Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Most lower extremity ischemic symptoms occur in patients with atherosclerotic occlusive disease. Nonatheromatous causes must be considered, however, in the absence of significant atherosclerotic risk factors, especially in younger individuals. The two most common nonatheromatous causes of popliteal artery disease are popliteal artery entrapment syndrome (PAES) and adventitial cystic disease (ACD). These patients can be asymptomatic but clinical symptoms associated with these pathologies range from claudication to chronic limb-threatening ischemia (CLTI). Given their rarity and the younger age of presentation, these conditions are often not diagnosed in a timely fashion, resulting in prolonged disability and occasional progression to CLTI.
PAES was first described in 1879 by University of Edinburgh medical student Anderson Stuart. It was not until 1965, however, that Love and Whelan at the Walter Reed Army Medical Center in Washington, D.C., coined the term “popliteal artery entrapment syndrome” to describe this clinical entity. , The anatomic abnormalities associated with PAES have been observed in 3.5% of individuals in a post-mortem study, and up to 60% of young individuals with claudication symptoms suffer from this syndrome. Those affected tend to be active and otherwise healthy, which has led some clinicians to describe PAES as the “jogging disease.”
The majority (up to 80%) of reported cases are in men, with a median age of 32 years (range, 20.7–41 years). Cases of PAES have also been described in children, teenagers, women, and siblings, but are unusual. While the anatomic variant in affected individuals is developed in utero , several decades are sometimes necessary before symptoms develop. Bilateral lower-extremity symptoms in PAES have been described in approximately 30% of cases, and two-thirds of patients with unilateral symptoms were found to have bilateral anatomic abnormalities. Rare instances of bilateral popliteal artery occlusion secondary to popliteal artery entrapment have also been reported, and concurrent entrapment of the popliteal and anterior tibial arteries has been described. ,
The anatomical variations observed in PAES are best understood by considering the embryologic development of the structures within the popliteal fossa.
The lower extremity arterial system arises from two arteries, the axial and external iliac arteries, which originate from the umbilical artery. The femoral artery originates from the external iliac artery and progresses distally in the anterior compartment, whereas the axial artery elongates distally in the posterior compartment. At approximately 42 days of intrauterine life, the axial artery is divided into three segments, depending on its