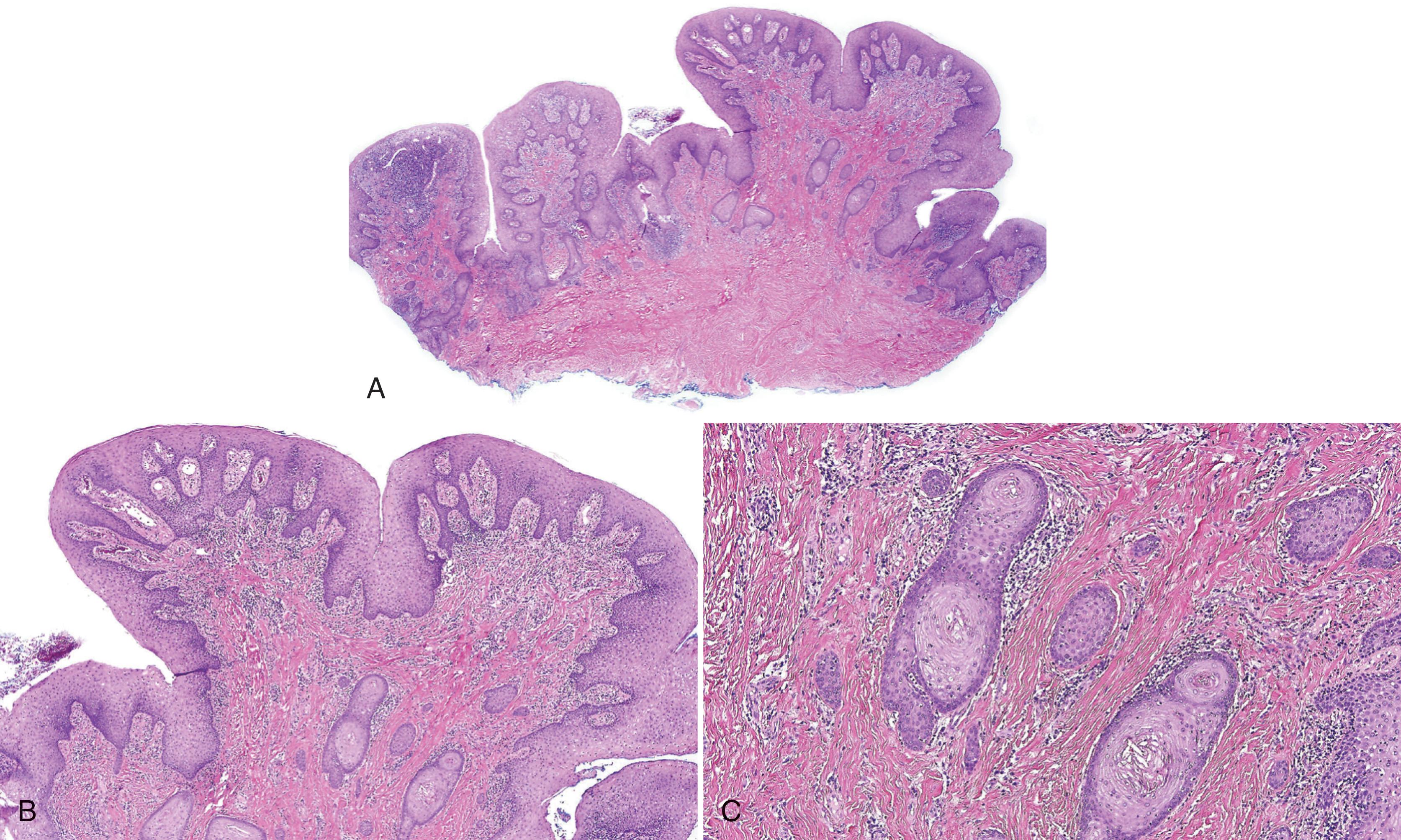
The presence of spongiotic pustules should always raise suspicion for candidiasis and periodic acid–Schiff staining with diastase should be performed.
