Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
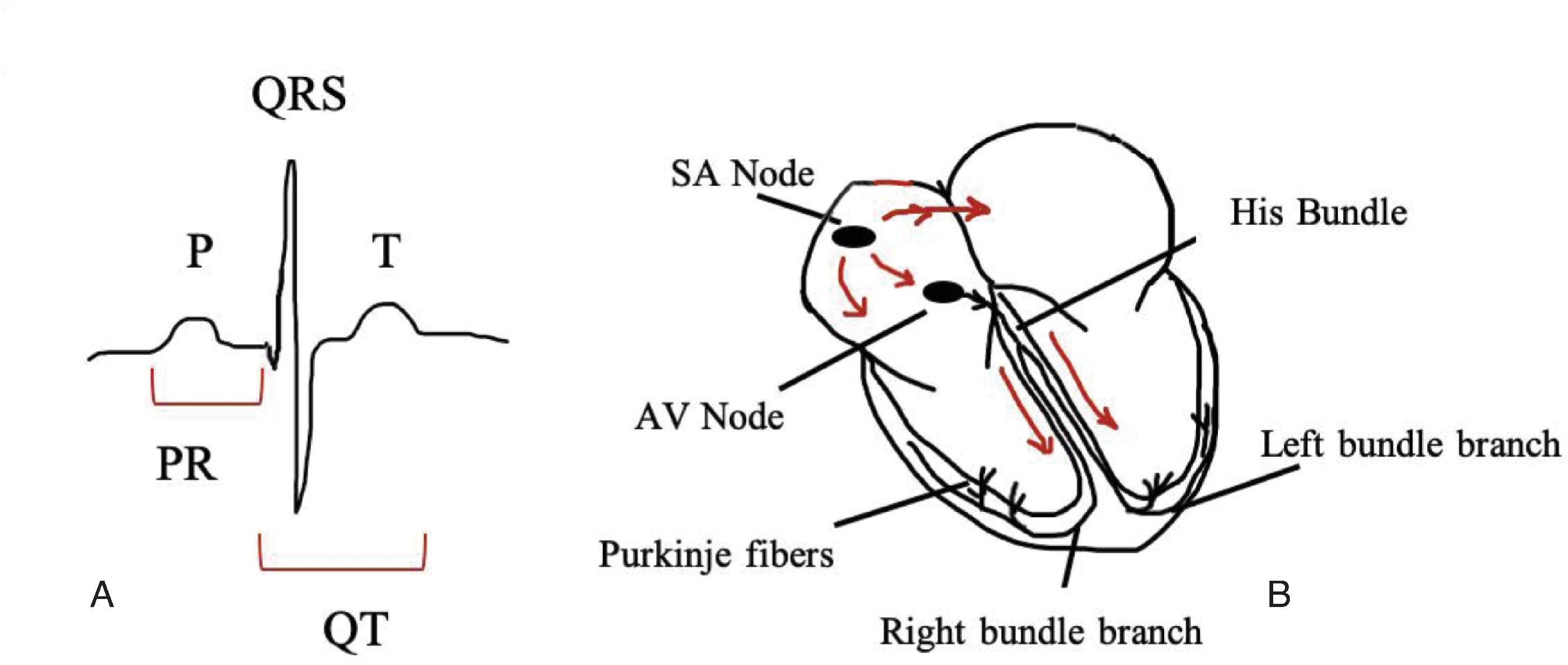
The normal cardiac electrical signal travels from the atria to the ventricles through a conduction system comprised of the sinus node, atrioventricular (AV) node, His bundle, and Purkinje system.
The AV node normally regulates the electrical action potentials from the atria to the ventricles. In some instances, the electrical signal bypasses the decremental AV node via an accessory pathway. AV block is a disturbance in conduction between the atrial depolarization and the ventricular response and may occur anywhere along the AV node–His bundle system.
