Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Open nerve injuries must be viewed as genuine surgical emergencies. In other words, they should be operated on within the initial hours following the accident. First, it is in an emergency setting that the surgeon encounters the best conditions to ensure matched fascicular group alignment. Second, because associated injuries are common, revascularization of the nerve and its surrounding tissues decreases the epi- and perineural sclerosis from scarring and thereby preserves gliding of the nerve.
This therapeutic approach has often been controversial in previous decades because statistical studies based on series with little homogeneity and with different evaluation criteria have proved to be inconclusive. Furthermore, Millesi presented his method of fascicular nerve grafting to treat nerve defects as an almost universal solution for the secondary treatment of nerve injuries. It was not until statistical studies based on series by Merle and Amend and then Allieu and Desbonnet that it became clear that primary suture offered the best outcomes for nerve injuries in open wounds. A study undertaken in 1993 based on 1794 nerve injury operations in our medical establishment showed that 87.4% of these constituted primary repairs.
This notion of primary repair has been advocated by Bunnel since 1956. He reported on his experience of 1000 repairs and concluded in his study that “the sooner a nerve is sutured in a clean field, the better, and in a fresh wound, by prompt debridement a clean field can often be obtained. This will give the promptest and greatest degree of regeneration.”
Despite the contribution of this significant experience, the secondary repair dogma was not transgressed for a long time, despite the introduction of microsurgical techniques developed by Smith, Kurze, Michon in 1964 and Millesi in 1967. The experimental works of Grabb (1968), Kline (1974), Van Beek (1975) and de Medinaceli (1983) and the clinical experiences of Holst (1975), Merle (1979–1984) and Allieu (1984) finally provided convincing proof that primary repair is indeed superior.
It should be pointed out, however, that despite this favorable therapeutic approach, there remains an incomprehensible level of primary repair failure. A multitude of experimental works have defined some of the anatomic and biological requirements that favor nerve regeneration. Some aspects nonetheless remain poorly understood such as the precise mechanisms by which apoptosis takes place. Furthermore, care must be taken with regard to extrapolating experimental results obtained in rats to that in humans, because the properties of nerve regeneration in rats are not transposable.
In the future, nerve repair is likely to involve genetic engineering to block or limit apoptosis, stimulate axonal regeneration, preserve the neuromuscular junction and avoid muscular atrophy. In the meantime, continued improvements in nerve repair will rely on treating the surrounding tissue so as to limit perineural fibrosis and promote gliding of the nerve trunk by providing coverage with either an adipose tissue flap or a vein wrap. Issues with regard to emergency treatment of nerve defects also need to be considered. Long-term outcomes using neurotubes for small defects have not been convincing.
The emergence of pretreated allografts that do not require any immunosuppressive treatment also needs to be evaluated in the long run, with the knowledge that fascicular autologous transplantation remains the preferred choice to treat these types of tissue loss. Once the surgical repair has been done it is paramount to ensure that the patient undergoes rehabilitative therapy with an emphasis on sensory reeducation, as well as ensuring that an orthosis is used to prevent wrist and finger deformities from forming.
A growing body of anatomic, experimental, electromyographic and clinical considerations has unambiguously established the superiority of primary repair for open nerve injuries.
It is in an emergency setting that the surgeon will be able to achieve the best approximation of the two nerve endings, because he or she is able to evaluate the fascicular organization and epineural vascularization. This is the only time when the nerve ends appear as mirror images of each other, thus facilitating accurate apposition.
Various electromyographic studies performed on monkeys (Grabb, Kline ) and rats (Van Beek ) have provided evidence for the superiority of primary repair. Based on experiments on rabbit and rat sciatic nerves, Becker also observed that a primary repair was better than a delayed one on the second or seventh day.
These works are contrary to those of Ducker (1969–1977), who showed that the metabolic activity of neurons peaks 3 weeks after the axonal injury and that this may therefore be the best time to undertake nerve repair. However, this should not be given further consideration because with late repair the nerve endings must be trimmed, and this triggers renewed retrograde degeneration (1983).