Inflamed squamous papilloma is usually solitary and pedunculated.
Condyloma acuminatum is a solitary, discrete papillary epithelial hyperplasia with large, broad, and bulbous rete ridges and koilocytes (see Chapter 4 ).
Inflammatory papillary fibroepithelial hyperplasia may also occur at the edges of dentures and represents a similar reactive process.
Papillary hyperplasia of the palatal mucosa may occur overlying a salivary gland malignancy such as a polymorphous carcinoma which presents usually as a unilateral palatal swelling with overlying pebbly mucosa.
Excision or laser ablation of lesions must be accompanied by a denture reline or fabrication of new dentures. Lesions may recur if the denture continues to fit poorly.
For lesions caused by mouth-breathing or high-arched palatal vaults, patients should be reassured regarding the benign nature of the condition.
Secondary candidiasis can be effectively treated with topical antifungals (e.g., antifungal and steroid cream applied to the denture base [see Appendix B ]). The dentures should also be disinfected with chlorhexidine, nystatin, sodium benzoate, or other agent.
Canger EM, Celenk P, Kayipmaz S. Denture-related hyperplasia: a clinical study of a Turkish population group. Braz Dent J . 2009;20:243-248.
Gual-Vaques P, Jane-Salas E, Egido-Moreno S, Ayuso-Montero R, Mari-Roig A, Lopez-Lopez J. Inflammatory papillary hyperplasia: a systematic review. Med Oral Patol Oral Cir Bucal . 2017;22:e36-e42.
Mainville GN. Non-HPV papillary lesions of the oral mucosa: clinical and histopathologic features of reactive and neoplastic conditions. Head Neck Pathol . 2019;13:71-79.
Poulopoulos A, Belazi M, Epivatianos A, et al. The role of Candida in inflammatory papillary hyperplasia of the palate. J Oral Rehabil . 2007;34:685-692.