Long QT syndrome (LQTS) refers to an abnormality in ventricular repolarization and is associated with syncope and sudden death.
Arrhythmias are relatively common in the neonatal period and can range from benign premature atrial contractions to wide-complex ventricular tachycardia (VT). Atrial arrythmias include the supraventricular tachycardias, which may be tolerated in the short term but can cause cardiovascular compromise over longer periods. Atrial flutter is a rapid atrial tachycardia due to a reentrant circuit revolving around the tricuspid valve.
Wide complex tachycardias from ventricular loci are uncommon in neonates. Rapid polymorphic VT or ventricular fibrillation can be seen in patients with channelopathies such as LQTS.
In normal sinus rhythm, the electrical signal travels from the atria to the ventricles through the conduction system, comprising the sinus node (SA node), atrioventricular (AV) node, His bundle, and Purkinje system ( Fig. 39.1 ). After the electrical signal reaches the end of the Purkinje system conduction, depolarization of the ventricle is completed through cell-to-cell activation from ventricular myocyte to ventricular myocyte. The cells then must complete repolarization prior to the next heart beat and activation. Pathology along any portion of the electrical conduction pathway will lead to varied conduction defects.
The role of the AV node is to conduct electrical action potentials from the atria to the ventricles. The AV node has decremental properties and therefore slows the electrical impulse from the atria to the ventricles. By causing a delay between the atrial contraction and the ventricular conduction, this decremental property of the AV node allows for enhanced ventricular filling due to ventricular contraction following the atrial kick. Abnormal signal conduction along the AV node can lead to relatively benign presentations such as first-degree AV block or pathologic defects such as third-degree heart block. Alternatively, in instances when atrial to ventricular conduction can bypass the decremental AV node, such as with accessory pathways, a short PR interval results and alters the sequence of ventricular activation (this is a feature of Wolff-Parkinson-White [WPW] syndrome).
AV block is a disturbance in conduction between the atrial depolarization and the ventricular response and may occur anywhere along the AV node–His bundle system. In adults, the most common etiology for AV conduction delay is not related to structural disease but rather to progressive fibrosis. In neonates, congenital heart block is defined as the presence of AV conduction system disease in any form diagnosed prior to 29 days of life, with an incidence of 1 in 22,000 live births. When diagnosed postnatally, congenital heart disease is associated with approximately one-third of AV conduction delays; however, when diagnosed prenatally, approximately one-half have congenital heart disease, most commonly left atrial isomerism and L-transposition of the great vessels. When fetuses with congenital heart block have structurally normal hearts, a majority had exposure to maternal autoantibodies.
AV block is designated as one of three degrees (first, second, and third), with nomenclature also including the ratio of atrial to ventricular contractions (1:1, 2:1, 3:2, etc.). Because the block occurs below the sinus node, the PP interval stays constant and can be marched out through any of the AV blocks, although the PR interval may change.
