Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Neonates and infants often are treated with medicines that have not been approved by regulatory authorities for use in this age group.
The inclusion of infants in drug development studies and clinical trials is limited by difficulties in enrollment, concerns for adverse effects due to developmental limitations, and the lack of universally accepted response variables in many conditions.
Neonatal randomized controlled trials (RCTs) are needed to evaluate the impact of interventions, from practice standards to devices to novel therapies or therapies that were developed for nonneonatal indications.
There is a need for RCTs not only to assess effectiveness and safety of neonatal therapies but also to focus on operational issues and outcomes for regulatory consideration.
Clinical investigations that evaluate interventions/procedures that present the prospect of direct benefit but carry a possibility of greater than minimal risk need review by institutional review boards. There is a need to ensure that the benefit-risk assessment is more favorable than that with alternative approaches.
Neonates and infants often are treated with medicines that have not been approved by any regulatory authorities for use in this population. High-risk neonates and children in general are seen as vulnerable, with their participation in drug development and clinical trials limited by numerous factors. Some of the reasons that so few products have been developed for neonates and children include gaps in understanding complex pathophysiology, a small market with many conditions involving rare diseases, challenges in the design and execution of clinical trials (including the need to wait for long periods of time to assess some clinical outcomes), and difficulties with the assessment of safety and efficacy. This has resulted in children being referred to as “therapeutic orphans.”
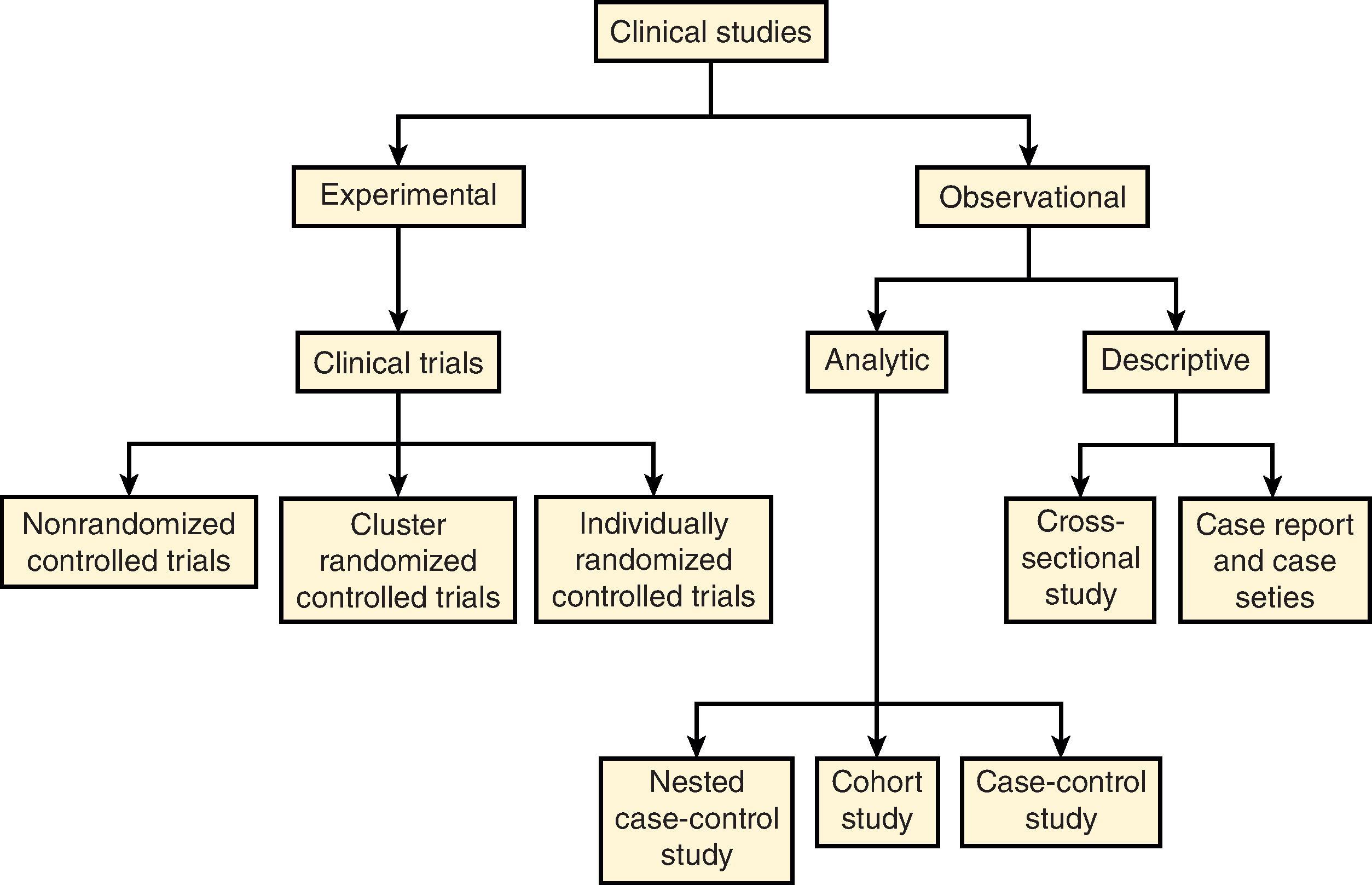
This chapter will review fundamentals of the design and conduct of clinical trials in neonates and young infants. Although randomized controlled trials (RCTs) are considered the “gold standard,” the use of alternative designs (e.g., cluster randomized trials) will also be discussed ( Fig. 98.1 ). Ethical considerations, including issues related to informed consent, will be presented along with the need for engagement of parents and neonatal intensive care unit (NICU) staff in the trial design process.