Vaz Goulart MC, Lara VS. Inflammatory papillary hyperplasia of the palate: quantitative analysis of Candida albicans and its negative correlation with microscopic and demographic aspects. Int J Prosthodont . 2011;24:235-237.
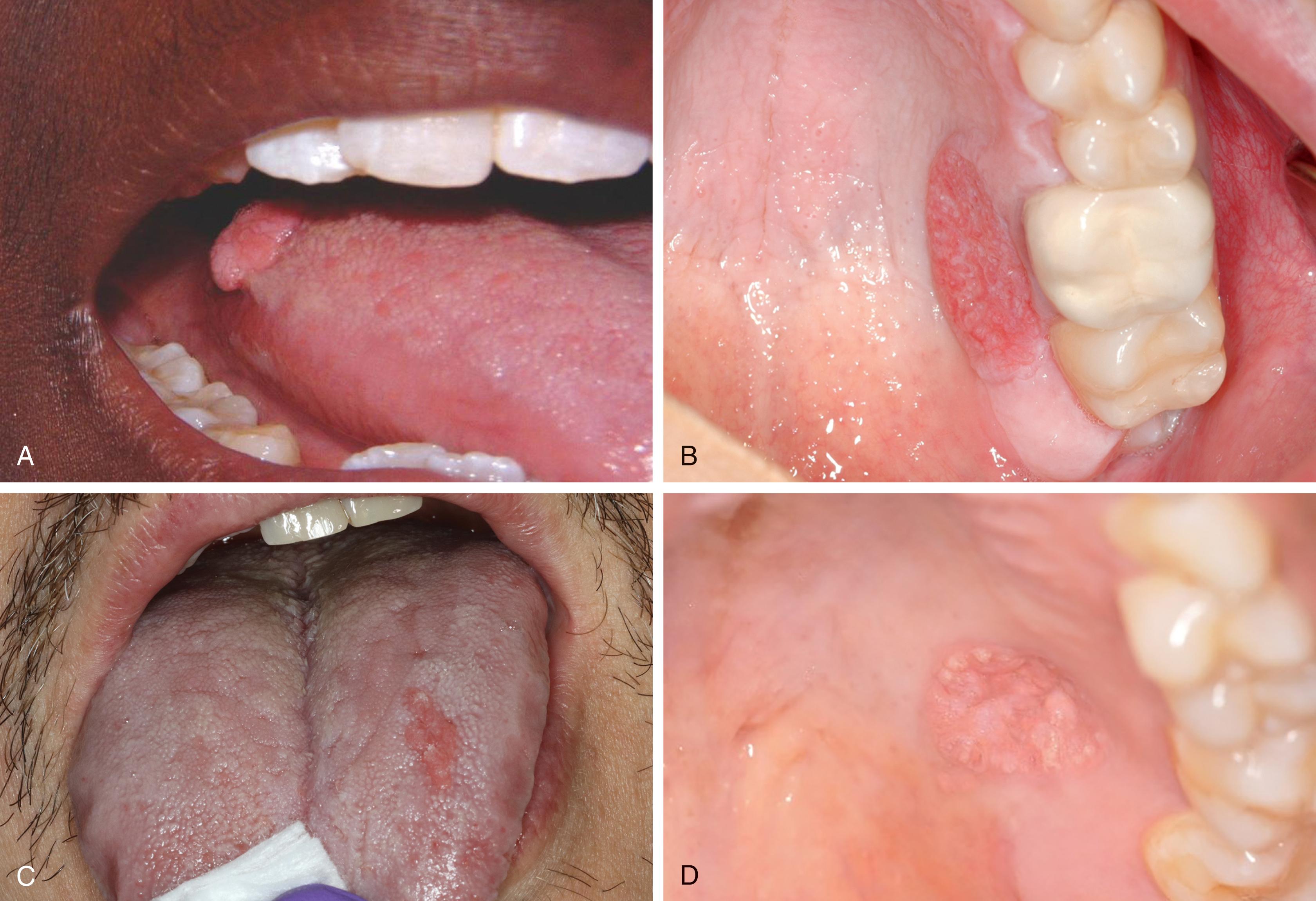
This occurs most frequently in the sixth to eighth decades of life with equal sex predilection. Seventy-five percent are located on the keratinized tissues of the gingiva and hard palatal mucosa, with the tongue and buccal mucosa being the next most common sites. It occurs as a painless, discrete, nontender, yellowish-red, or mucosa-colored plaque with a pebbly, warty appearance, although some have a smooth surface ( Fig. 3.5 ). It also occurs on the skin and genital mucosa.
This may be seen in areas of mucosa (or skin) exhibiting damage to the epithelium, such as from trauma, and inflammatory conditions such as lichen planus, pemphigus vulgaris, epidermolysis bullosa, and chronic graft-versus-host disease. It is less commonly associated with with dysplasia, carcinoma-in-situ, invasive carcinoma, chronic lymphedema, and congenital epidermal nevi.
Verruciform xanthoma is a reactive lesion believed to be mediated through neutrophils that cause degeneration of keratinocytes, a histiocytic response to products of epithelial breakdown, although some believe that it is accumulation of lipid-laden macrophages that induces the epithelial proliferation. Resident and reparative macrophages are involved. A subset of cutaneous cases shows mutation of the 3β-hydroxysteroid dehydrogenase gene, which is important in cholesterol biosynthesis. These lesions are not associated with human papillomavirus infection.