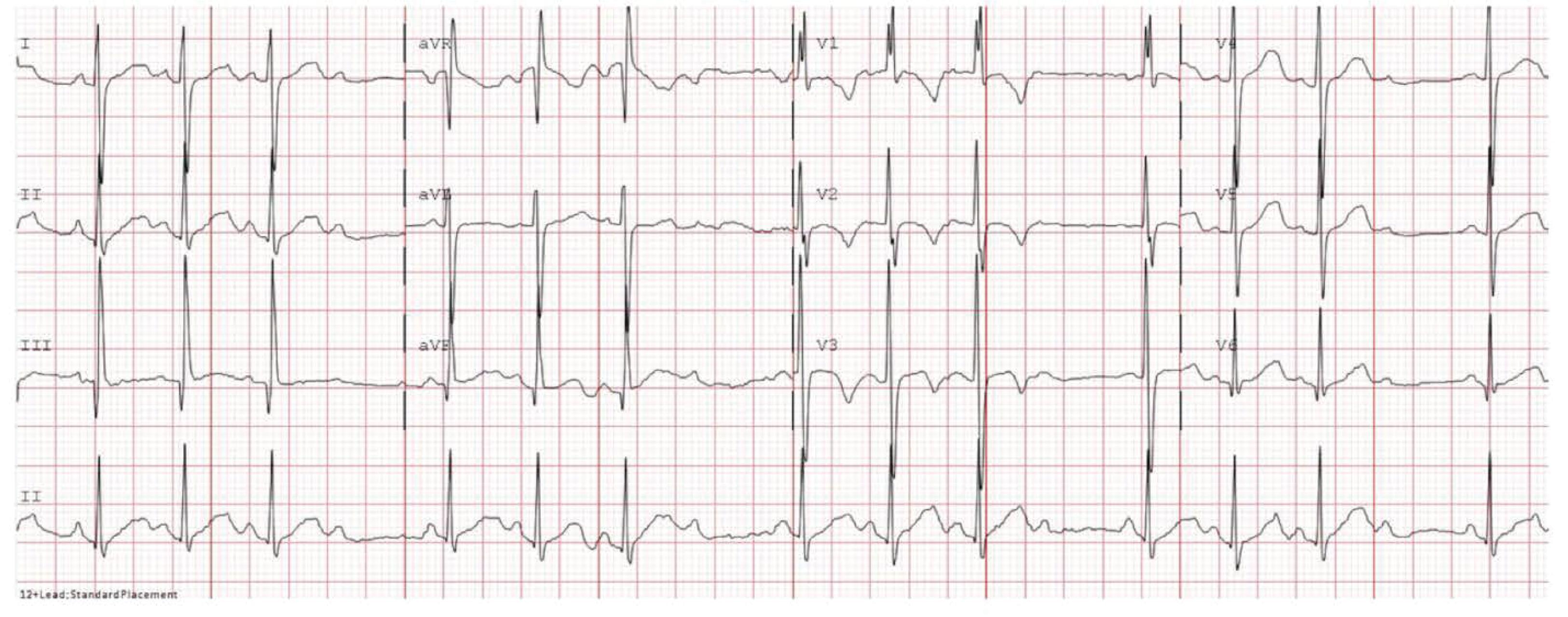
First-degree AV block is defined as a delay between atrial and ventricular conduction and is most commonly due to delays through the AV node (although slow intraatrial conduction can also be responsible ). In first-degree AV block, the PR interval is prolonged beyond the upper limits of normal for the patient’s age and heart rate, but a 1:1 atrial to ventricular contraction ratio is maintained. The PR interval includes (1) the time required for depolarization of the atrial myocardium from the start of the atrial contraction to its reaching the AV node (sometimes denoted as the PA interval, from onset of the P wave to the A wave on the His bundle electrocardiogram [ECG]), (2) the delay of conduction in the AV node (AH interval; the time interval between the onset of the atrial signal and the onset of the His bundle signal in His catheter recording), and (3) conduction through the bundle of His until the time of onset of ventricular depolarization (HV interval) ( Fig. 39.2 ). First-degree AV block can be seen in otherwise healthy young individuals and in athletes, which is generally due to increased vagal tone. Other less frequently implicated causes include congenital heart disease, infectious and inflammatory conditions, and drugs (such as digoxin or beta blockers). In the absence of heart disease, a prolonged PR interval does not typically progress to further degrees of block or produce hemodynamic instability; intervention is therefore not generally required. , A congenital prolonged PR interval does not typically progress to higher-grade block in neonatal life. In a cohort of 32 fetuses with exposure to maternal autoantibodies that can lead to heart block, eight developed first-degree AV block in utero. All had resolved by the first month of life without intervention in pre- and postnatal life.

Second-degree AV block is defined by interruption in conduction, typically within the AV node, where some, but not all, P waves result in a QRS, thus resulting in dropping of one or more ventricular beats. Second-degree AV block is usually divided into two patterns, Mobitz type I (Wenckebach) and Mobitz type II. For the purpose of this chapter, Mobitz type I and Wenckebach will be used interchangeably.