relationship to the popliteus muscle: proximal, deep, and distal. A bridging artery, the ramus communicans superius, joins the femoral artery and the proximal segment of the axial artery through the adductor hiatus. During the following week of development, the proximal component of the axial artery gives rise to a branch that runs superficial to the popliteus muscle and joins with the distal segment of the axial artery. The deep segment of the axial artery involutes, and the fully developed popliteal artery results from the fusion of these arterial elements ( Fig. 144.1 ).
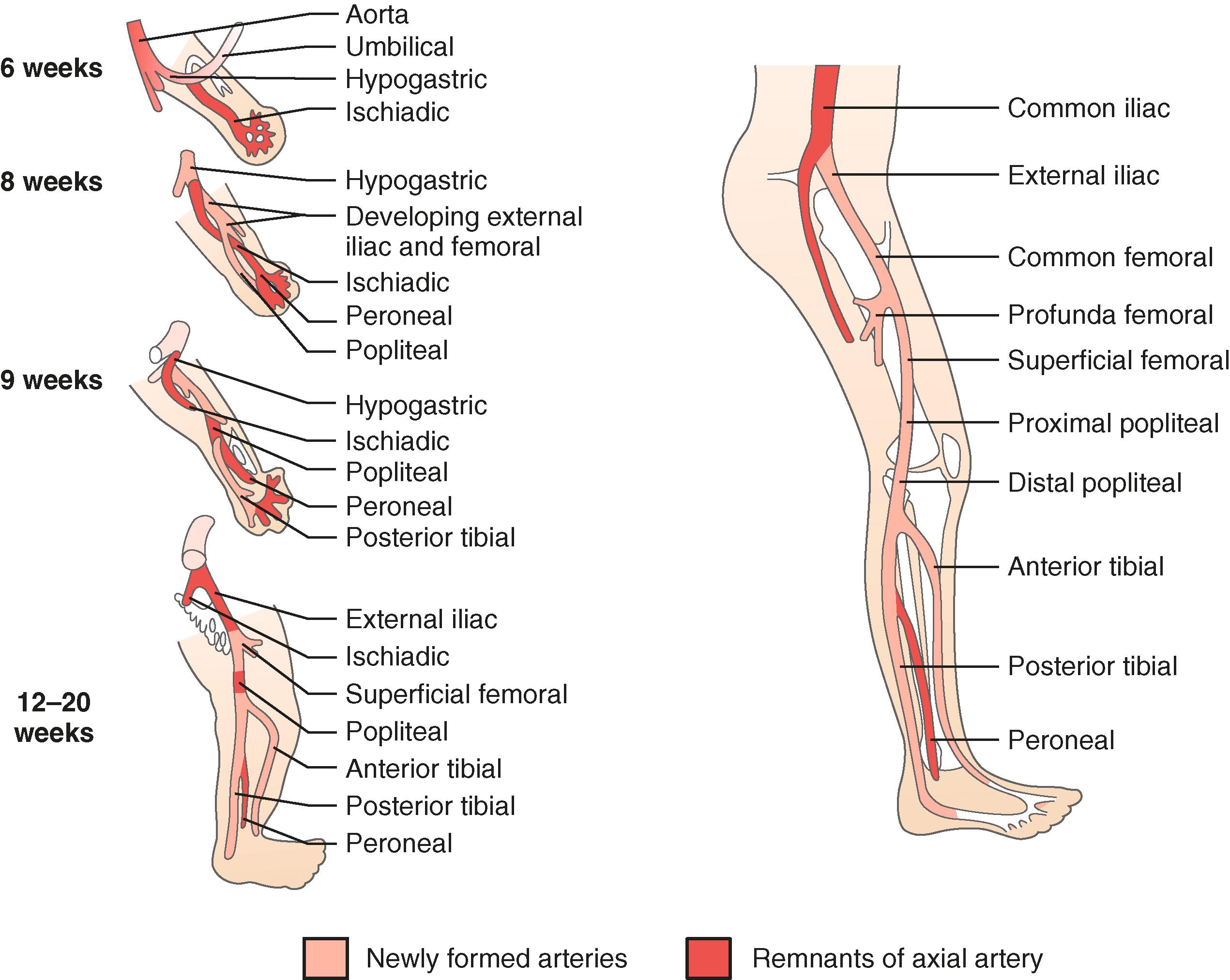
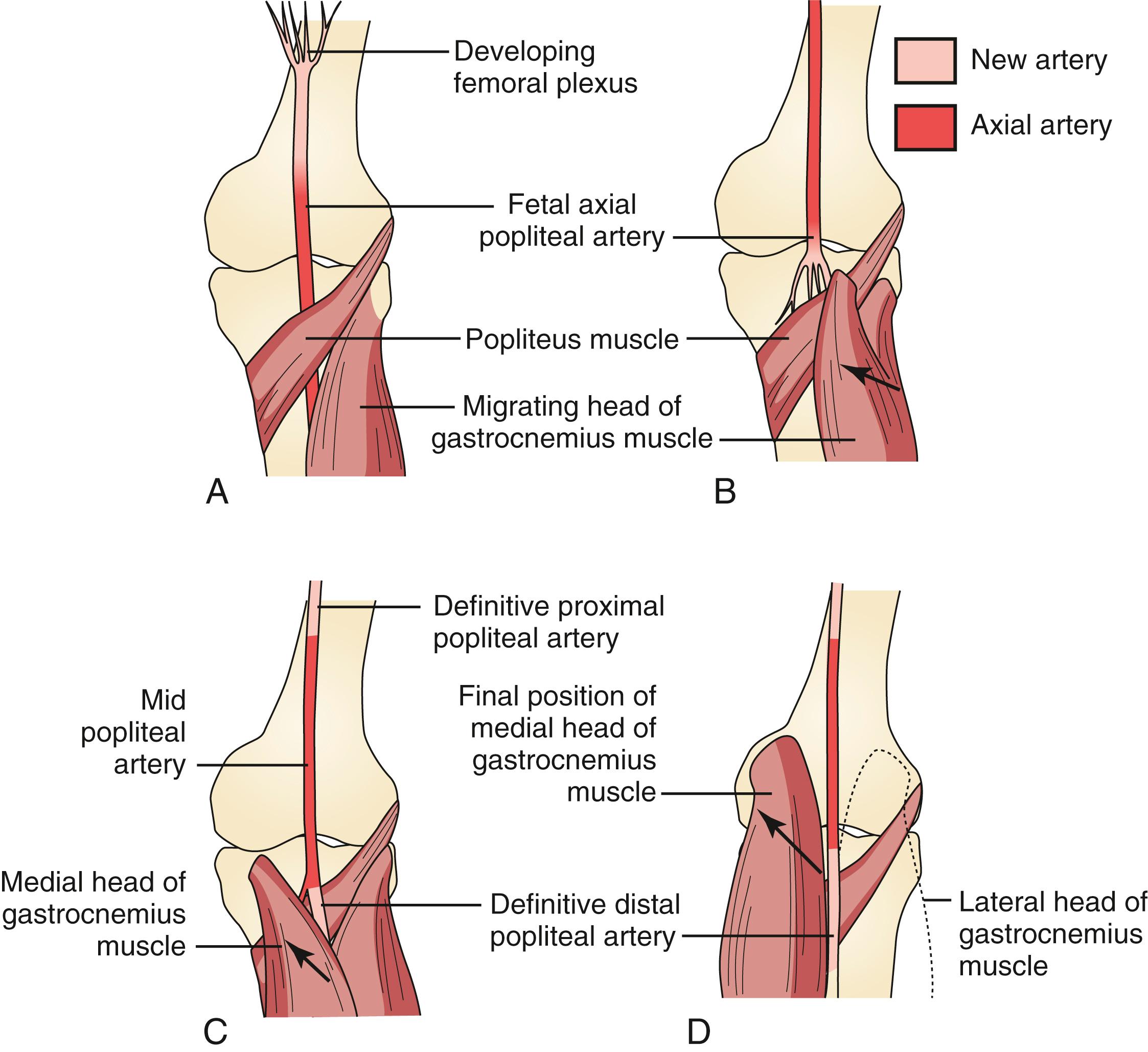
Initially, both heads of the gastrocnemius muscle originate from the proximal tibia. With development, they migrate cranially along the femur to different extents. The final position of the medial head of the gastrocnemius muscle is more proximal to that of the lateral head and immediately caudal to the adductor hiatus, with the popliteal artery lying immediately lateral. These dynamic processes of muscle and arterial development create the potential for various anatomic variations that can lead to popliteal artery entrapment ( Fig. 144.2 ).
The current PAES classification system consists of six variants and is based on the Heidelberg classification. It accounts for variations in the anatomy of the popliteal fossa ( Fig. 144.3 ).
