Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Most benign and malignant tumors of bone and soft tissue are relatively rare, and their occurrence in the region of the elbow is even more unusual. Although there are no valid statistics on soft tissue tumors, compilation of data from the files of the Mayo Clinic until December 2003 indicates that only 1% or so of bone tumors occur at the elbow ( Table 81.1 ). Hence, no single entity is likely to be encountered very often at this site.
| Type of Tumor | Number at Elbows | Total |
|---|---|---|
| Benign | ||
| Osteoid osteoma | 25 | 397 |
| Osteochondroma | 16 | 884 |
| Giant cell tumor | 13 | 682 |
| Chondromyxoid fibroma | 2 | 50 |
| Osteoblastoma | 1 | 108 |
| Fibrous dysplasia | 6 | 671 |
| Aneurysmal bone cyst | 11 | 377 |
| Malignant | ||
| Lymphoma | 38 | 905 |
| Ewing sarcoma | 15 | 611 |
| Osteosarcoma | 16 | 1984 |
| Chondrosarcoma | 6 | 1080 |
| Malignancy in giant cell tumor | 2 | 39 |
| Undifferentiated pleomorphic sarcoma | 1 | 98 |
| Myeloma | 19 | 1069 |
Unfortunately, accurate statistics are not available for benign and malignant soft tissue tumors, although our impression is that the most common benign soft tissue tumor in the elbow region is the lipoma. Ganglia and myxomas are also occasionally seen in this region. Of the malignant soft tissue tumors, epithelioid sarcoma and synovial sarcoma are probably the most frequently encountered at this joint. The locally aggressive desmoid tumor may also occur at or near the elbow. Metastatic disease usually originates from the breast or kidneys.
Tumors of the elbow are unique because there are a relatively large number of important structures in a confined area and there is little normal tissue that can be spared; it is difficult or impossible to remove a tumor with a margin of normal tissue without severely compromising function of the elbow and hand. Tumors about the elbow, particularly in the antecubital fossa, are somewhat comparable to those that occur around the knee. However, upper extremity functional loss is more likely than ambulation because the reconstructive procedures are more developed in the lower extremity. In addition, effective prosthetic function is more problematic in the upper than in the lower extremity. This topic is discussed in detail in Chapter 120 .
For all the reasons stated previously, at the Mayo Clinic, these tumors are addressed by a team of surgeons specialized in orthopedic oncology along with a surgeon with expertise specifically at the elbow. In this chapter we will give some insight into the detail of planning and execution, but the emphasis is on the surgical management at the elbow joint.
As with mesenchymal tumors in other locations, patients usually complain of a lump or pain, or perhaps both. If the mass fluctuates in size, a ganglion or hemangioma may be considered. Limitation of motion is often the first symptom noted. Neurologic symptoms are common due to the proximity of the three major nerves that cross this joint. A long history suggests that the lesion is benign.
The most important consideration is determining the extent of involvement, and this is accomplished with specialized imaging (see Chapter 7, Chapter 8, Chapter 9 ). Following the clinical examination, radiographs in at least two planes should be obtained. The authors rarely employ arteriography today, and instead computed tomography (CT) with contrast is performed to provide this information more simply and safely.
Magnetic resonance imaging (MRI) has proved to be particularly valuable in the assessment of both bone and soft tissue tumors. It is especially helpful to reveal the extent of medullary and soft tissue involvement.
Radioisotopic bone scans may be useful, not only in defining the extent of the lesion in the elbow but also in ruling out additional disease in other sites.
Routine blood chemistries and hematologic studies along with a routine chest radiograph should be obtained in every patient. It should be stressed that as much information as possible should be obtained about the patient and the tumor before any surgical procedure is performed.
An image-guided core needle biopsy, typically performed by radiologists under CT or ultrasonographic guidance, is a common first approach for bone and soft tissue tumors with worrisome radiologic features. An open biopsy procedure may be necessary if the pathologist needs more tissue for histologic analysis and, at times, ancillary studies such as immunohistochemical stains and molecular studies. The open biopsy procedure itself should be done meticulously. The general principle that incisions on extremities should be made vertically rather than transversely holds for the region of the elbow, although for lesions in the region of the antecubital fossa, it may be desirable to make an S -shaped incision with the transverse portion crossing the crease of the elbow.
The staging system of Enneking et al. which includes both soft tissue and bone sarcomas, is useful for malignancies around the elbow. The details of this system are beyond the scope of this chapter.