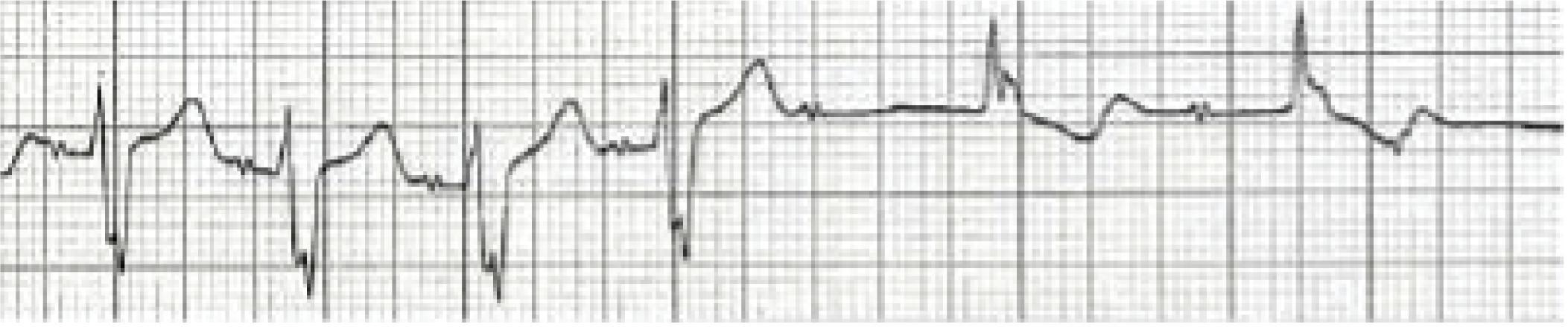
In Mobitz type I, the PR interval becomes gradually prolonged from beat to beat as the AV node progressively fatigues until one QRS complex is dropped ( Fig. 39.3 ). Most examples of Wenckebach AV block in neonates demonstrate a narrow QRS, are asymptomatic, do not require intervention, and are related to medications or maternal connective tissue disease. , Wenckebach is generally related to abnormalities within the AV node and is manifested as prolonging PR intervals due to the ability of the AV node to decrement (prolonged conduction).
Mobitz type II AV block is a far rarer cause of second-degree block in neonates and generally occurs as a result of block in the distal conducting pathway below the AV node. Mobitz type II block presents with intermittent dropped ventricular beats without any prior prolongation of the PR interval and can rapidly progress to complete AV block ( Fig. 39.4 ). In addition, because a junctional escape rhythm cannot conduct to the ventricles during severe Mobitz II block, very slow (if any) escape rates can be seen with progressive Mobitz II block. Mobitz type II block therefore has a more ominous prognosis, and permanent pacemaker placement is often recommended. Causes of Mobitz type II include myocarditis, cardiomyopathies, widespread sclerodegenerative conduction disease, myocardial infarction, congenital heart disease, and cardiac surgery. , ,
In the setting of 2:1 AV conduction, differentiating Mobitz I from Mobitz II conduction can be difficult. A prolonged PR during 2:1 conduction suggests Mobitz I block, but with a normal PR interval, either is possible. An additional consideration in the neonatal (and fetal) period is that 2:1 AV block can be a manifestation of long QT syndrome (LQTS) (where a prolonged repolarization period does not allow conduction through the ventricle when the next signal appears). As a result, LQTS (whether congenital or acquired) should be considered when 2:1 AV block is seen in the neonate.