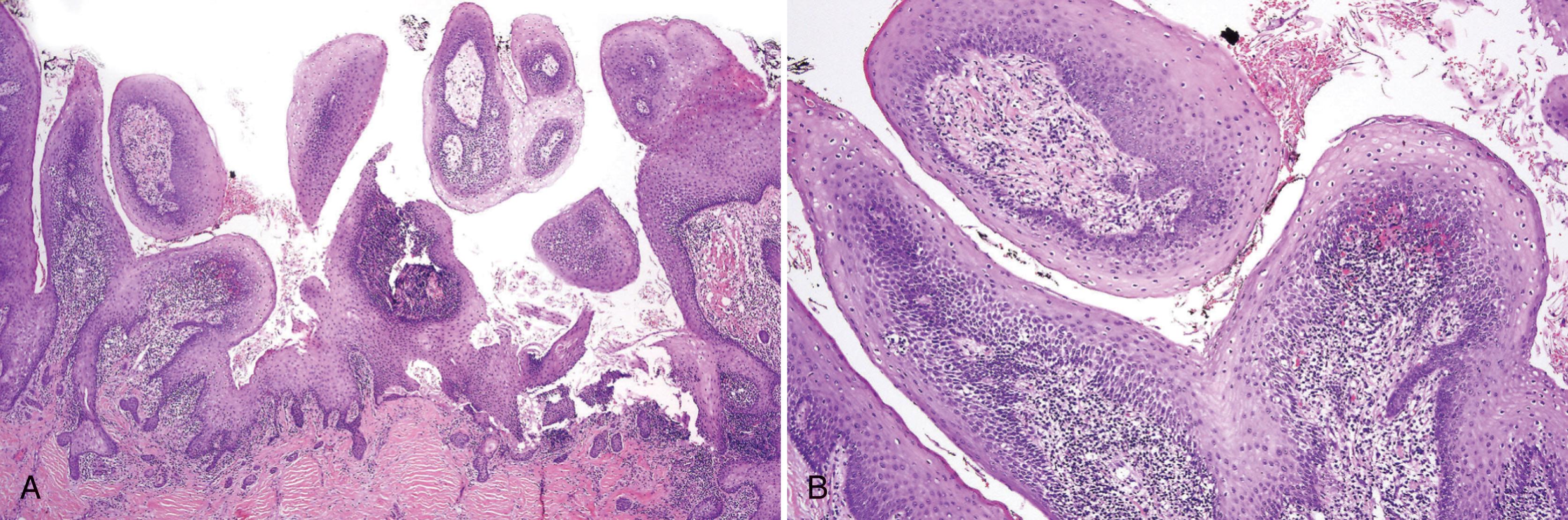
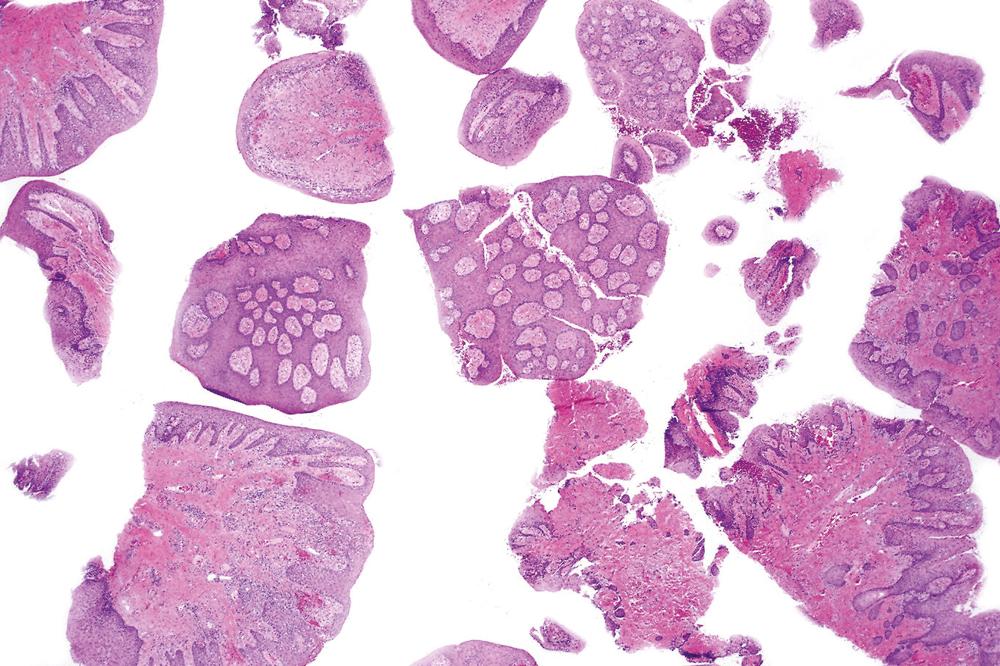
There is a benign papillary proliferation of stratified squamous epithelium with elongated rete ridges, generally of the same length and joined at the tips. There is parakeratosis with a brightly eosinophilic hue, parakeratin plugs, and keratin squames on the surface and within crypts. Neutrophilic transmigration and spongiosis are often present unassociated with candida ( Figs. 3.6 and 3.7 ). Infrequently, lesions have a flat surface ( Fig. 3.8 ).