With improved designs and technique, prosthetic replacement for tumors at the elbow has considerably improved over the years. The majority (90%) of presentations are related to metastatic disease. Satisfactory limited goal outcomes may be expected given that the overall prognosis of these patients is guarded, with a mean survival time of only 3 years ( Fig. 81.1 ).

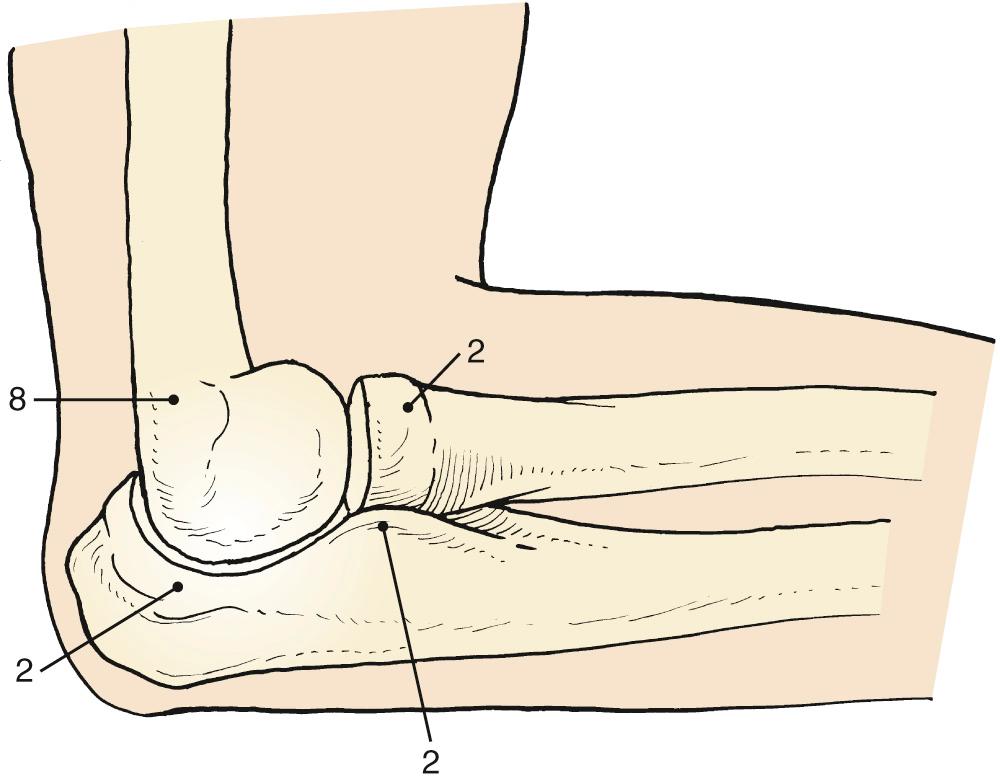
Osteoid osteoma arising in an intraarticular location is relatively uncommon; however, it may occur in the region of the elbow. It is relatively common at the elbow, but only a few reports on the presentation, diagnosis, and management have appeared. This small benign bone tumor occurs in patients of any age, most commonly children and young adults. As with most bone tumors, boys and men are more commonly affected than girls and women. Unremitting pain, especially at night, is the dominating symptom; however, progressive loss of motion is characteristic at the elbow. Occasionally, the pain may be experienced at a site remote from the lesion. Another peculiar feature of this tumor is its occasional association with atrophy of the adjacent soft tissues. In the Mayo Clinic's experience with 14 such cases, eight have occurred in the distal humerus, four in the ulna (two coronoid, two olecranon), and two in the radial head–neck region ( Fig. 81.2 ).
Motion loss with an osteoid osteoma at or near the elbow joint selectively affects the flexion arc, but pronation and supination are preserved. In addition, there may be a synovial reaction that may further confuse the diagnosis. The most striking feature of these tumors is the prolonged average time required for making the diagnosis. In the Mayo Clinic's experience, the delay to diagnosis averaged almost 2 years.
The osteoid osteoma, by definition, is small, usually no more than 1.5 cm in diameter. Lesions that are clinically and histologically similar but are 2 cm or more in diameter are referred to as osteoblastomas; these lesions have clinical features somewhat different from those of osteoid osteoma, but loss of motion is a common feature. Osteoid osteoma is small when first encountered and remains small, a feature that suggests the diagnosis.