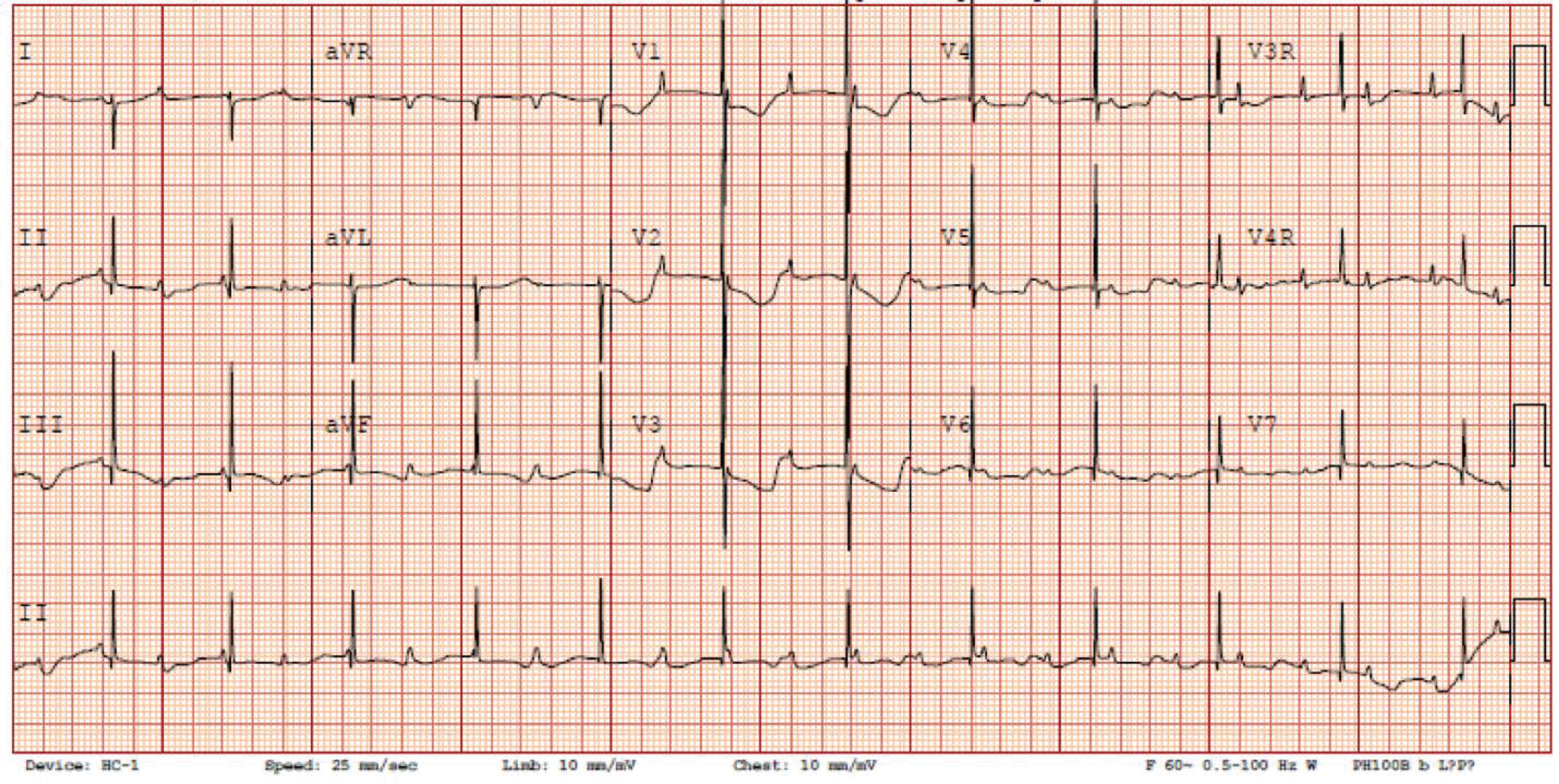
In complete heart block (CHB), also referred to as third-degree AV block, the atrial and ventricular activations are entirely independent of each other ( Fig. 39.5 ). Atrial impulses are not conducted to the ventricles through the AV conduction system, and the ventricles depolarize in response to a subsidiary intrinsic pacemaker, usually resulting in a slow escape rate. As with the previously discussed AV blocks, the P waves are regular, with regular PP intervals, and with an atrial rate usually comparable to the normal heart rate for age. The QRS complexes are also usually very regular but at a much slower rate than the P wave rate. A narrow QRS complex indicates that the subsidiary pacemaker (escape rhythm) is junctional and originates above the bifurcation of the bundle of His. Alternatively, a wide-complex escape rate suggests that the subsidiary pacemaker originates in the ventricular muscle (see Fig. 39.4 ). Most cases of congenital CHB have a narrow QRS complex and typically have a higher escape rate than is seen with wide-complex escape; these narrow-complex escape rates can vary in response to physiologic conditions. During slow escape rates, cardiac output can be maintained by augmenting a slow heart rate with a stronger myocardial contractile force, a long diastolic filling time, and an increased end-diastolic volume resulting in an increased stroke volume.
