Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Mitral stenosis (MS) is the most common form of rheumatic valve disease and produces significant disability, particularly in young and middle-aged adults. , Patients with severe MS usually develop fatigue, heart failure, atrial fibrillation, and thromboembolism. Of the many causes of MS, rheumatic mitral stenosis (RMS) remains the most common, usually presenting in patients between the ages 20 and 40 years, several years after an attack of rheumatic fever. In developed countries RMS is primarily seen in the immigrant population. Degenerative mitral valve stenosis (DMS), the other common form of MS, is more often seen in older adults, and its prevalence is increasing. Unlike RMS, DMS is typically not amenable to percutaneous mitral valve balloon valvuloplasty (MVBV).
Echocardiography is the diagnostic tool of choice to determine the presence, type, and severity of MS; to determine the best therapeutic options; and to follow patients with MS. The hemodynamics of MS has been reviewed with several associated problems such as pregnancy, in obese patients, and with resultant pulmonary hypertension.
MVBV and surgery are complementary interventions used at different times in the management of patients with MS. There are clear indications for surgical mitral valve repair or replacement in MS; however, surgery has been replaced by MVB) as the procedure of choice for managing severe, symptomatic rheumatic MS. The 2014 American Heart Association (AHA)/American College of Cardiology (ACC) and the 2017 European Society of Cardiology/European Association for Cardio-Thoracic Surgery ( Table 165.1 ) guidelines for the management of valvular heart disease delineate the central role of MVBV in the management of severe MS. The recent 2019 American Association for Thoracic Surgery/ACC/American Society of Echocardiography (ASE)/Society for Cardiovascular Angiography and Interventions/Society of Thoracic Surgeons Expert Consensus System of Care Document includes percutaneous mitral balloon commissurotomy as one of seven interventional procedures requiring care under a Comprehensive Valve Center.
| (Class I Indications) | Level of Evidence |
|---|---|
| 2014 ACC/AHA Guidelines for Interventions in Mitral Stenosis (7) | |
|
A |
|
B |
| 2017 ESC/EACTS Guidelines for Interventions in Mitral Stenosis (8) | |
|
B |
|
C |
|
C |
MVBV is most effective in patients with rheumatic MS, and echocardiography plays an essential role in determining MVBV suitability according to well-stablished scoring parameters. In patients with degenerative MS, other transcatheter procedures are being used, including the deployment of valves designed for transcatheter aortic valve replacement (TAVR) as valve in mitral anulus calcification (MAC) or valve-in-ring interventions. , A similar approach is being used in patients with mitral bioprosthesis stenosis. ,
This chapter describes the role of echocardiography in the management of MS with MVBV. Patient selection, intraprocedural guidance, detection and prevention of procedural complications, and evaluation of results and follow-up are discussed.
Proper medical, interventional, and surgical management of patients with MS requires characterization of the cause, stage, valve anatomy, valve hemodynamics, hemodynamic consequences, and determination of the presence and severity of symptoms. Candidates for MVBV have symptoms of heart failure, rheumatic valve changes with commissural fusion and diastolic doming of the mitral valve leaflets, and severe MS with a mitral valve area (MVA) of 1.5 cm 2 or less. Absence of more than mild mitral regurgitation (MR) and absence of left atrial (LA) thrombus are also prerequisites.
Native valve MS can be rheumatic, or nonrheumatic. Nonrheumatic causes include DMS with MAC, , radiation‐induced MS, and congenital MS. Rare causes of MS include LA myxoma, LA mases, amyloidosis, carcinoid syndrome, systemic lupus erythematosus, , endomyocardial fibroelastosis, and endocarditis. MS can also occur in the setting of prosthetic mitral valve dysfunction, which typically is not treatable by MVBV.
The first step in determining suitability for MVBV is to exclude nonrheumatic MS. Most of the nonrheumatic causes of MS have characteristic echocardiographic findings and are relatively easy to differentiate from rheumatic MS; these are not discussed here. However, differentiating rheumatic from degenerative MS is not always straightforward, and this distinction has important implications regarding eligibility for MVBV. Preprocedural cardiac computed tomography (CCT) is being increasingly used for the planning of valve in MAC with very promising results. Table 165.2 and Figs. 165.1 and 165.2 illustrate and summarize the main differences between rheumatic and degenerative MS.