De Medinaceli has clearly shown that everything depends on the initial repair and that attempts at secondary repair, which often end up being multiple, yield worse if not outright poor outcomes.
Based on the same criteria, our cumulative clinical experience since 1976 is proof of the functional benefits conferred by primary microsurgical repair of median and ulnar nerve injuries. Among other things, our efforts in this area have also established the importance of routine repair of the principal vascular axes. Electromyographic studies have also confirmed the high quality of nerve regeneration both at the muscular level and in terms of sensory input. The use of de Medinaceli's method has led to an increase in favorable outcomes. This was assessed by Amara and Chardel, who showed that poor outcomes have indeed been significantly reduced in favor of good, very good and excellent functional outcomes.
The structure and ultrastructure of peripheral nerves are well understood today. On the other hand, the so-called microsurgical perspective is still far from what surgeons might wish for, which is to be able to directly intervene on axons. Nerve microsurgery has only allowed progression from a perineural approximation to a fascicular approximation. Better knowledge regarding the nerve structure, its vascularization and its capacities of regeneration have led to a reevaluation of the technical means required to ensure better coaptation of injured nerve ends.
Nerves have a perifascicular connective tissue sleeve called the epineurium ( Fig. 14.1 ). This extensive structure contains blood vessels, and injury by contusion and hematoma creates a fibrosis that is mechanically detrimental to nerve regeneration. This structure is resilient and allows solid anchoring of suture threads. Reconstitution of the epineurium and perineurium protects the wound from extrinsic colonization by fibroblasts.
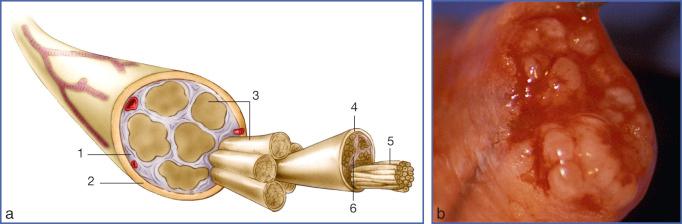
The nerve component that is amenable to microsurgical repair is the fascicular group. Using an operating microscope, it is relatively easy to detect five to six fascicular groups in the median nerve, but higher magnification allows 20–25 fascicles to be discerned. Each fascicle is delineated by a perineural sleeve, which is a veritable barrier between the intrafascicular environment (which is an expansion of the subarachnoid space) and the extrafascicular environment (which is composed of perineural connective tissue).
Myelinated and unmyelinated nerve fibers are found inside the interior of the perineurium, where they are in a connective tissue matrix called the endoneurium. When there is injury, the pressure inside the perineural tube can cause an extravasation of the neural substance, “mushrooming” that becomes worse with intemperate manipulation of the fascicular groups.
In addition, the abundance of connective tissue is also an anatomic factor that must be taken into consideration to achieve good apposition of neural tissue. The median nerve is composed of 63% connective tissue and 37% neural tissue. The ulnar nerve has even more connective tissue, 83%, and 14% neural tissue.
Attempts at intraneural dissection are damaging to the vascularization of the nerve, and the fascicular disorders they cause make coaptation risky, with an increased likelihood of fibroblast proliferation (Lundborg ). It is therefore preferable to preserve the connective tissue to ensure good suture hold and restoration of the epineural seal to combat invasion by fibroblasts.
The arrangement of fascicles within the nerve trunk is complex and subject to substantial individual variation. Sunderland (1945), Bonnel (1977–1985) and Jabaley (1981) have shown that fascicles split and converge to create a bona fide plexiform network every 10 mm. Thus it is impossible to find a connection between two nerve endings. It is thus clear that nerve repair that is neglected in an emergency setting, necessitating secondary neuroma resection, will considerably alter the likelihood of fascicular matching.