CHB can be divided into congenital and noncongenital forms as well as immune and nonimmune forms. The most common cause of congenital immune CHB is exposure to maternal autoantibodies. Nonimmune congenital forms of CHB are usually associated with structural heart disease such as left atrial isomerism, complete AV canal defects, and congenitally corrected transposition of the great arteries (accounting for approximately 14%–42% of cases of congenital CHB). Noncongenital forms of CHB are usually due to AV node injury during congenital heart disease surgery; other forms of noncongenital CHB are extremely rare in the neonatal period.
Heart block affects an estimated 2% to 5% of infants born to primigravid women with anti-Ro/SSA and anti-La/SSB antibodies, and the risk is as high as 15% to 20% in women who have had a previously affected newborn. , CHB can result in significant morbidity, and mortality rates of up to approximately 20% have been reported, with the following factors associated with increased mortality: diagnosis in fetal life (particularly <20 weeks’ gestation), presence of fetal hydrops, delivery prior to 33 weeks’ gestation, ventricular rate <50 bpm, and decreased LV function. , , Anti-Ro/SSA and/or anti-La/SSB bind to fetal cardiac tissue and cause an immune-mediated injury to the AV node and its surrounding tissue. Although most signs and symptoms in neonatal lupus are transient and disappear as the maternal antibodies fade within the first 6 months of life, congenital heart block is caused by fibrous replacement of the AV node and is frequently permanent, especially when third-degree AV block is present. In addition to congenital heart block, antibody-mediated cardiomyopathy may occur with neonatal lupus, with cardiac failure due to cardiomyopathy a leading cause of early death. A majority of patients with congenital CHB require a permanent pacemaker before adulthood, with one study reporting an epicardial pacemaker approach in the majority of patients at a median of 10 days after birth. Permanent pacing is a Class I indication for the symptomatic individual with congenital complete AV block or the infant with a resting heart rate of <55 bpm, or <70 bpm if associated with congenital heart disease.
Standardized therapy for congenital CHB in utero is lacking. In patients with congenital CHB and normally structured hearts, early access to pacing wires immediately after birth is associated with improved survival. Once in-utero CHB develops, it is generally irreversible, with goals of fetal therapy to halt advance to higher degrees of block and reduce clinical compromise and development of hydrops. Although there is no standardized management due to lack of definitive efficacy, antenatal medical therapies that have been utilized include steroids to mitigate the inflammatory response, plasmapheresis and intravenous immunoglobulin (IVIG) to reduce autoimmune antibodies, and beta-sympathomimetics to increase heart rate and augment cardiac output. , Studies have demonstrated mixed benefit to providing steroids to mothers with fetuses in CHB, and with the risks to mother and fetus of steroid administration, such as risk of maternal diabetes and risk of postnatal neurodevelopmental delay, there remains no generalized recommendation for steroid administration in utero for CHB. , ,
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here