The likelihood that a clinical study will answer the research questions posed in a reliable manner, meaningful for decision makers and patients, while preventing important errors, can be dramatically improved through prospective attention to the design of all components of the study protocol, procedures and associated operational plans. —From the International Council for Harmonisation (ICH) E8(R1) Draft Guideline
Randomized, double-masked or blinded, placebo- or standard of care–controlled clinical trials have provided many of the key advances in neonatal therapeutics. Surfactant replacement for respiratory distress syndrome, caffeine for apnea of prematurity, therapeutic hypothermia for hypoxic-ischemic encephalopathy, and inhaled nitric oxide for persistent pulmonary hypertension of the newborn are among the most significant therapeutic successes in neonatology. Despite these successes, RCTs of preventive agents or therapies for conditions such as bronchopulmonary dysplasia and neonatal hypotension have not produced clear evidence of clinically meaningful benefit for any of the therapies studied.
RCTs remain an essential tool for assessing the effectiveness and safety of neonatal therapies, both novel therapies and those whose efficacy and/or safety may be unclear. It has been recognized that clinical trials may either fail to show an effect or fail to provide useful data due to problems with elements of design and implementation. “Quality by design” is an approach that relies on sound prospective design and execution plans such as (1) focusing on protecting human subjects, (2) determining predefined objectives, (3) selecting appropriate study participants, (4) minimizing bias, (5) controlling confounding, (6) choosing measurable and well-defined study endpoints and methods of assessment, and (7) addressing operational and feasibility criteria. ,
The U.S. Department of Health and Human Services (HHS) and the Food and Drug Administration (FDA) require special protections for the inclusion of children in research. These protections are defined under HHS 21CFR§50, Subpart D, as the “Additional Safeguards for Children in Clinical Investigations” and under FDA 45CFR§46, Subpart D, as the “Additional Protections for Children Involved as Subjects in Research.” The principles are the same, but the HHS and FDA Subpart D guidelines differ slightly in scope. The HHS regulation applies to “all research involving children as subjects, conducted or supported by HHS,” whereas the FDA regulation applies only to studies of an FDA-regulated product.
Under Subpart D, an institutional review board (IRB) can approve clinical investigations involving children that fall into the following categories:
not greater than minimal risk,
greater than minimal risk but presenting the prospect of direct benefit to individual subjects, or
greater than minimal risk and no prospect of direct benefit to individual subjects but likely to yield generalizable knowledge about the subjects’ disorder or condition.
An IRB may determine that a study presents no more than minimal risk if all the interventions or procedures within the clinical investigation do not exceed minimal risk. Such studies may proceed with the permission of one parent or guardian. Minimal risk is difficult to define but is indexed to the risks for the population in their daily life, including routine examinations. In the case of hospitalized neonates, a single blood draw (preferably with routine labs), bagged urine specimen, or a single chest radiograph may be considered minimal risk.
Interventions or procedures within a clinical investigation that convey greater than minimal risk but present the prospect of direct benefit (PDB) are reviewed by IRBs to ensure that the risk is justified by the anticipated benefit and that the benefit-risk assessment is at least as favorable to participants as would be available with alternative approaches. Permission of one parent or guardian must also be obtained for research approved under this category. Protocols should clearly describe available alternatives to the investigational therapy and any adverse events and long-term consequences if known. A comprehensive understanding of therapeutic alternatives is critical to benefit-risk assessments for IRBs and regulators. An example of a study in this category may include evaluation of a novel therapy in a pediatric population for which the PDB to the child has been established and justifies the risk of exposure. Such an assessment should include whether there is adequate evidence to establish proof of concept to support a benefit and whether the proposed dose and duration of therapy are sufficient to offer a potential clinical benefit ( Table 98.1 ).