An extensive diagnostic evaluation is usually performed but is not necessary to make the diagnosis if one is sensitive to the features described previously. When the patient complains of unremitting pain in the elbow, plain radiographs may or may not reveal the presence of the tumor ( Fig. 81.3 ). The lesion typically appears as a central small nidus, with a radiolucent area surrounded by an area of sclerosis. When the lesion is located on the surface of the bone, there may be periosteal new bone formation that obscures the nidus. A further unusual radiographic feature of subperiosteal new bone formation in adjacent bones has been reported. The authors concluded that “awareness of this association will prevent misdiagnosis of the benign neoplasm as an inflammatory arthritis.”

Technetium-99m scintigraphy has been essential in locating these lesions. If technetium-99m scintigraphy reveals no abnormality, an osteoid osteoma is unlikely; however, if the bone scan is positive, further diagnostic studies of the involved area should be undertaken ( Fig. 81.4 ). If there is any significant synovial reaction, there may be increased uptake owing to the synovitis, as well as to the lesion itself.

Today, thin-section (0.5–2.0 mm) CT and multiplanar reconstructions utilizing bone window are the diagnostic standard to confirm the benign nature of bone reaction and to identify the nidus.
The role of MRI in the evaluation of osteoid osteoma is controversial. A constant finding on MRI scans is marked bone marrow edema corresponding to the highly vascularized mesenchymal tissue. Gadolinium enhancement increases the nidus conspicuity.
Grossly, there is usually some sclerotic bone surrounding a central nidus. This nidus may be somewhat redder than the surrounding cortical bone and has been described as having the appearance of a small cherry. It is sometimes helpful to obtain radiographs of the excised block of tissue before the pathologist cuts into the block. Microscopic examination of the surrounding bone shows no unusual features; the nidus itself consists of a network of osteoid trabeculae (see Fig. 81.3 ).
The classical en bloc resection and curettage is the recommended treatment for patients with juxta- or intraarticular osteoid osteoma. The main problem is identification of the lesion and confirmation of its removal by the pathologist, which may be difficult. Ghelman et al. have described a method for localizing an osteoid osteoma intraoperatively using a scintillation probe. This technique may simplify the localization of the lesion at the time of surgery. Total excision of the lesion guarantees a histological diagnosis, even though it requires a bigger bone excision.
Today, excision of juxtaarticular osteoid osteoma of the elbow may be done arthroscopically, which also affords excellent visualization of the intraarticular sites of involvement. Even when the lesion is so located, complete excision of the larger lesion may be difficult.
Patients whose lesions are not completely excised will probably continue to have the same pain and will require a second operation. The authors have observed that the loss of motion so characteristic of this lesion at the elbow resolves with removal of the nidus. Hence, capsular release is not necessary as an adjunctive procedure.
Whereas laser or radiofrequency percutaneous ablation under CT guidance is highly (90%) effective, its use about the elbow should be done with great caution due to neurovascular and articular proximity. Moreover, local destruction precludes histologic confirmation of the diagnosis, which is important in some instances. In 2014, Albisinni et al. from the Rizzoli Institute reported success in 25 of 27 patients with intracapsular osteoid osteoma using CT-guided percutaneous radiofrequency thermal ablation (RFA).
Osteochondroma is probably the most common benign bone tumor, but it is rare at the elbow. The incidence may be somewhat higher than that reflected in our surgical experience, however, because osteochondromas are often asymptomatic.
The tumor commonly arises from the metaphyseal region of long bones and usually stops growing when skeletal maturity is reached but remains present in adulthood ( Fig. 81.5 ). It may be pedunculated on a stalk or sessile and have a broad base ( Fig. 81.6 ). The tumor is covered by a cartilage cap, which, if greater than 1.5 cm to 2 cm thick, should raise the suspicion of malignant transformation. This occurs in approximately 1% of solitary and up to 5% of multiple osteochondromas.


When multiple bones are involved, severe deformity of the elbow may occur and the risk of malignancy also increases. Hence patients with multiple osteochondromas should be carefully observed through periodic follow-up examination.
Osteochondromas in the region of the elbow may cause painless loss of motion. The tumor may also cause nerve compression and even dislocation of the joint.
If there are symptoms or mechanical or cosmetic difficulties, complete excision of the osteochondroma is performed. Simple excision generally results in cure, although local recurrence has occurred, probably because of incomplete excision of the cartilage cap.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here