| Rheumatic | Degenerative | |
|---|---|---|
| Age group | Younger | Older |
| History of rheumatic fever | Yes (not always) | No |
| Commissural fusion | Yes | No |
| Mitral annulus calcification | No (usually) | Yes |
| Extension of calcification to surrounding tissues | Uncommon | Common |
| Main leaflet thickening | Tips | Base |
| Valve geometry | Funnel shape | Tunnel shape |
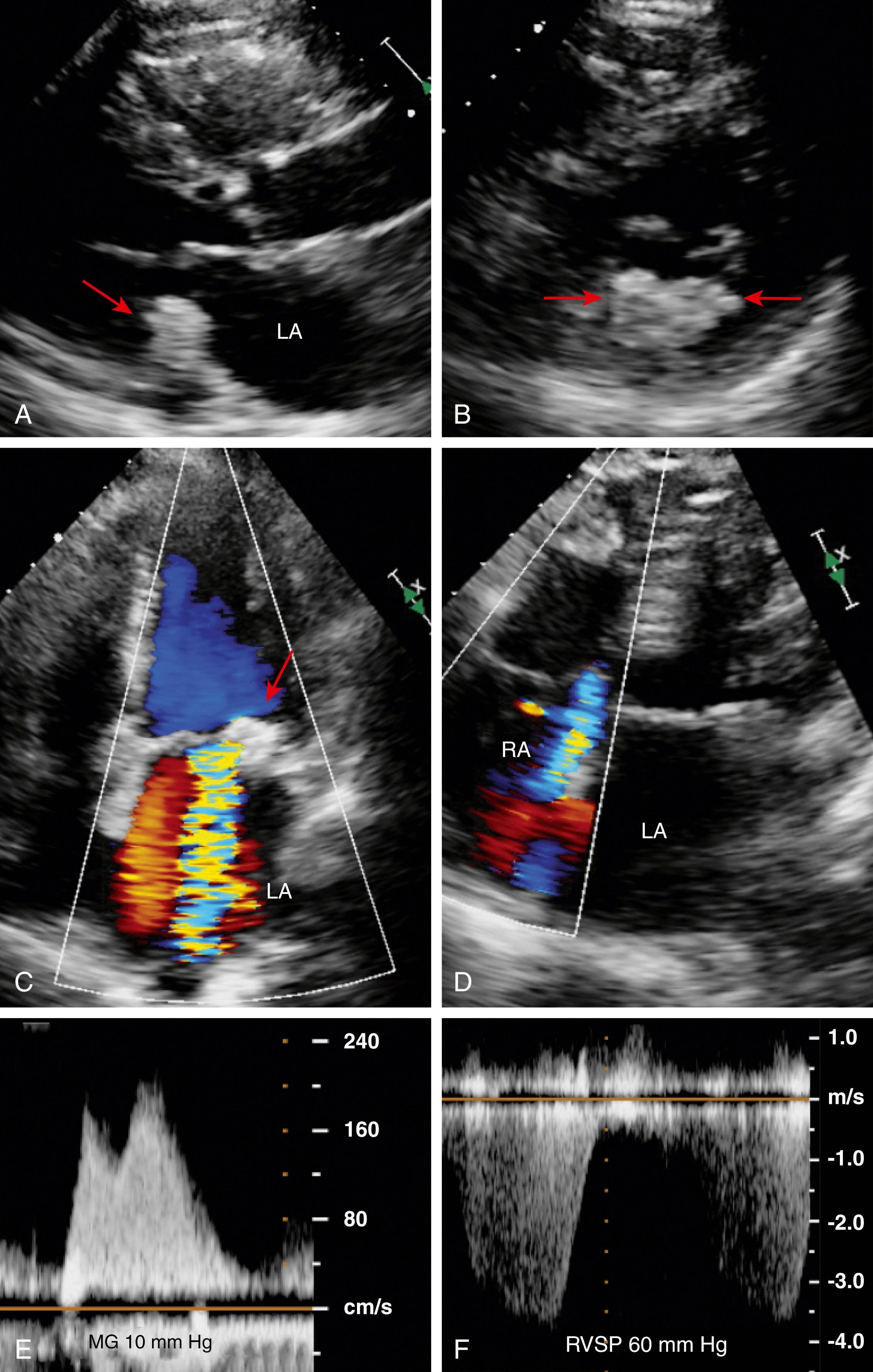
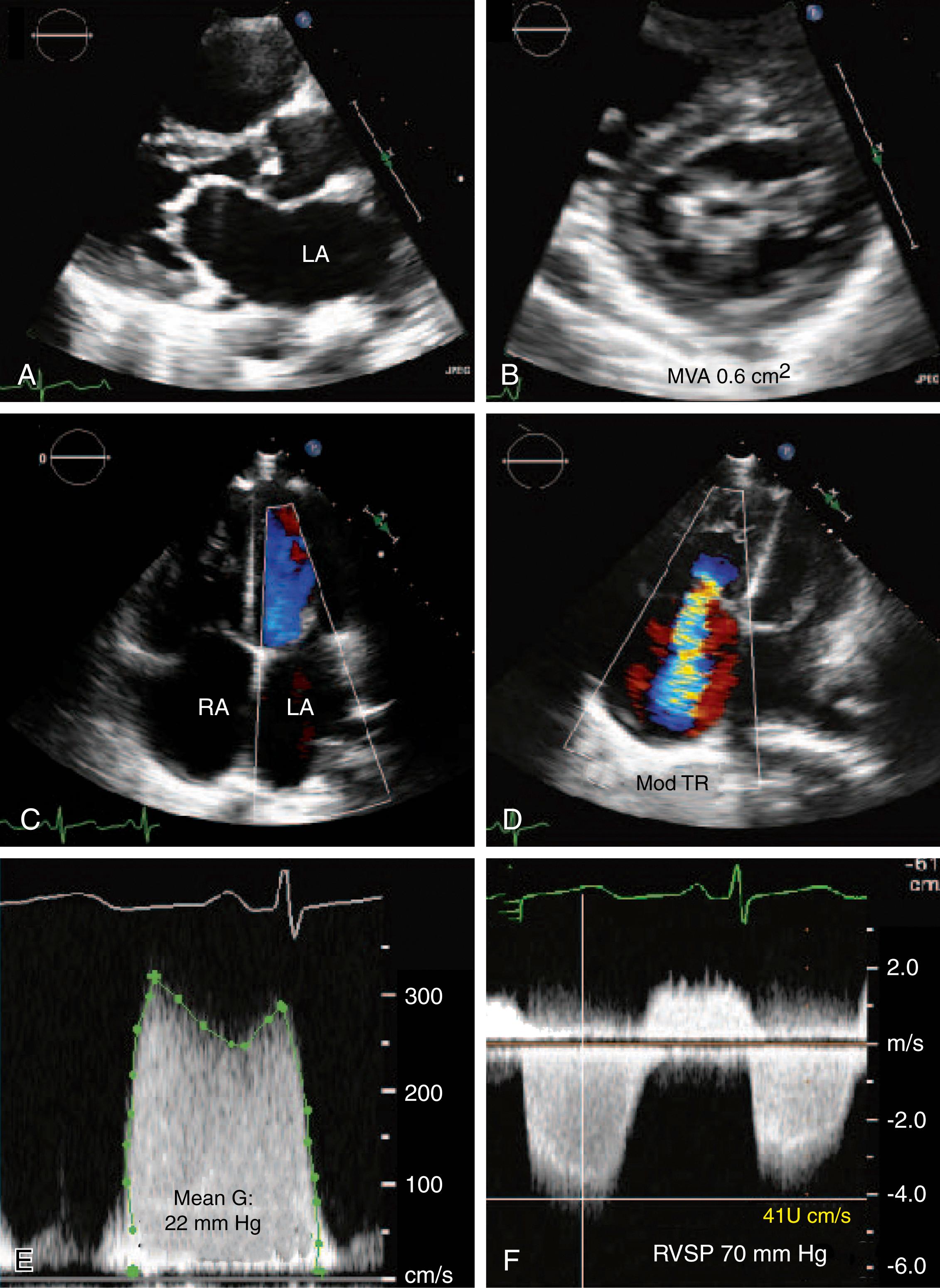
Candidates for MVBV have evidence of severe MS as described by the ASE guidelines for the assessment of valve stenosis. The following echocardiographic or Doppler indices of MS severity are required (see Fig. 165.2 ):
Mean mitral gradient from continuous-wave Doppler diastolic mitral flow. Mitral gradient, although reliably assessed by Doppler, is not the best marker of the severity of MS because it is dependent on the MVA as well as several other factors that influence transmitral flow rate, such as heart rate, cardiac output, and associated MR. Because of this, the 2014 AHA/ACC guidelines on valvular heart disease explicitly state that the gradient is an ancillary method of determining the severity of MS. Severe MS typically has a mean diastolic transmitral gradient of more than 5 to 10 mm Hg.
MVA planimetry using two-dimensional (2D) echocardiography of the mitral orifice has the advantage of being a direct measurement of MVA, and unlike other methods, it is not affected by flow conditions, cardiac chamber compliance, or associated valvular lesions. Severe MS is MVA of 1.5 cm 2 or less.
Pressure halftime (PHT) is defined as the time interval in milliseconds between the maximum mitral gradient in early diastole and the time point at which the gradient is half the maximum initial value. Severe MS is a diastolic PHT of 150 ms or greater.
Other markers of MS severity include increased LA volume and pulmonary hypertension (pulmonary artery systolic pressure ≥50 mm Hg).
The determination of severity may require exercise when the resting gradient does not meet the severity level or the patient appears to be symptomatic with activities. Exercise not only increases cardiac output but also decreases the diastolic filling time. Furthermore, some patients with MS may restrict their activities to avoid breathlessness, and exercise provides an objective assessment of hemodynamics as well as symptoms. Therefore, baseline measurement of mean mitral gradient and estimated pulmonary systolic pressure is compared with immediate postexercise measurements. The results are integrated with the presence of symptoms with exercise to determine the physiologic impact of the patient’s MS.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here