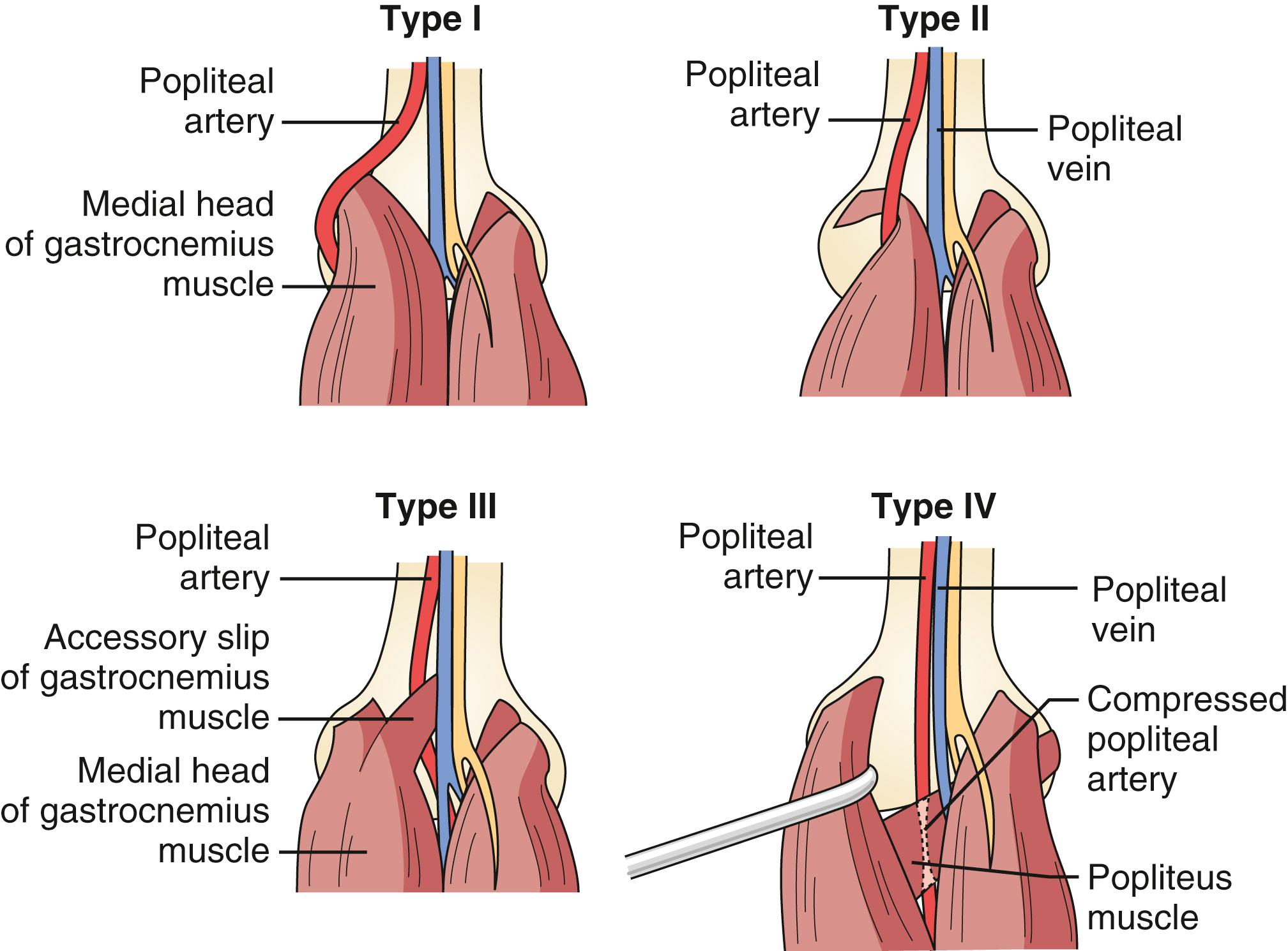
The popliteal artery completes its development before migration of the medial head of the gastrocnemius muscle, which then pushes the artery medially during migration. This results in the popliteal artery’s medial deviation to a normally situated gastrocnemius muscle.
The artery is displaced medially, but the medial head of the gastrocnemius muscle has an abnormal attachment on the lateral aspect of the medial femoral condyle or intercondylar area. In this case, the artery forms prematurely and partially arrests the migration of the gastrocnemius muscle, resulting in the artery positioned medially to an abnormally attached muscle. In contrast to the normal position of gastrocnemius muscle insertion in type I entrapment, type II is defined by an abnormal femoral insertion site.
