Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The distinctiveness of the connective tissue diseases is less pronounced than the classification system implies. In practice, there is a continuous spectrum of symptom combinations, merging features of various entities. Mixed connective tissue disease (MCTD) is the prototype of an overlap syndrome, combining features of systemic lupus erythematosus (SLE), systemic scleroderma (SSc), polymyositis (PM), and rheumatoid arthritis (RA). As described by Sharp and colleagues, MCTD constitutes a likewise separate entity and is now, despite previous debate, a commonly used label for the anti–U1-ribonucleoprotein (RNP)–associated disease spectrum.
The etiology underlying this special symptom combination is unknown. There are several hypotheses, such as the induction of autoantibodies due to molecular mimicry after retrovirus infection (or Epstein-Barr virus infection) or defects in the clearance of apoptotic cells similar to SLE concepts. The exact prevalence and incidence rates are unknown but estimated to be approximately one of every four SLE patients. A Norwegian study found a point prevalence of 4 per 100,000 adults and an incidence of adult-onset MCTD of 2 per million and year. The female predominance is threefold to tenfold. Genetic studies show mostly human leukocyte antigen (HLA)-DR4 and HLA-Dw4 association, a genetic background that is different from that of SLE patients.
Due to the overlapping nature, MCTD does not present a constant clinical picture, and individual patients often exhibit a symptom shift. Approximately 40% of patients initially classified as having MCTD will evolve into another defined connective tissue disease during disease progression, most often into SSc (initially often associated with hypomotility of esophagus), SLE (initially often associated with the presence of anti-DNA antibodies), and undifferentiated connective tissue disease (UCTD), a minority into RA or overlap syndromes. Uncompleted forms or partial remissions are not uncommon, and diagnosis may remain limited to UCTD. This term, however, has received its own definition and can self-sufficiently serve as a basis for patient care. In patients with Raynaud phenomenon, factors have been defined that have prognostic significance for the future development of a specific connective tissue disease. Most patients with UCTD and anti–U1-RNP develop MCTD.
Nonspecific signs, such as fatigue, weight loss, and fever, are often associated with more specific manifestations, the latter including:
Puffy hands, swollen fingers
Raynaud phenomenon
Keratoconjunctivitis sicca
Arthralgia, unexplained polyarthritis myalgia, myositis
Skin symptoms: rash, sclerodactyly
Esophageal dysfunction
Central nervous system symptoms, peripheral neuropathy
Fibrosing alveolitis and pulmonary hypertension
Serositis
Adenopathy, hematologic disorders
Presentation with symptoms of two or more well-defined connective tissue diseases (SLE, SSc, RA, PM) is typical. Even the characteristic feature of swollen hands may incorporate signs of more specific diseases, for example, erythema of the dorsum of the proximal interphalangeal joints and metacarpophalangeal joints, as in PM or sclerodactyly, and fixed finger flexion, as in SSc.
Serologic findings include raised erythrocyte sedimentation rate and elevated C-reactive protein, which are nonspecific signs of inflammation. The presence of antibodies against U1 ribonucleoprotein (anti–U1-RNP) is fundamental for the diagnosis and has been initially stressed to be specific. Currently, it is known that high titers can also be found in 40% of patients with SLE, as well as in some cases of SSc, RA, PM, and other overlapping syndromes. IgG and complement levels are usually high. In addition to clinical overlap, serologic overlap has also been recognized. Antinuclear antibodies (ANA) and rheumatoid factor (Waaler-Rose test as well as enzyme-linked immunosorbent assay) may be found in patients with MCTD, and anti–ds-DNA and anti-Sm suggest SLE.
Sharp and colleagues initially described a favorable prognosis. However, this notion has been disproven; myositis, renal disease, as well as fibrosing alveolitis and pulmonary hypertension are potentially fatal, and, therefore, the overall prognosis is worse than that for SLE.
Multiple classification criterion sets have been proposed because of the variability of the disease presentation and course. The best approach is still a matter of debate. Alarcón-Segovia and Cardiel's criteria include five clinical criteria only. Prerequisite is a high titer of anti–U1-RNP; however, the exact levels for assays commonly used have not been described. Clinical criteria are swollen hands, Raynaud phenomenon, acrosclerosis, synovitis, and myositis. According to Alarcón-Segovia and Cardiel, MCTD can be diagnosed with reasonable specificity and sensitivity when in addition to the serologic marker, three clinical criteria are present. If the criteria of swollen hands, Raynaud phenomenon, and acrosclerosis are positive, one of the other two criteria is additionally necessary. Kasukawa and colleagues' criteria set seems to be more sensitive. Fulfillment of the criteria of another connective tissue disease (RA, SLE, SSc, PM) in a patient with the positive diagnosis of MCTD should not be considered an association but refers to the nature of MCTD being an overlap syndrome itself. It is found in approximately 16% of patients.