| Factors That May Support a Prospect of Benefit for a Novel Therapy | Tools to Support Benefit and Minimize Burdens/Risks |
|---|---|
| Evidence to support proof of concept | |
| Biological plausibility and scientific justification for the proposed mechanism of action and its expected effect in the condition of interest | Evaluate existing scientific rationale, summarize available experimental and observational data |
| Nonclinical evidence ( in-vitro mechanistic studies, in-vivo studies in animal models) | In vivo data in animal models of disease can provide insight into the impact of the intervention on pathophysiology as well as dosing strategy |
| Clinical evidence in adults or older children with similar and/or relevant conditions | Efficacy responses may support benefit and data on adverse effects can provide important information to guide monitoring in a neonatal clinical trial |
| Structure of the study intervention | |
| Dosing justification including evidence to support that the proposed doses are likely to have the intended treatment effect |
|
| Trial duration |
|
Interventions or procedures in a clinical investigation that pose greater than minimal risk (referred to as a “minor increase over minimal risk”) without a PDB for individual subjects but that is likely to yield important, generalizable knowledge about the participant's condition may be approvable if the minor increase is commensurate with expected medical experiences for the subject. Clinical investigations approved under this category require permission of both parents.
An example of a clinical investigation that might be allowed to proceed with a minor increase over minimal risk would be the evaluation of a single dose of an investigational product solely to collect pharmacokinetic data for which adequate safety data exist to characterize the risk as no more than a minor increase over minimal risk. For a clinical investigation to proceed under this category, all the interventions and procedures in the protocol (e.g., blood draws or any diagnostic testing) also need to be no more than a minor increase over minimal risk. This analysis is called a component analysis of risk , used to determine the overall acceptability of the clinical investigation including the risks and anticipated benefits of the interventions that are listed in the protocol (which must be analyzed individually as well as collectively). ,
For RCTs of interventions to treat a disease or condition, study participants should have the disease or condition with clear and reproducible diagnostic criteria. If the disease or condition is ill-defined either physiologically or clinically, enrolled patients may be a heterogeneous group. Identifying a potential treatment effect may be impossible in a study that enrolls patients with variable manifestations of a condition.
For RCTs of interventions to prevent a disease or condition, study participants must be at significant risk for developing that disease or condition. When the risk of a disease is low in a given population, participants could be enrolled in a study and exposed to an experimental intervention to prevent an infrequent outcome. In this scenario, understanding the safety of the study intervention is critical to any benefit-risk assessment. Strategies to identify a population at higher risk of the condition should reduce the proportion of enrolled neonates who would likely not have developed the condition. Enrichment strategies may include well-evaluated biomarkers and/or risk scores that are derived from clinical data.
Inclusion and exclusion criteria should be clearly defined and used to capture the population for whom the intervention is intended. Early-phase studies of a novel therapy in neonates may require study in a relatively homogeneous population to balance the unknown risks with the potential for individual benefit. Once more is known about the product's safety profile, later-phase RCTs may be able to enroll a more heterogeneous sample of patients that is similar to the intended use population.
Neonatal RCTs may evaluate the impact of interventions, from practice standards to devices to novel therapies or therapies that were developed for nonneonatal indications. Subpart D guidelines, as discussed above, help guide the benefit-risk assessment for a trial protocol. An intervention that conveys more than a minor increase over minimal risk must provide a PDB to participants, with rare exceptions. In this category, clinical equipoise is assumed—the “honest, professional disagreement among expert clinicians about the preferred treatment” and IRBs must determine whether the potential benefit justifies the risks. PDB can be established based on information from the literature, animal models, other nonclinical studies, and/or proof-of-concept studies in humans. Study protocols should include all available nonclinical and clinical evidence to support both PDB and safety to inform IRBs and regulatory bodies.
Nonclinical toxicology studies that support drug approval in adults or older children may not be sufficient to inform the safety of a treatment in the neonatal period. When a drug's impact on developing organ systems is unknown, juvenile animal studies can inform safety and/or dosing parameters. Safety and tolerability information from healthy adult volunteer studies may also be needed to support neonatal studies if the drug has not been previously given to humans.
The importance of establishing effective and safe dosing strategies prior to initiation of large RCTs cannot be overstated. Thoroughly evaluating existing pharmacokinetic information and drug absorption, distribution, metabolism, and excretion data is critical to optimizing the dosing strategy and reducing the chance of trial failure due to suboptimal dosing. Although dose selection is typically confirmed in phase 2 studies, later RCTs may incorporate more than one dosing regimen for confirmation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here