This type is caused by an abnormal muscle slip or fibrous band that arises from either the medial or lateral femoral condyle. Type III entrapment occurs when embryologic remnants of the gastrocnemius muscle remain posterior to the popliteal artery or when the artery develops within this muscle mass. Occasionally, a double origin of the gastrocnemius muscle can surround and compress the popliteal artery.
Types I to III represent the same anatomic variant, the degree of which depends on the temporal relationship between popliteal artery development and migration of the medial head of the gastrocnemius muscle.
The mechanism resulting in type IV entrapment is fundamentally different from that causing types I to III. Type IV entrapment occurs with persistence of the axial artery as the mature distal popliteal artery. This artery remains in its embryologic position, deep to the popliteus muscle or fibrous bands.
Both the popliteal artery and vein are involved or entrapped by any of the previously described mechanisms. This subtype has been estimated to occur in approximately 10% to 15% of cases. ,
An additional type of entrapment – previously known as functional entrapment, or type F – is now commonly referred to as type VI entrapment. Patients present with the typical features of PAES in the absence of an explanatory anatomic abnormality. It has been proposed that the anatomic abnormality in type VI entrapment is an especially lateral attachment of the medial head of the gastrocnemius muscle to the posterior aspect of the medial femoral condyle. Alternatively, hypertrophy of gastrocnemius following regular exercise is thought to result in compression of the posteromedial aspect of the popliteal artery. When subjected to MRI examination, individuals with type VI PAES and popliteal artery occlusion with stressor maneuvers tend to have a more extensive midline position of the medial head of the gastrocnemius muscle. Compared with normal controls, patients with type VI PAES have more of this muscle attached toward the supracondylar femoral midline, around the lateral border of the medial femoral condyle, and within the intercondylar fossa.
Recent advancements in imaging technologies have led to the discovery of other etiologies for popliteal artery entrapment, such as anomalous slips of the lateral head of the gastrocnemius or plantaris muscles. Such cases are extremely rare and have not warranted a modification of the current classification system.
The pathological classification of PAES describes the continuum of histological changes that result with chronic popliteal compression, from fibrosis of the various arterial layers to complete occlusion and thrombosis. In stage 1, the fibrosis is confined to the adventitia. In stage 2, it extends into the media, which may result in post-stenotic dilatation or aneurysm formation. In stage 3, the artery may become thrombogenic as the fibrosis extends to the intimal layer. The degree of arterial damage does not appear to be related to the duration of compression or popliteal entrapment.
PAES patients are typically young, physically active men who present with lower-extremity claudication. However, a range in the severity of symptoms, along with a grading scale for their description, has been described ( Table 144.1 ).
| Class | Description |
|---|---|
| 0 | Asymptomatic |
| 1 | Pain, paresthesia, and cold feet after physical training (e.g., jogging, heavy work) |
| 2 | Claudication while walking (>100 m) |
| 3 | Claudication while walking (<100 m) |
| 4 | Rest pain |
| 5 | Necrosis |
Claudication symptoms may be atypical and paradoxical, worsening with standing or walking and improving with more vigorous exercise, or they may occur immediately, rather than after walking for a long distance. Patients occasionally describe symptoms of coldness, blanching, and numbness. All types of entrapment (except type VI) can involve the tibial nerves and result in paresthesia. A minority of patients (10%) present with signs and symptoms of chronic CLTI, and even fewer present with acute limb ischemia. Venous entrapment (type V) is suggested by calf cramping or symptoms more typical of a compartment syndrome, including swelling and a feeling of fullness.