Depending on the clinical and serologic expression of the different entities, the radiographic picture will reflect the corresponding features, sometimes of multiple features in an atypical mixture. Then the overlapping nature of the disease is once more confirmed. Bone and soft tissue abnormality often resemble SSc. Joint involvement is more variable and shows features of RA or SLE, sometimes with a slightly atypical pattern ranging from mild effusion to mutilating arthritis. Any joint may be affected, although there is a clear predominance for the small joints of the hand and feet. In most cases, only nonspecific signs are radiographically present (e.g., demineralization and soft tissue swelling).
RA features such as synovitis, joint space narrowing, marginal erosions that progress to destruction, and deformities with predilection for the metacarpophalangeal and proximal interphalangeal joints, wrist, and metatarsophalangeal and interphalangeal joints can be seen ( Fig. 54-1 ). Slightly atypical RA manifestations have been stressed to be typical for MCTD, that is, asymmetric involvement, distal interphalangeal joint involvement, and postarthritic capitate-trapezoid ankylosis.

Punctate, linear, or extensive soft tissue calcification with predilection for the fingertips and periarticular region as well as subcutaneous location is not uncommon (see Fig. 54-1 ). Acral soft tissue atrophy, tuftal resorption, and bandlike distal interphalangeal joint destruction occur in patients with SSc parameters ( Fig. 54-2 ). The combination of erosive arthritis with soft tissue calcifications is the most impressive radiologic feature but is not very frequent.

Deformity without joint destruction is some hint of an SLE component (see eFig. 54-1AB ). Avascular necrosis of the femoral or humeral head, femoral condyles, diaphysis, carpal bones, and metacarpal heads may occur with or without corticosteroid therapy, just as in SLE, and presents with the familiar aspect seen in otherwise healthy individuals (see eFig. 54-1C ) (see Chapter 71 ).

Unsurprisingly, soft tissue abnormalities are detected with significant superiority by means of ultrasound compared to radiography. Synovitis of the tendon sheath and tendinopathy as well as arthritis are highlighted just as in RA and SLE. Features of arthritis are known from rheumatoid arthritis: synovitis is characterized by effusion and synovial hypertrophy of various amounts and is often enough found in clinically silent joints. The addition of Doppler highlights hyperemia of the thickened synovium and indicates active inflammation. A number of studies have shown that ultrasound imaging has a higher sensitivity for bone erosions than radiography, due to its ability to scan almost the entire bone surface.
Ultrasonography emerges as a powerful diagnostic tool. The differentiation of early stage arthritis in different rheumatic diseases, however, is a major problem, and most literature covers rheumatoid arthritis. Puffy hands are characterized by edema of the subcutaneous structures and extensor synovitis, which remains nonspecific.
For MRI of the hands, it has already been shown that the features of early rheumatic disease do not allow the differentiation of separate entities. Nonspecific findings of tenosynovitis, tendinosis or tendon rupture, joint effusions, pericapsular edema, and bone marrow edema have been described in MCTD. The subcutaneous edema may be pronounced (see eFig. 54-2 ). It has been suggested that the small number of published cases may be a reason that no characteristic MRI pattern for MCTD has been identified as of yet. However, this disease is characterized by a highly variable combination of features of several entities, which can confound MR imaging classification.
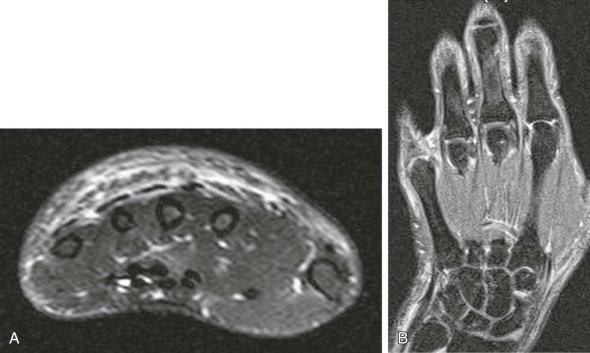
On MRI, arthritis is characterized by effusion, synovial hypertrophy, bone marrow edema, and erosions. In active disease, the pannus is hyperintense on short tau inversion recovery (STIR) images with enhancement postcontrast. Bone marrow edema is well seen on MRI, and, in RA, this has been shown to be a prognostic factor of progression. MRI shows a higher number of erosions than radiography, in part, because of the cross-sectional technique allowing to highlight the complete articular surface without superimposition effects, in part, corresponding to true pre-erosions. The natural history of MRI erosions in RA has been described for rheumatoid arthritis. Some of them persist in the pre-erosional stage, some progress, and some regress.