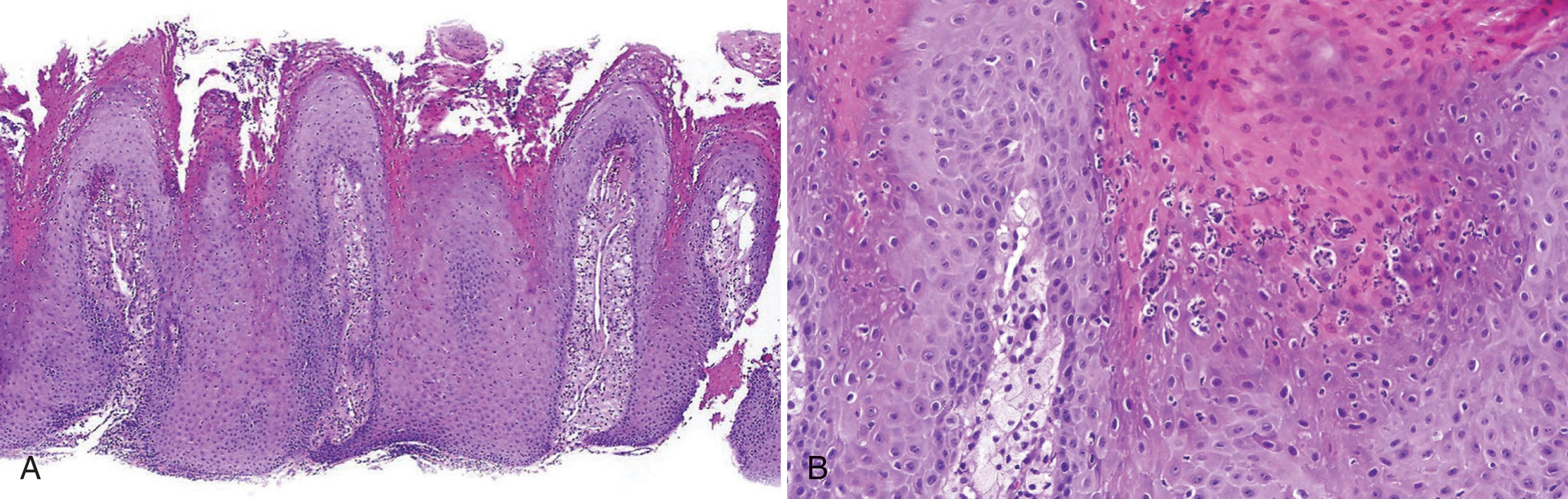
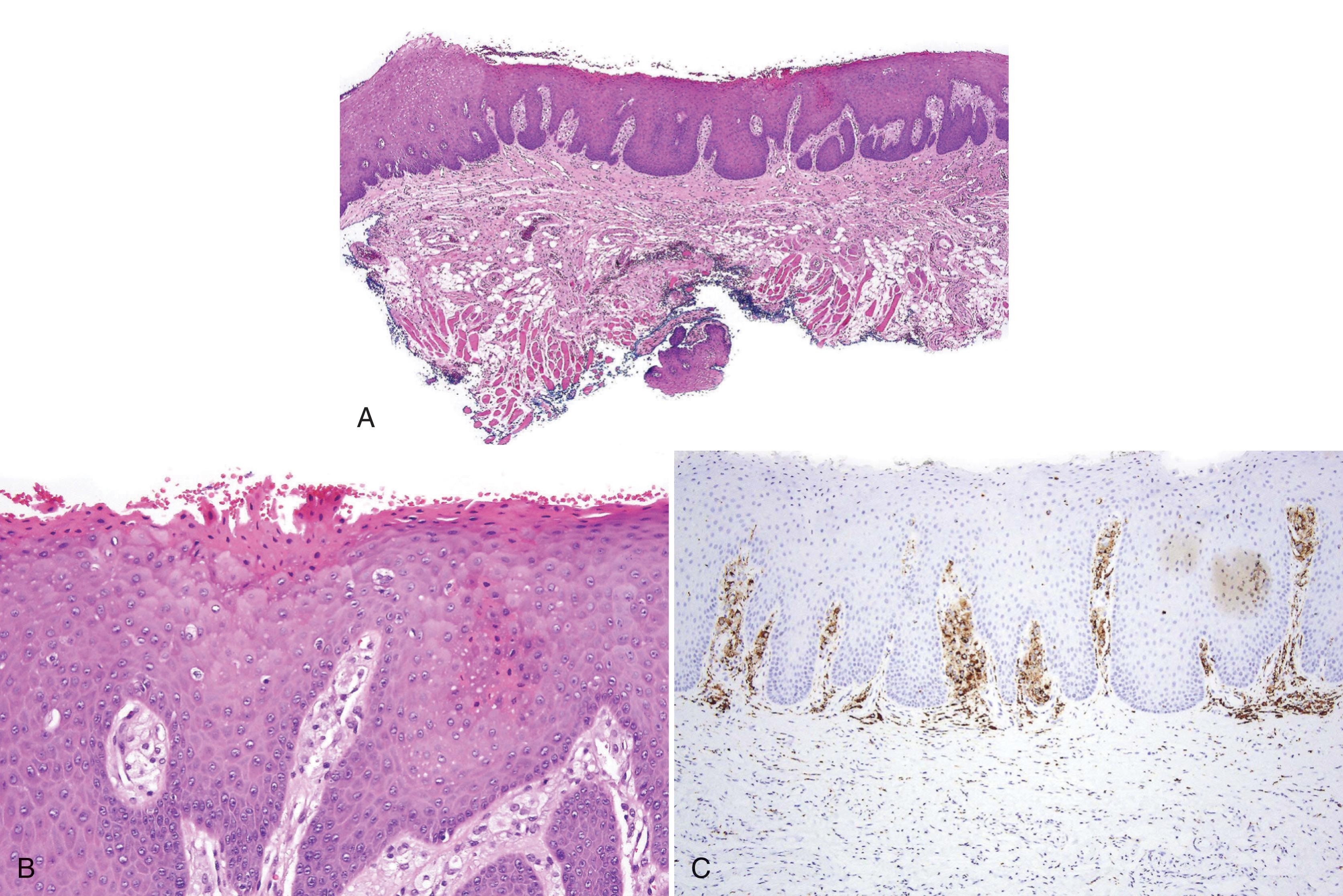
Foamy macrophages (positive for CD68 and CD163) fill the lamina propria (see Figs. 3.6–3.9 ).

When inflamed, there may be minimal parakeratosis ( Fig. 3.10 ).

Because of the association of verruciform xanthoma with other more serious conditions, evaluation for dysplasia, carcinoma in situ or invasive carcinoma should be performed at the edges of the specimen.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here