This plexiform arrangement dominates at the origin of the nerve and then turns into fascicular groups that separate from each other and form collateral branches destined for sensory and muscle innervation. Thus for the ulnar nerve at the level of the wrist, microdissection makes it relatively easy to distinguish between fascicle groups destined for sensory innervation and groups destined for the intrinsic muscles.
Although a degree of imperfection in the orientation can be tolerated when injuries are proximal, the slightest error in approximation of a distal wound will have a significant impact on the functional outcome by creating wrong connections in the sensory and motor systems.
The excursion of the nerve must be taken into account when the injury is close to the site of a joint. Wilgis and Murphy have shown that the excursion of the median nerve is of the order of 15.5 mm when the wrist goes from complete flexion to full extension.
If the nerve repair is trapped by scar tissue, it will have no mobility. Even indiscriminate rehabilitation done carefully at the third or fourth week postoperatively will create substantial tension on the nerve, thereby causing ischemia and fibrosis that impede nerve regeneration. Regardless of the nature of the injury, it is therefore important even in an emergency setting to appose the nerve ends through the use of a microscope so as to preclude their retraction and restore the tissue environment to minimize scarring around the nerve.
Placing a vein wrap around the nerve repair or wrapping an adipose tissue flap limits perineural fibrosis promotes gliding and facilitates axonal progression, concurrently limiting painful side effects.
Despite improvements in microsurgical suture techniques, we have shown that though primary repair of nerves is superior to secondary repair, satisfactory outcomes in adults are only seen in 46.4% of cases. However, de Medinaceli's technique has changed these outcomes, with satisfactory results seen 80% of the time with repair of the ulnar nerve.
There are numerous factors leading to unfavorable outcomes of nerve repair and thus disappointing results. When the wound is contaminated, scar tissue or even foreign-body reaction occurs at the site of nerve injury. If the repair is poorly performed in a way that causes additional damage to tissues, intraneural vascularization becomes altered. Furthermore, injury of the perineurium can result in unchecked and random axonal growth. Together, all these factors severely compromise the outcome of nerve repair.
Degeneration of the distal ends must also be taken into account because this will create disorder of the regenerating fibers and cause anomalies in reconnection at the neuromuscular junction. Despite the action of nerve growth factors and trophism, satisfactory functional outcomes are not guaranteed. Similarly, retrograde degeneration can occur at the proximal end of the injured nerve.
These conventional issues are not sufficient on their own to explain the disappointingly high incidence of poor outcomes with primary repairs of open nerve wounds. A major factor that must be taken into account is the random nature of nerve outgrowth.
Based on long-term experimental work, de Medinaceli has made the following assertions:
The basal lamina, which wraps around each neurite, plays a fundamental role in outgrowth.
The outgrowth becomes random every time the basal lamina is disrupted.
Rather than the abundance of nerve regeneration, what counts the most is the accuracy of its trajectory.
Directional errors are what underlie imperfections in the joining of neural ends.
Histology studies have shown that nerve endings are very irregular, and the bulky fascicular groups and their respective alignment is not ensured. Blood, cell debris and perineural connective tissue commonly intervene, creating a gap of 100–300 µm between the nerve endings.
An operating microscope is inadequate to detect these cellular misalignments and being able to achieve a good perineural apposition does not mean the axons are aligned correctly. Furthermore, manipulation of the nerve and introduction of suture materials only increases the level of cellular disarray.
Nerve damage due to the injury also triggers chemical changes. All interruptions of axonal integrity are associated with a loss of potassium and proteins, as well as a massive influx of sodium and calcium. The cells are not able to withstand such chemical imbalances, and the nerve endings undergo a bona fide chemical burn over one or two nodes of Ranvier. Thus nerve regeneration does not start at the nerve end, but one or two nodes of Ranvier further back. Because the axon therefore has to regenerate through a no man's land, without support from the basal membrane, its trajectory is largely random.