Pedal pulses are typically palpable and normal at rest, but disappear with passive dorsiflexion or active plantar flexion of the foot. These maneuvers tense the gastrocnemius muscle against the entrapped artery, temporarily occluding the patent lumen. They should also be performed on the contralateral asymptomatic limb. If left untreated, chronic entrapment causes progressive fibrosis of the popliteal artery, resulting in a thrombogenic intimal surface and eventual arterial thrombosis and occlusion. Occlusion of the popliteal artery can be heralded by the sudden onset of more severe calf claudication and absent pedal pulses. This can occur after an episode of strenuous exercise, and should result in a high degree of suspicion for PAES when it occurs in a young adult with no risk factors for atherosclerosis. Post-stenotic dilatation or aneurysmal degeneration of the popliteal artery, when it occurs, can be a source of distal emboli.
The differential diagnosis for nonatherosclerotic lower-extremity peripheral arterial disease is outlined in Table 144.2 .
| Age | Sex | Key Features | Diagnosis | ||
|---|---|---|---|---|---|
| Popliteal artery entrapment syndrome | Young adults | M > F | Exertional claudication pain, paresthesias, and poikilothermia after exertion External compression of popliteal artery from muscles and ligaments in popliteal fossa |
Loss of Doppler signaling with provocative maneuvers Demonstration of compression on active pedal plantar flexion against resistance CT/MRI to demonstrate entrapment of vascular structures |
|
| Adventitial cystic disease | 4th and 5th decades | M > F | Exertional claudication with extended recovery time compared to aPAD Symptoms caused by compression of arterial lumen by mucinous containing cystic lesion within the adventia |
Loss of pedal pulses with sharp knee flexion (Ishikawa sign) CT/MRI |
|
| Iliac artery endofibrosis | 2nd and 3rd decades | M = F | Competitive athletes, common in cyclists Intimal thickening by collagen fibers, fibrous tissue, and smooth muscle proliferation Femoral bruit with hip flexion |
Arterial duplex ultrasound and digital subtraction angiography with hip flexion and extension Intravascular ultrasound with intraarterial translesional pressure gradients |
|
| Fibromuscular dysplasia | 2nd to 5th decades | F > M | “String of beads” appearance Symptoms based on vascular bed involved |
Digital subtraction angiography with intravascular ultrasound | |
| TAO (Buerger disease) | <50 years | Tobacco smokers, intermittent claudication, Raynaud phenomenon, superficial thrombophlebitis, skipped lesions and corkscrew collaterals | CT/MRI digital subtraction angiography | ||
| Medium and large vessel vasculitis | TA | 15–30 years | F > M | Asian and Latin descent Pulseless upper extremity |
Elevated inflammatory markers Duplex ultrasound CTA MRA temporal artery biopsy (GCA) |
| GCA | >50 years | M = F | Headache, jaw claudication, visual disturbances | ||
| Behçet | <30 years | M = F | Recurrent mucosal ulcers, uveitis, pathergy | ||
| Chronic exertional compartment syndrome | >40 | M = F | Athletes Typically bilateral Complete symptom resolution 10–20 min after rest |
Imaging to rule out other causes Elevated intra-compartment pressures before and after exercise |
|
Exercise treadmill testing is commonly performed as an initial investigation. The patient is instructed to walk or jog until symptoms develop. Ankle–brachial pressure measurements are obtained before and following the treadmill test and should drop significantly. Subsequently, duplex segmental pressures are taken with the Doppler probe placed on the posterior tibial artery. Active plantar flexion and passive dorsiflexion of the ankle with the knee in full extension results in gastrocnemius muscle contraction. Readings are repeated several times, and care should be taken to avoid moving the probe during muscle contractions. Similarly, duplex studies are performed with visualization of the popliteal artery during calf muscle contraction and relaxation. The duplex interrogation must be repeated several times because the popliteal artery can be pushed deeper into the popliteal fossa during muscle contraction, negatively affecting visualization and volume recordings. A positive duplex test with provocative maneuvers should prompt further investigative studies. While some investigators have had excellent results with duplex ultrasound, others have reported high (72%) false-positive studies, resulting in an overestimation of popliteal artery compression.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here