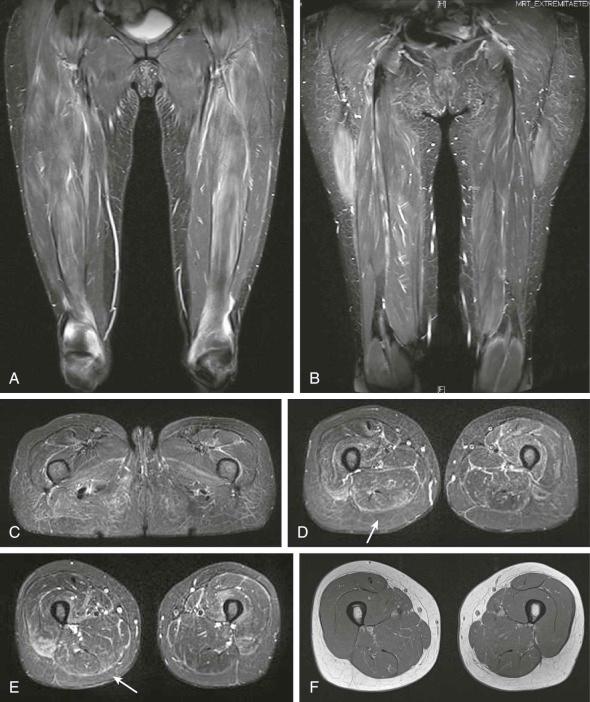
Myalgia is a very frequent symptom in MCTD, whereas frank myositis is less common. When present, it resembles entire features of PM (see Chapter 55 ). MRI of myositis in the acute phase presents with edema-like muscle signal abnormalities, which are best visualized in STIR images. The edema-like pattern may be diffuse, affecting more or less all muscles approximately to the same degree, or more focal, affecting single muscles. Sometimes a myofascial pattern is present. Muscle hyperintensities in STIR images precede the fatty degeneration and the decrease of muscle volume as displayed in T1-weighted images (see eFig. 54-3). Recurrent or persistent inflammatory activity results in the display of muscle hyperintensities on STIR images and fatty atrophy. The severity of muscle edema-like signal has been shown to correlate with the activity of the inflammatory disease, whereas the extent and severity of fatty atrophy may serve as a measure of damage in PM. Neither myonecrosis nor abscesses are found. Bilateral and symmetric affection of the pelvic and thigh musculature, especially of the quadriceps muscle, is typical, but small muscle involvement has been described, too. MRI is a helpful tool for assessment of the extent and number of lesions and is suited for therapy monitoring or locating a biopsy site in an area of active disease. In known MCTD, however, muscle biopsies are not necessarily required. The diagnosis of myositis may be assumed in MCTD patients with proximal muscle weakness, elevated muscle enzymes, and/or with an MRI pattern typical of PM.
Treatment depends entirely on the pattern of clinical involvement. For arthralgia and arthritis as well as constitutional symptoms, nonsteroidal anti-inflammatory agents are used, and, if needed, the combination with low-dose corticosteroid therapy has been shown to be effective. For arthritis, corticosteroid and antimalarial therapy is commonly administered, and methotrexate can be used in cases with an RA-like erosive course. Sclerodermatous features are sometimes irresponsive. Raynaud phenomenon may be addressed with iloprost or vasodilator therapy (calcium channel blockers). It is very important to monitor and treat the serious manifestations of MCTD, such as fibrosing alveolitis, pulmonary hypertension, and renal complications. For more severe disease, immunosuppressive drugs such as cyclophosphamide are used, followed by maintenance therapy with drugs such as azathioprine. New therapeutic regimens comprise methotrexate and B-cell inhibitors. For tumor necrosis factor α–blockers, the incidence of lupus-like syndrome has been described.
Nonspecific signs such as demineralization, soft tissue swelling, and extension deficit of the finger joints are the most common radiographic findings.
A mixture of the characteristic features of several rheumatic entities is typical but not very frequently found.
Polyarthritis ranges from nonerosive forms to a mutilating course; most often, it remains mildly erosive and sometimes exhibits an unusual involvement or distribution compared with RA.
Features of scleroderma comprise soft tissue calcifications, acral soft tissue atrophy with necrosis, and tuftal resorption.
Nonerosive deforming arthropathy and avascular necrosis of the femoral or humeral head as well as other epiphysis may be seen in patients with SLE features.
Polymyositis most often affects the thigh or pelvis, but it is much less common than simple myalgia.
In early disease, the most prominent finding on radiographs of the hands may be the soft tissue swelling. If present, more specific radiographic signs may appear slightly atypical, in part, because of the combination of features of two different connective tissue diseases and, in part, because of an unusual involvement or an irregular distribution of the polyarthritis compared with rheumatoid arthritis.
Prognosis is not always favorable. One should especially search for pulmonary hypertension with or without fibrosing alveolitis at regular follow-up evaluations and treat myositis efficiently.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here