The hand is innervated by three mixed nerves: the median, radial and ulnar. Injuries proximal to the arm, elbow and the upper third of the forearm create both a sensory and motor deficit. By contrast, the more distal the injury, the more identifiable the deficit in terms of sensory loss. This can be determined by the two-point discrimination (2PD) test or the Semmes-Weinstein monofilament test. The latter test is particularly accurate when partial injuries need to be diagnosed. Testing of motor function is more demanding in the case of major multitissue trauma and can be painful and inaccurate.
Because nerve injuries also frequently entail musculotendinous and vascular injuries, a cursory exploration of the wound is not sufficient. It is paramount to know the time, the action that led to the accident, the causative agent and the degree of contamination. A puncture wound at the wrist, palm or finger can conceal substantial tissue damage.
An open wound with little contamination and no associated injury represents the ideal case. By contrast, evaluation of the extent of the injury is more difficult when there is contusion, avulsion and associated injuries with devascularization and edema.
Even if the nature of the trauma warrants secondary repair of the injured nerve, it is necessary to consider this injury a bona fide emergency so as to ensure tissue revascularization and perform debridement of the wound so the injured individual will not be subjected to necrosis and infection.
In a full-blown emergency setting, electromyographic examinations are not a consideration, because the nerve remains electrostimulatable (so long as Wallerian degeneration has not occurred) until around the third week following the injury.
Nerve microsurgery is a demanding technique that requires laboratory training and the use of specific equipment (see Chapter 3 ). By all accounts, correctly repairing a nerve by microsuture is more difficult than repairing a blood vessel of a millimeter in diameter. The gelatinous consistency of nerves and the intrafascicular pressure that causes extrusion of the neural substance makes them difficult to work with.
Use of a microscope with a magnifying power between 20 and 25 times is desirable if a high-quality repair is to be carried out. Loupes with a magnifying power of 6 may be sufficient for a trained microsurgeon.
Needles with a diameter of 50–70 µm, crimped onto 9-0 or 10-0 monofilament threads, are most commonly used to pass through the perineurium. The perineurium is hard to distinguish optically but can readily be detected owing to its resilient elastic response to passage of the needle.
Microsurgical instruments have been adapted for nerve surgery (Biover). The instruments have round bodies to improve their handling and provide the surgeon with a high level of accuracy and user comfort. To grasp the epineurium, we use titanium tweezers equipped with microclaws ( Fig. 14.2 ). Biover scissors are elongated, which allows the fascicles to be cut in one go. We avoid cutting the nerves with Millesi scissors, however, because this results in the fascicle being crushed over a few tenths of a millimeter, thereby creating a bona fide necrotic segment.

Using a scanning electron microscope, de Medinaceli has shown experimentally that the technique of recutting a nerve is one of the most important elements in improving the coaptation of nerve ends. Although the technique of recutting by controlled freezing is indisputably the best, to date, this cannot be used in the operating room, owing to issues with miniaturization of the equipment. Currently Meyer's “guillotine” clamps represent the best compromise (see Fig. 14.20 ).
To date, we do not consider the use of biological adhesives to be suitable in the setting of conventional primary nerve repair, because the retraction forces exerted on the repair are higher than the adhesion that can be achieved with these materials. By contrast, they are used systematically to perform fascicle grafts.
The choice of suturing techniques has been the subject of numerous and lively controversies. For a long time the epineural suture was the only technique recommended by the majority of surgeons for the repair of nerve injuries. The exceptions were Langley and Hashimoto, who since 1917 proposed fascicular repair; this form of repair was mainly popularized by Tupper with the advent of microsurgery.
Enthusiasm for microsurgery was, however, tempered by the works of Bora and Cabaud in 1976, which showed there was no difference between repairs by perineural and epineural suturing, and that the accumulation of suture material at the level of the perineurium triggered a reaction to foreign objects that created further obstacles to nerve regeneration.
Microsurgical techniques gave surgeons the impression that they could dissect nerves with impunity by interfascicular dissociation for better apposition and suturing of the fascicular groups. Lundborg, however, has shown that this intraneural dissection is not benign; it devascularized the nerve and created an intense sclerosis.
In the same way, microsurgery allows for the option of isolating the fascicular groups of the abundant connective tissue environment. To make nerve repair easier, Millesi proposed resecting the epineurium over a few millimeters. We do not, however, adhere to this technique. Instead we preserve the epineurium, which is the vessel-bearing structure of the nerve, and ensure its closure by sealing it so as to avoid colonization by extrinsic fibroblasts.
Practically speaking, microsurgical techniques have contributed above all to due consideration being given to the nerve and its surroundings, and to minimization of damage by the surgical intervention. In this context it is best to avoid being rigid in one's approach and strictly opposed to epineural and perineural sutures. These techniques are in fact often complementary, and it is necessary to combine different procedures as a function of the trauma to improve apposition of fascicular groups without causing major intraneural disarray.
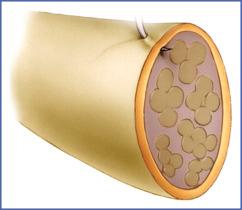
The epineural suture relies on a resilient vessel-bearing connective tissue structure.
To relieve tension at the suture area, we begin with a posterior epineural suture performed with Prolene or Ethilon 7-0. This provides great support for the interfascicular or perineural sutures.
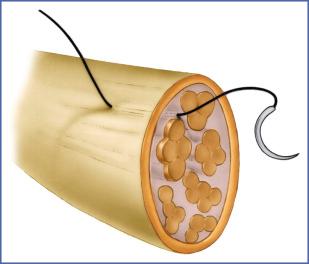
The axial epineural suture originally described by Laugier and reinstated by Tsuge is more logical, because it anchors itself at some distance from the suture area and causes less deformation of the internal organization of the nerve, as shown by Saint-Venant's theory. This suture, which is made with an absorbable PDS 6-0 loop, anchors itself in the epineurium and protects the nerve repair area from tension. Upon completion of the nerve repair, it is preferable to ensure sealing of the epineurium using Ethilon 9-0 or 10-0 by either strictly epineural stitches or epiperineural stitches ( Fig. 14.3 ).
The interfascicular stitch is the most atraumatic. Proposed by Michon, it has the advantage of following a trajectory through the epineural connective tissue, serving as a bona fide guideline providing axial orientation, thereby ensuring overall alignment of the fascicular groups. To facilitate introduction of the needle between the fascicles and to avoid injuring the perineurium, we color the nerve area sections with methylene blue. This measure ensures good visual distinction between the neural and connective tissue. When combined with a perineural suture, this type of suture most often yields the best outcomes for repairs of open nerve injuries ( Fig. 14.4 ).
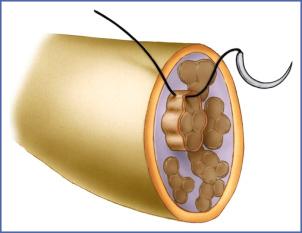
Practically speaking, the repair is performed starting with the clumped fascicular groups. The sutures are made with 10-0 or 11-0 thread mounted on 50- to 70-µm-diameter needles.
Passage through the perineurium is a delicate process because this envelope is both elastic and tough. Owing to the intraneural pressure, intemperate manipulation of the fascicular group will on the one hand cause injury to the perineurium and on the other hand create a mushrooming effect that compromises the apposition of fascicular groups.
To avoid these drawbacks, it is useful to apply counterpressure with microsurgery forceps while threading the needle. The number of sutures per fascicular group must be limited. If the quality of the tissue junction is high, a single stitch may suffice, taking into account the additional support ensured by the interfascicular or epineural stitches.
A strictly perineural repair is not desirable, because instead of having 5 or 6 fascicular groups to be sutured, the surgeon may have 15 or even 20 distinct fascicles that are difficult to join. Intraneural dissection then creates vascular damage. An inflammatory reaction induced by the substantial number of suture stitches may compound this problem ( Fig. 14.5 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here